Analkarzinom
Anal cancer is relatively uncommon, accounting for less than 2% of large bowel malignancies. Most cases are squamous cell carcinoma on histology.
Epidemiology
It accounts for less than 2% of large bowel malignancies and 1-6% of anorectal tumors (~1.5% of all gastrointestinal tract malignancies in the United States ). It is commonly diagnosed between the ages of 45 and 75 years .
There may be a slight female predilection where its incidence has been reported to be approximately 0.5 per 100 000 in men and 1.0 per 100 000 in women . The incidence is thought to be rising over the years .
Clinical presentation
Approximately 45% of patients may present with bleeding per rectum. Around 30% of patients may have pain and/or a sensation of a mass.
Pathology
Anal carcinoma typically originates between the anorectal junction above and the anal verge below. The vast majority of anal canal cancers are squamous cell cancers. See WHO classification of anal canal tumors.
- ~85% squamous cell carcinoma
- ~10% adenocarcinoma
- ~5% made of rarer tumors (e.g. melanoma, small cell carcinoma, and metastatic disease)
Risk factors
Both male and female :
- HIV infection
- HPV infection
- strongly related to sexual activity
- in particular, anal receptive intercourse
- more than 90% of patients presenting with metastatic SCC have been reported with detectable HPV
- strongly related to sexual activity
- immunosuppression
- number of lifetime sexual partners, and receptive anal intercourse
- smoking
In females: previous in situ or invasive cervical, vulva, or vaginal cancer .
Lymphatic spread
- tumor above dentate line: mesorectal and internal iliac nodes
- tumor below dentate line: external iliac, inguinal, and deep inguinal nodes
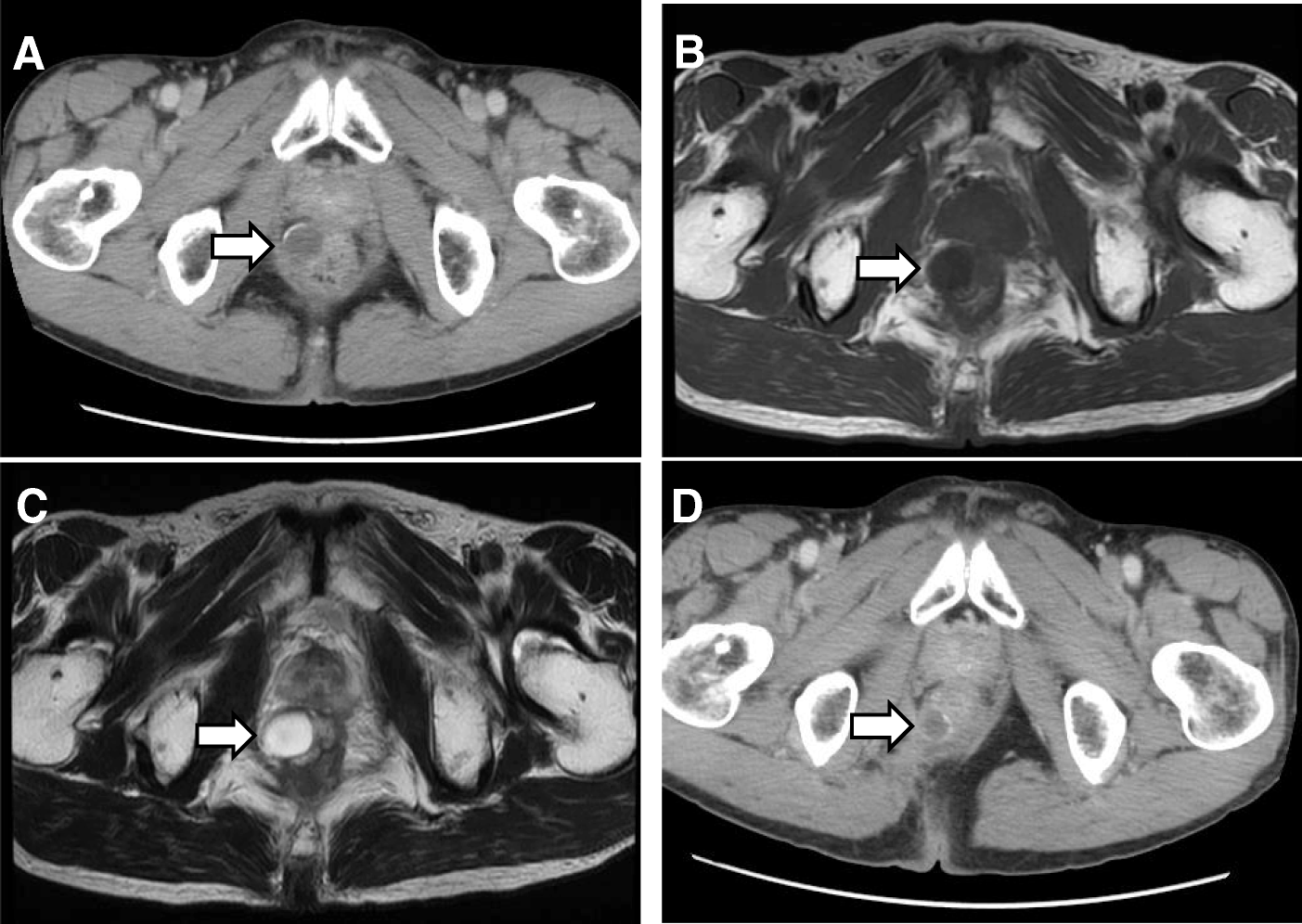
Radiographic features
Imaging performed before treatment provides an assessment of the extent of local disease and nodal involvement. Accurate delineation of the disease in relation to the rest of the perineal anatomy is of paramount importance in initial imaging assessment. The size of the tumor is also considered a critical prognostic factor (see staging of anal cancer) .
Ultrasound
Endoanal ultrasound can sometimes be used in locoregional staging , particularly for small superficial lesions (T1 stage) . Some authors suggest that endoanal ultrasound can accurately determine the depth of penetration of the carcinoma into the sphincter complex and can be used to accurately gauge the response of these tumors to chemoradiation therapy .
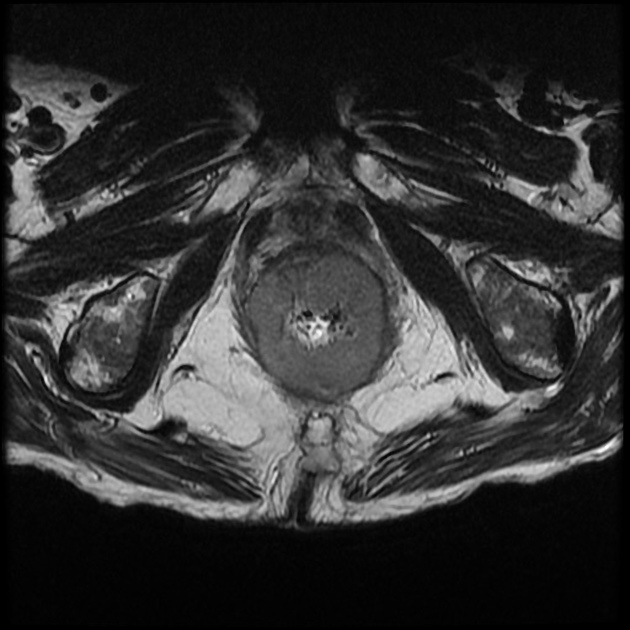
MRI
MRI is the modality of choice in the assessment of locoregional disease and is performed with a dedicated protocol: see MRI protocol for assessment of anal cancer.
Reported typical signal characteristics include :
- T1: primary and recurrent tumors are usually of low to intermediate signal intensity relative to skeletal muscle
- T2: primary and recurrent tumors are generally of high signal intensity relative to skeletal muscle
Nodal metastases have a signal intensity similar to that of the primary tumor.
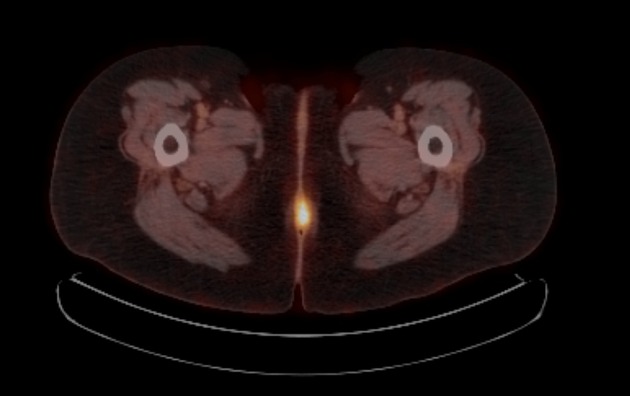
PET-CT
F-18 FDG PET-CT has been now used as an auxiliary imaging modality for staging in many countries. It has a high sensitivity for detection of both the primary lesion and the regional node involvement , and it alters the initial staging frequently .
Treatment and prognosis
Treatment is often with a combination of chemotherapy and radiotherapy (often given concurrently) and is usually curative in lower stages.
- approximately 50-60% are thought to present with T1 to T2 lesions carrying a 5-year survival of 80-90% .
Some authors suggest a benefit of a salvage abdominoperineal resection (APR) for those patients with failed chemoradiation .
Siehe auch:
- MRI protocol for assessment of anal cancer
- Adenokarzinom Analdrüse
- Analrand-Neoplasien
- staging of anal cancer
und weiter:

 Assoziationen und Differentialdiagnosen zu Analkarzinom:
Assoziationen und Differentialdiagnosen zu Analkarzinom: