angioinvasive aspergillosis








Angioinvasive aspergillosis is the most severe and aggressive form of invasive aspergillosis. It is a life-threatening condition that requires prompt treatment. Fortunately, it is not seen in the general population and only occurs in profoundly immunocompromised patients.
Epidemiology
Angioinvasive aspergillosis is seen in patients who are profoundly immunosuppressed, with underlying causes for this immunodeficiency that include :
- prolonged high dose corticosteroids
- neutropenia (absolute neutrophil count <500/μL)
- graft-vs-host disease after allogeneic bone marrow transplantation
- end-stage AIDS
Infection with Aspergillus spp occurs in up to 10% of patients who received allogeneic stem cell transplantation . Aspergillus, unlike other pulmonary infections, can infect the lung at any stage following stem cell transfusion .
Clinical presentation
Clinical presentation is non-specific and thus in the correct patient population requires a low threshold for investigation. Typical symptoms include cough and fever. Pleuritic chest pain and hemoptysis may also be present .
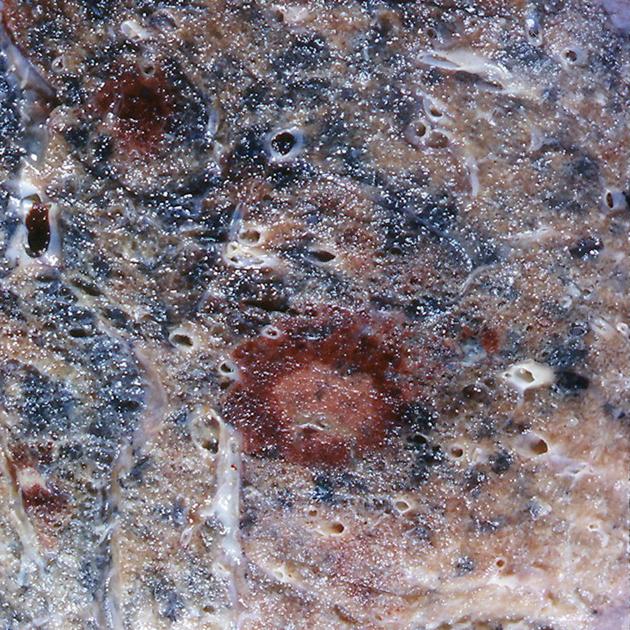
Pathology
Spores of a variety of Aspergillus spp are inhaled and begin to proliferate in the alveoli. The hyphae are able to invade pulmonary arteries resulting in pulmonary necrosis and hemorrhage . They may also gain access to the systemic circulation and are haematologically disseminated to the kidneys, gastrointestinal tract, and the central nervous system. Systemic dissemination occurs in 25-50% of cases .
If the neutrophil count recovers (in patients where neutropenia is the cause of the immunosuppression), the central necrotic area of lung demarcates, shrinks and separates from the adjacent viable tissue. It is this separation that creates the air crescent sign .
Radiographic features
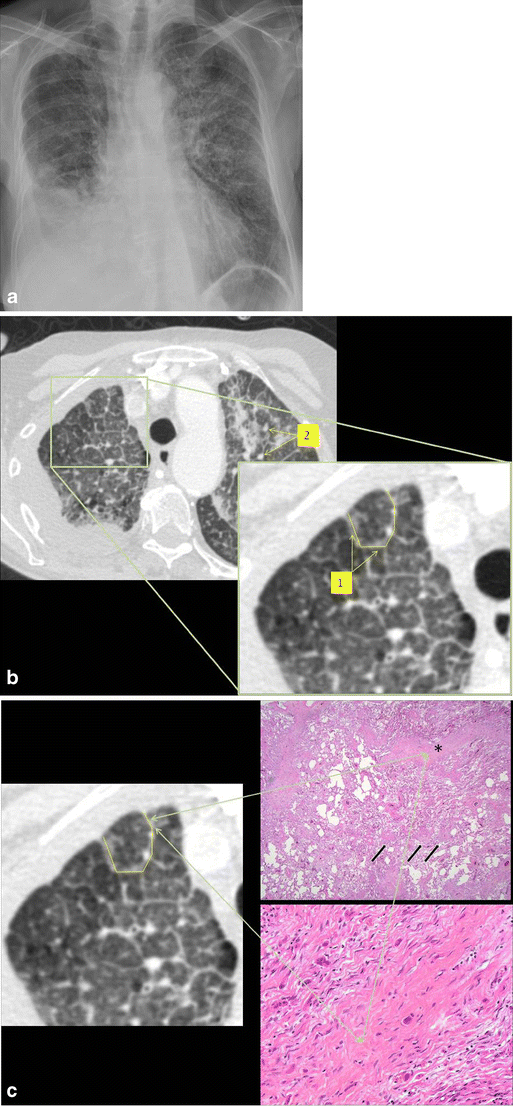
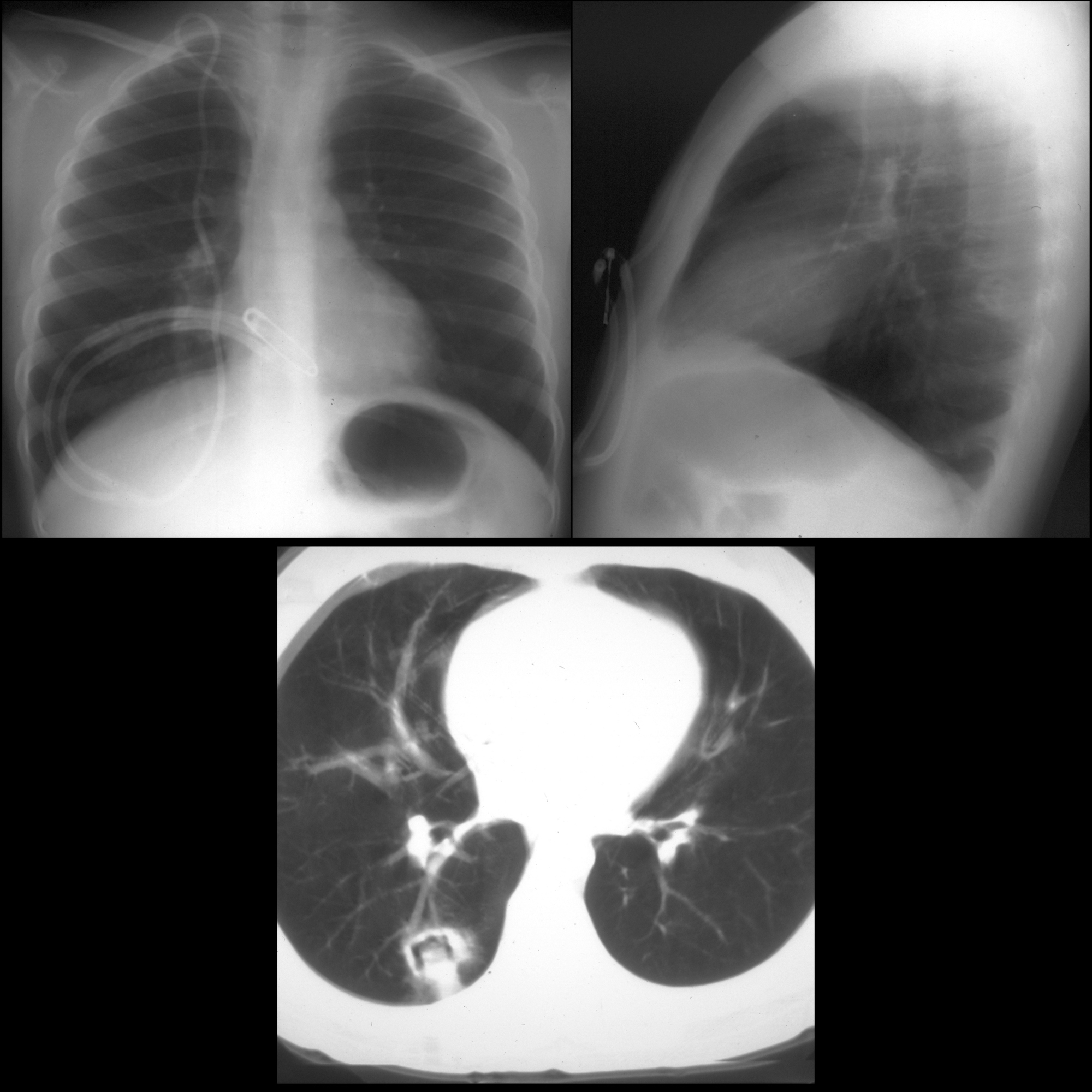
Plain radiograph
Typical appearances are those of solitary or multiple pulmonary nodules/masses. Wedge-like areas of ill-defined opacities may also be seen most likely representing infarcts due to the invasion of proximal pulmonary vessels .
An air crescent may be visible when recovery commences, although it is seen earlier on CT.
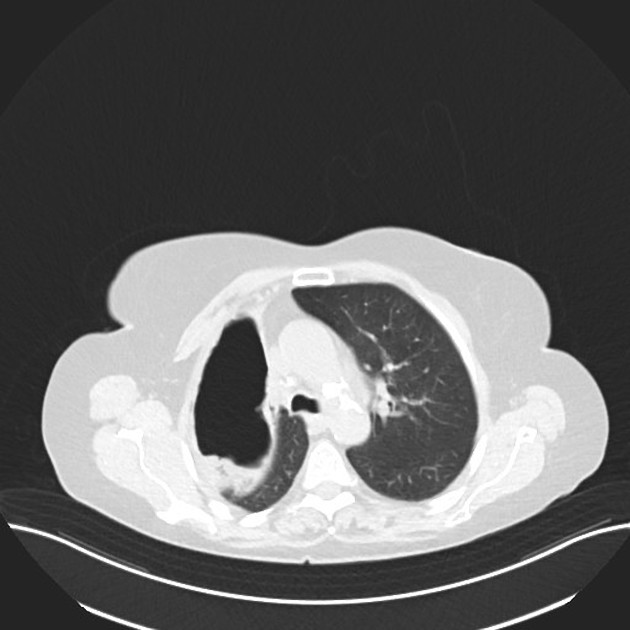
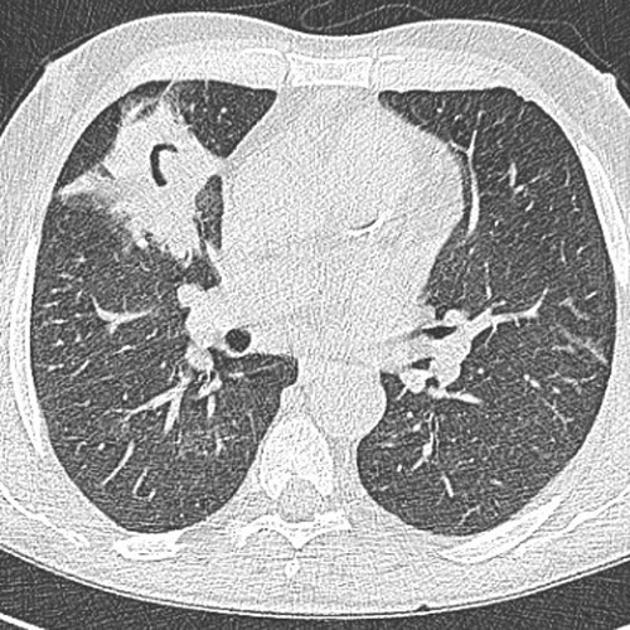
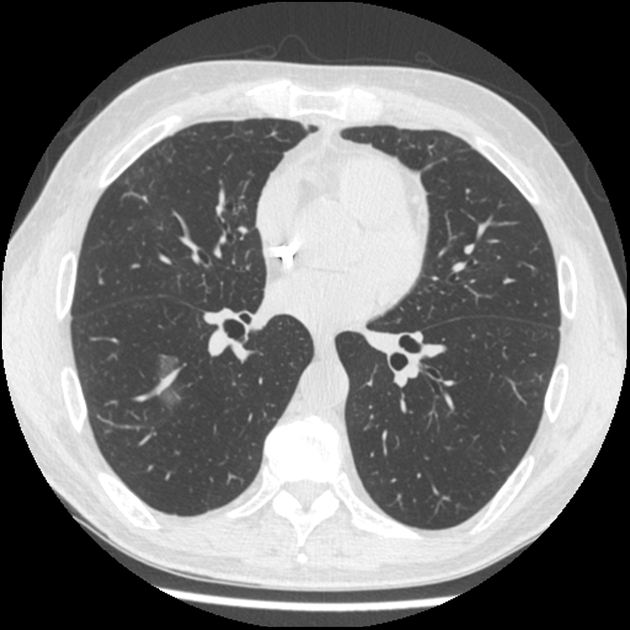
CT
As on plain radiography, CT findings demonstrate solitary or multiple pulmonary nodules/masses. A halo of hemorrhage may be seen around the nodule as a result of invasion into pulmonary vessels and is seen as an area of ground-glass opacity . A reverse halo may also be encountered . In the correct clinical setting, these findings are strongly suggestive of angioinvasive aspergillosis and warrant institution of appropriate therapy until proven otherwise (see below).
Peripheral wedge-like areas of consolidation representing hemorrhagic pulmonary infarcts are seen better on CT than plain films . Direct invasion into the adjacent chest wall or mediastinal structures may be seen in advanced cases .
Eventually, if recovery occurs, the central necrotic lung separates away from surrounding parenchyma, forming an air crescent. This typically occurs 2-3 weeks after treatment . Cavitation may also occur.
Lymph node enlargement and pleural effusions are not usually seen .
Treatment and prognosis
The mainstay of treatment is intravenous amphotericin B. If the patient recovers, resection of the residual mass may be required .
Prognosis is generally poor, although early diagnosis and treatment may result in recovery .
Differential diagnosis
In the correct clinical setting, the presence of new nodules with ground-glass halo or reversed halo (atoll) sign is strongly suggestive of the diagnosis of angioinvasive aspergillosis, and treatment is usually initiated, without recourse to biopsy.
Other entities to be considered if demographics, presentation, or imaging is atypical include:
- other types of pulmonary infection
- pulmonary hemorrhage
- pulmonary metastases
- other causes of the air crescent sign
- other causes of the reversed halo sign
Siehe auch:
- Milchglasverschattungen
- Lungenblutung
- Luftsichelzeichen
- Lungenmetastasen
- pulmonary infection
- invasive aspergillosis
- aspergillus
- pulmonale Aspergillose
- AIDS
- airway invasive aspergillosis
- invasive pulmonale Aspergillose
- halo
- multiple Lungenherde
- masses
- air crescent
und weiter:
- aspergillosis
- obstructive bronchopulmonary aspergillosis
- feeding vessel sign
- Pilzpneumonie
- differential of an air crescent sign
- semi-invasive aspergillosis
- Halozeichen Lunge
- halo sign : chest
- Pneumocystis jiroveci Pneumonie
- superior vena cava thrombosis and haemorrhagic mediastinitis as manifestations of angioinvasive aspergillosis
- pulmonale Pilzinfektionen
- Thorax Onlinekurs
- chronic necrotising pulmonary aspergillosis

 Assoziationen und Differentialdiagnosen zu angioinvasive pulmonale Aspergillose:
Assoziationen und Differentialdiagnosen zu angioinvasive pulmonale Aspergillose: