Herpesenzephalitis


Herpes simplex (HSV) encephalitis is the most common cause of fatal sporadic fulminant necrotizing viral encephalitis and has characteristic imaging findings.
Two subtypes are recognized which differ in demographics, virus, and pattern of involvement. They are :
This article concerns itself with the latter. For a discussion of the former, please refer to the article neonatal herpes simplex encephalitis.
Epidemiology
Childhood and adult herpes encephalitis are usually due to HSV-1 (90%) with the rest due to HSV-2 . There is no particular age, sex, or seasonal predilection.
Clinical presentation
The presentation is unfortunately relatively non-specific consisting of fever, headaches, focal neurological deficits, seizures, and altered or decreased level of consciousness.
Diagnosis is established with PCR of CSF, although the combination of the clinical scenario, CSF demonstrating pleocytosis and elevated protein, and appropriate imaging is usually highly suggestive and permits commencement of treatment.
Pathology
HSV is an obligatory intracellular virus that enters via infecting nasopharyngeal cells into the sensory branch of lingual nerve then ascends to trigeminal ganglion and remains latent for a lifetime. Reactivation in the case of immunosuppression, trauma, or other stresses can result in fulminant hemorrhagic necrotizing encephalitis. HSV has a high affinity for limbic systems with bilateral but asymmetric involvement.
Microscopic appearance
Perivascular cuffs of lymphocytes, large inclusions in neurons and glial cells called "owl's eye", neuronophagia, necrosis and hemorrhage are characteristics of herpes simplex encephalitis.
Radiographic features
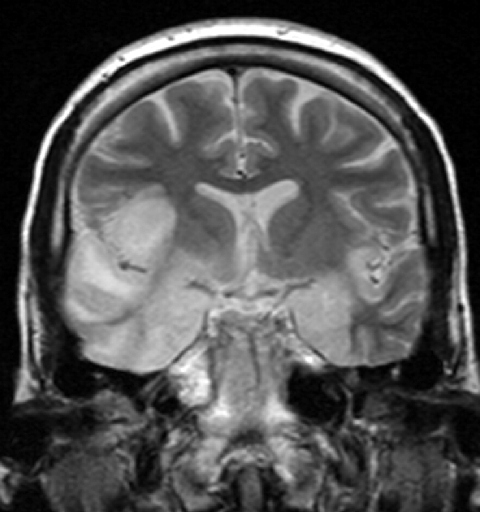
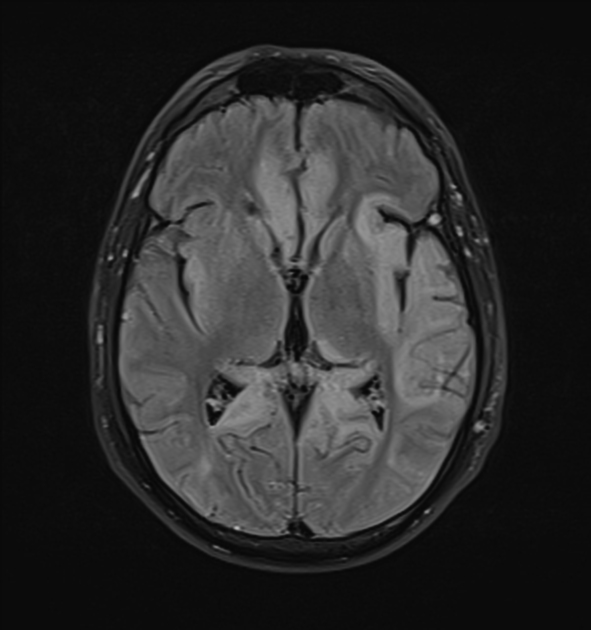
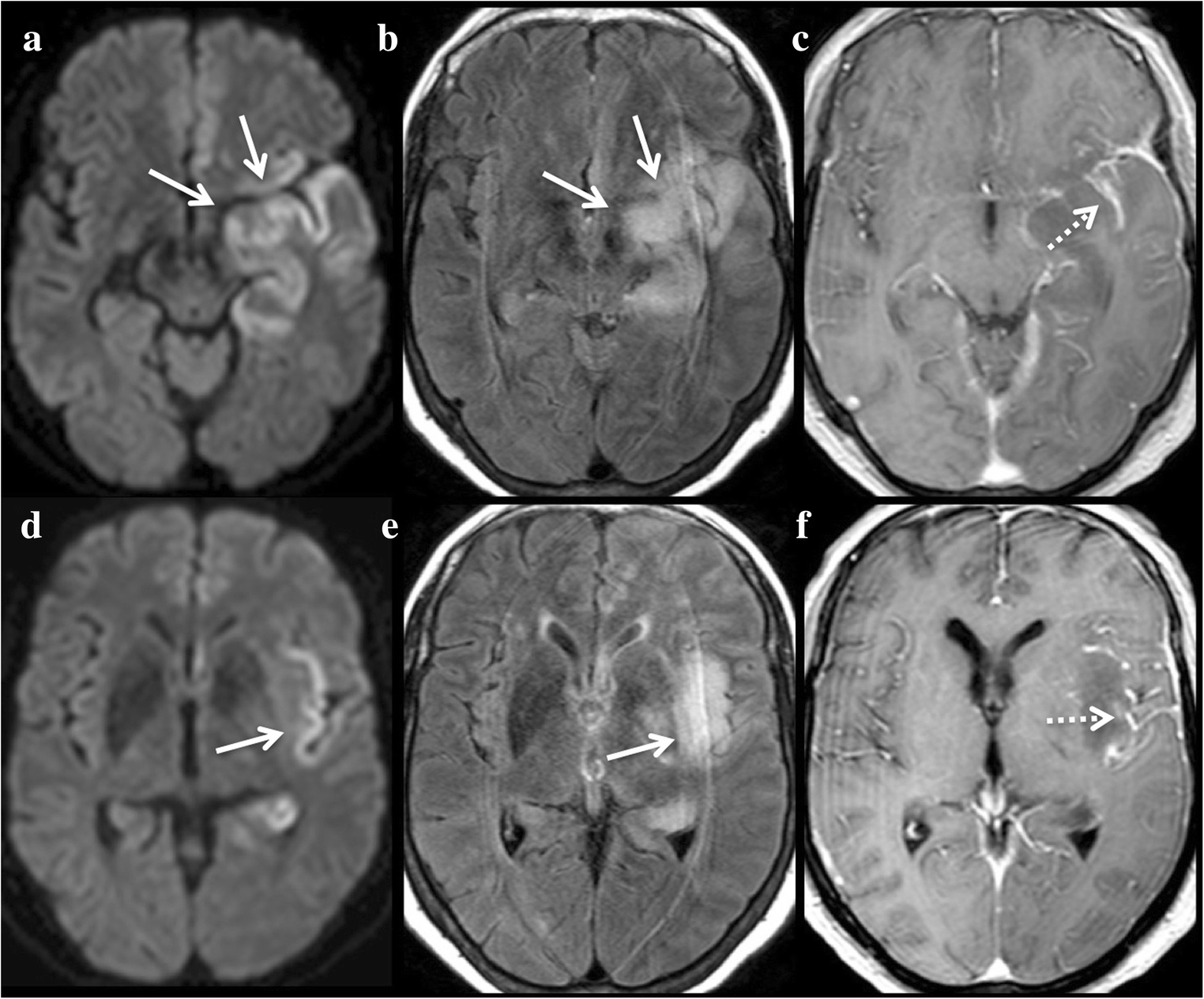
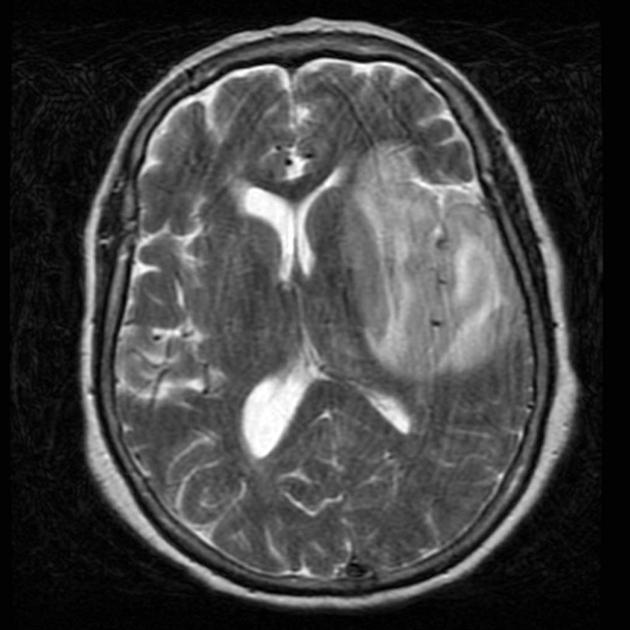
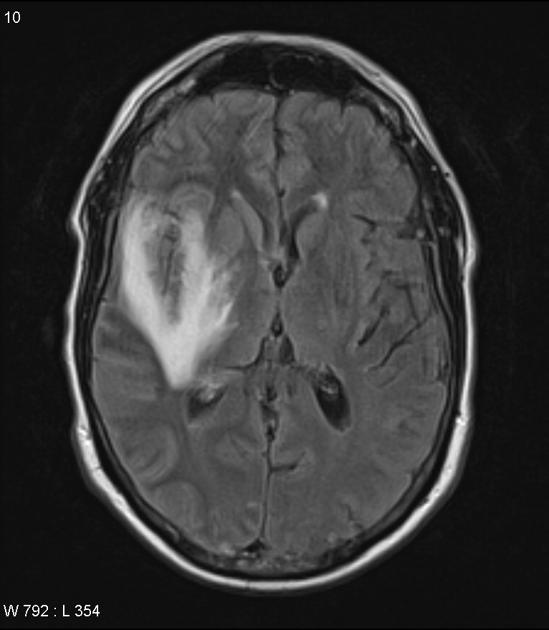
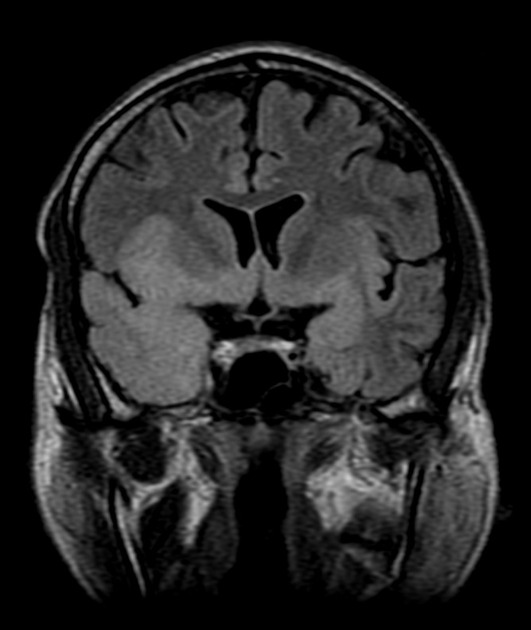
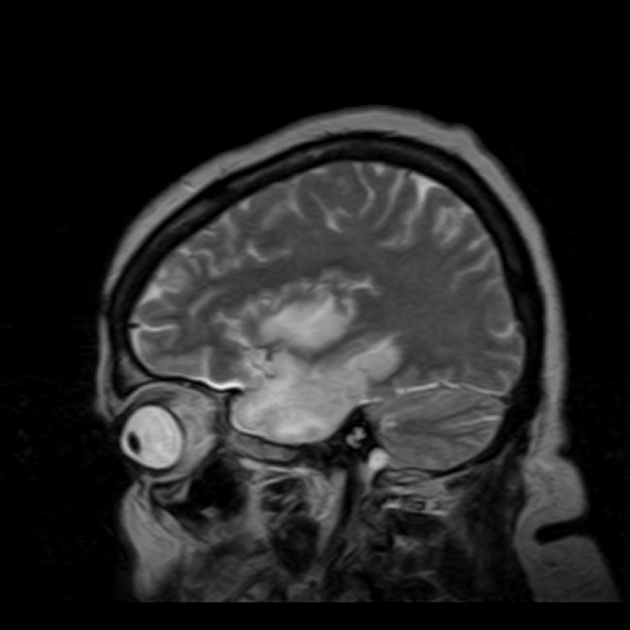
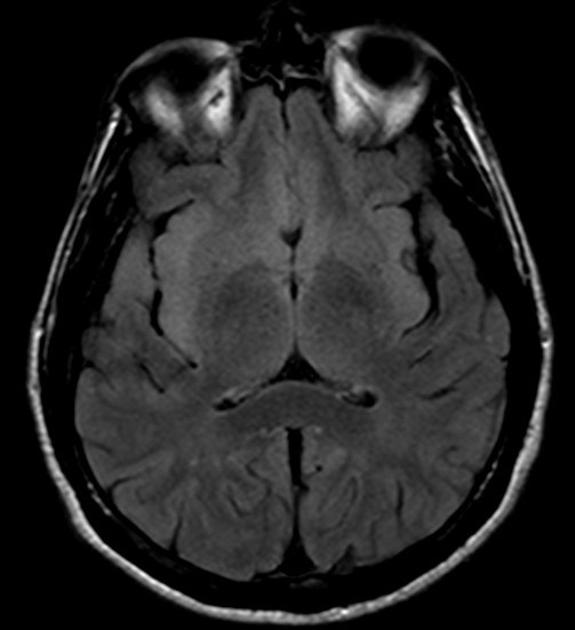
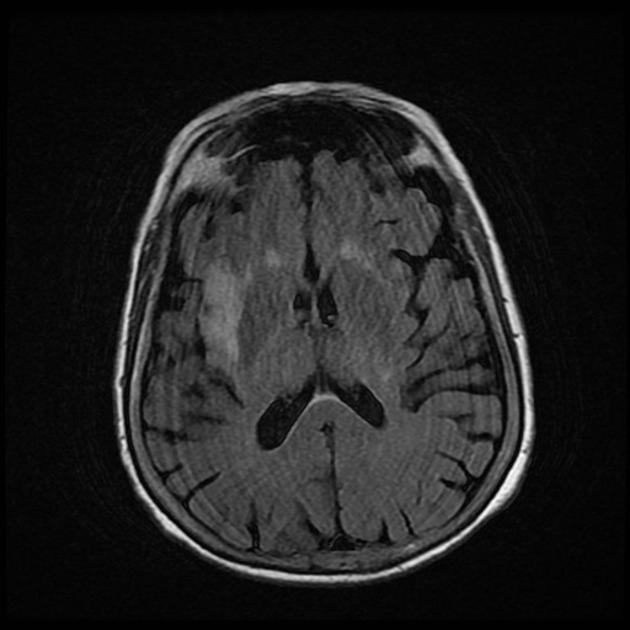
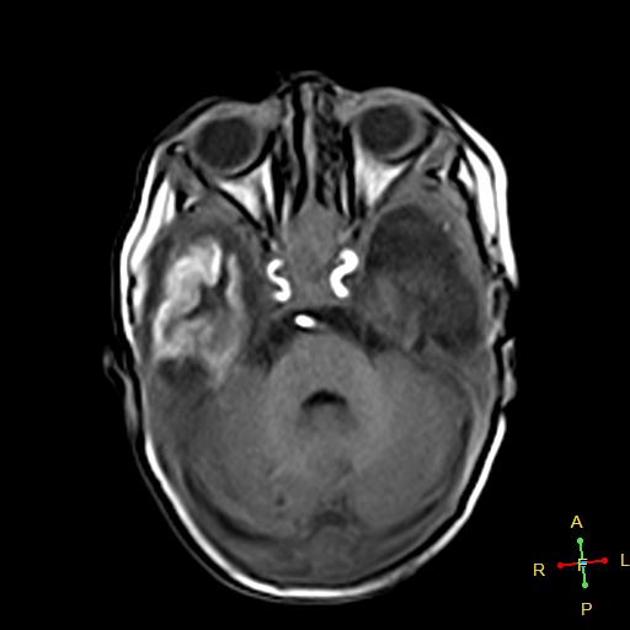
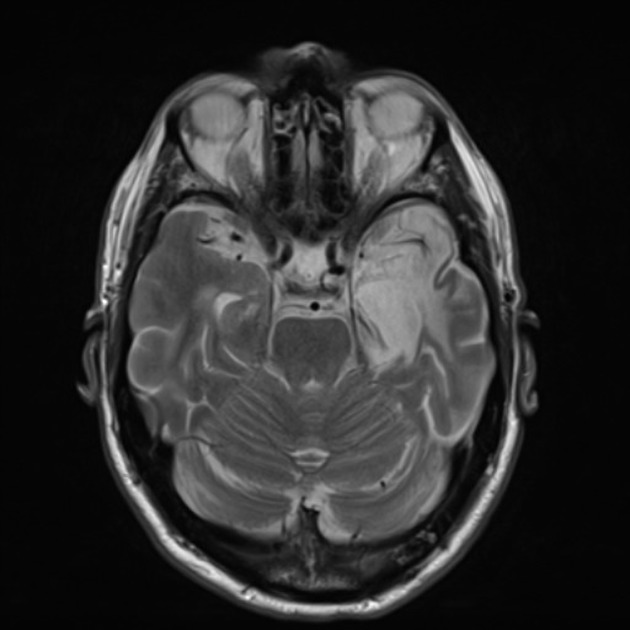
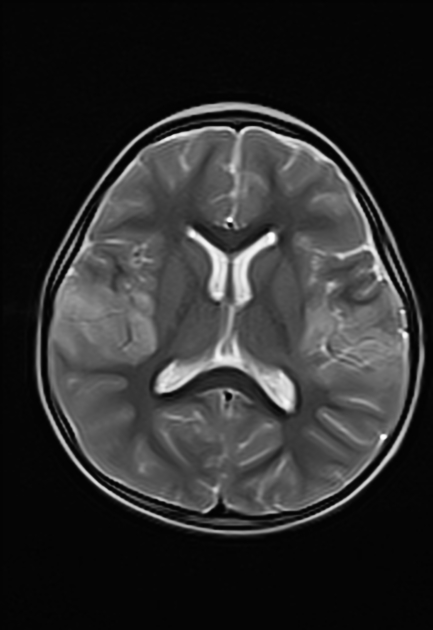
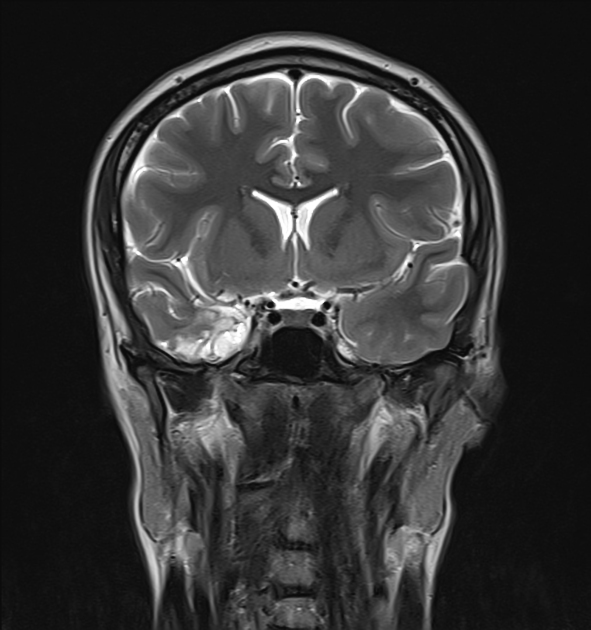
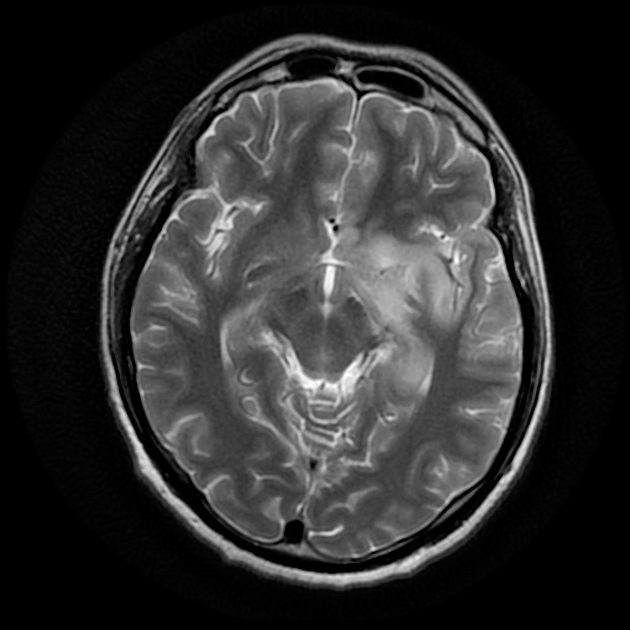
In the immunocompetent adult patient, the pattern is quite typical and manifests as a bilateral asymmetrical involvement of the limbic system, medial temporal lobes, insular cortices and inferolateral frontal lobes. The basal ganglia are typically spared, helping to distinguish it from a middle cerebral artery infarct.
Extralimbic involvement is more prevalent in children than in adults, seen most commonly in the parietal lobe, with sparing of basal ganglia. Eventually, it results in marked cystic encephalomalacia and volume loss in affected areas.
In immunocompromised patients, involvement can be more diffuse, and more likely to involve the brainstem .
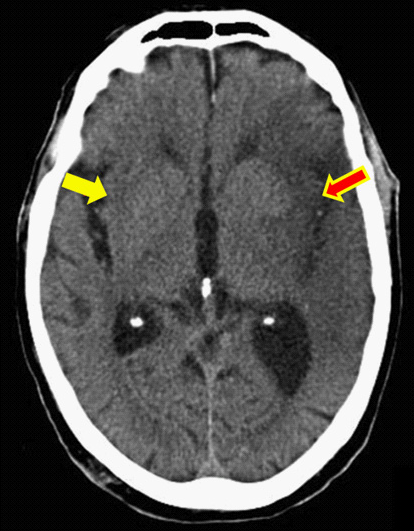
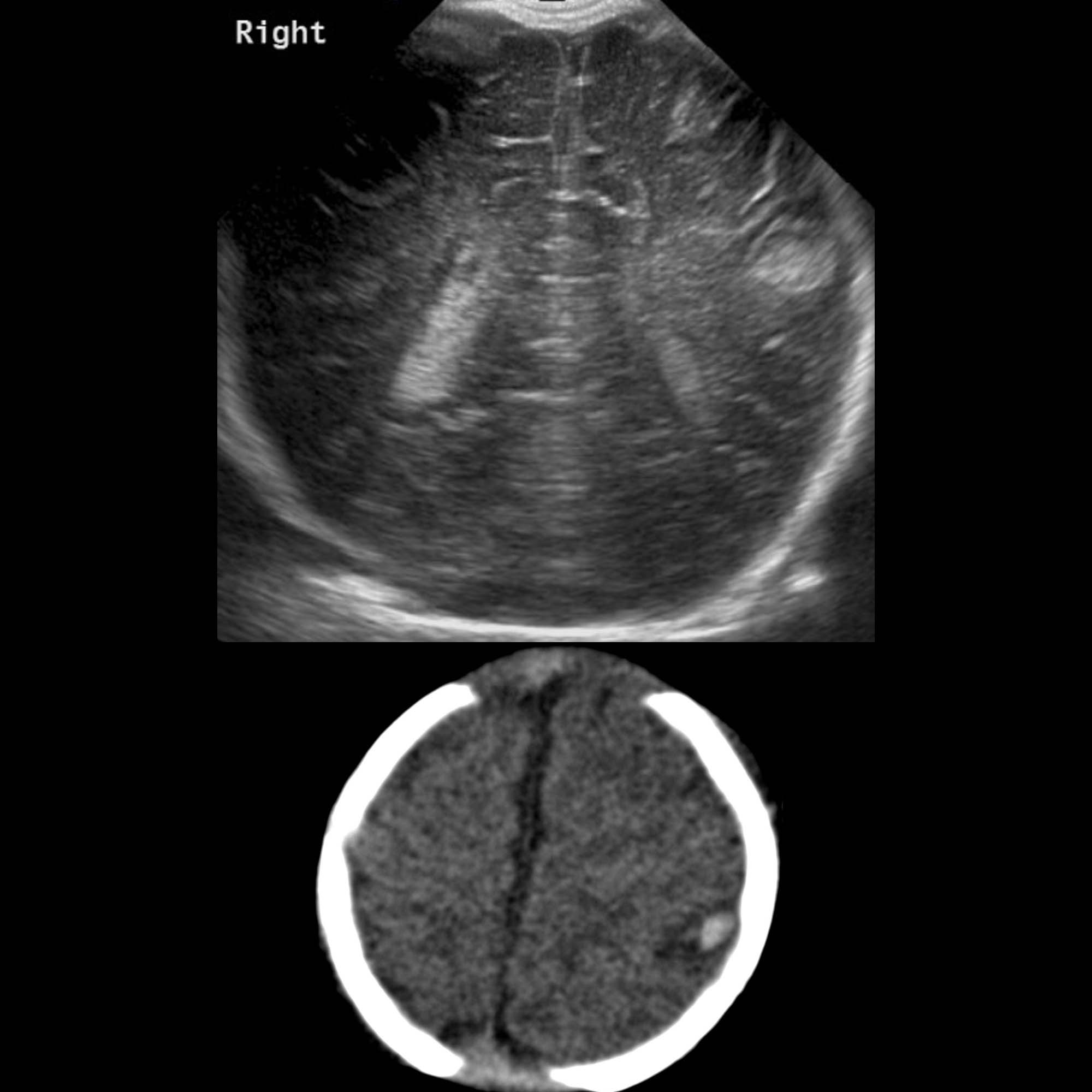
CT
Early diagnosis is difficult, and a 'normal' scan should not dissuade from the diagnosis. If findings are present, they typically consist of subtle low density within the anterior and medial parts of the temporal lobe and the island of Reil (insular cortex) . If scanned later then the changes may become more apparent and even progress to hemorrhage.
Contrast enhancement is uncommon during the first week of the disease. After that, a patchy low-level enhancement may be seen .
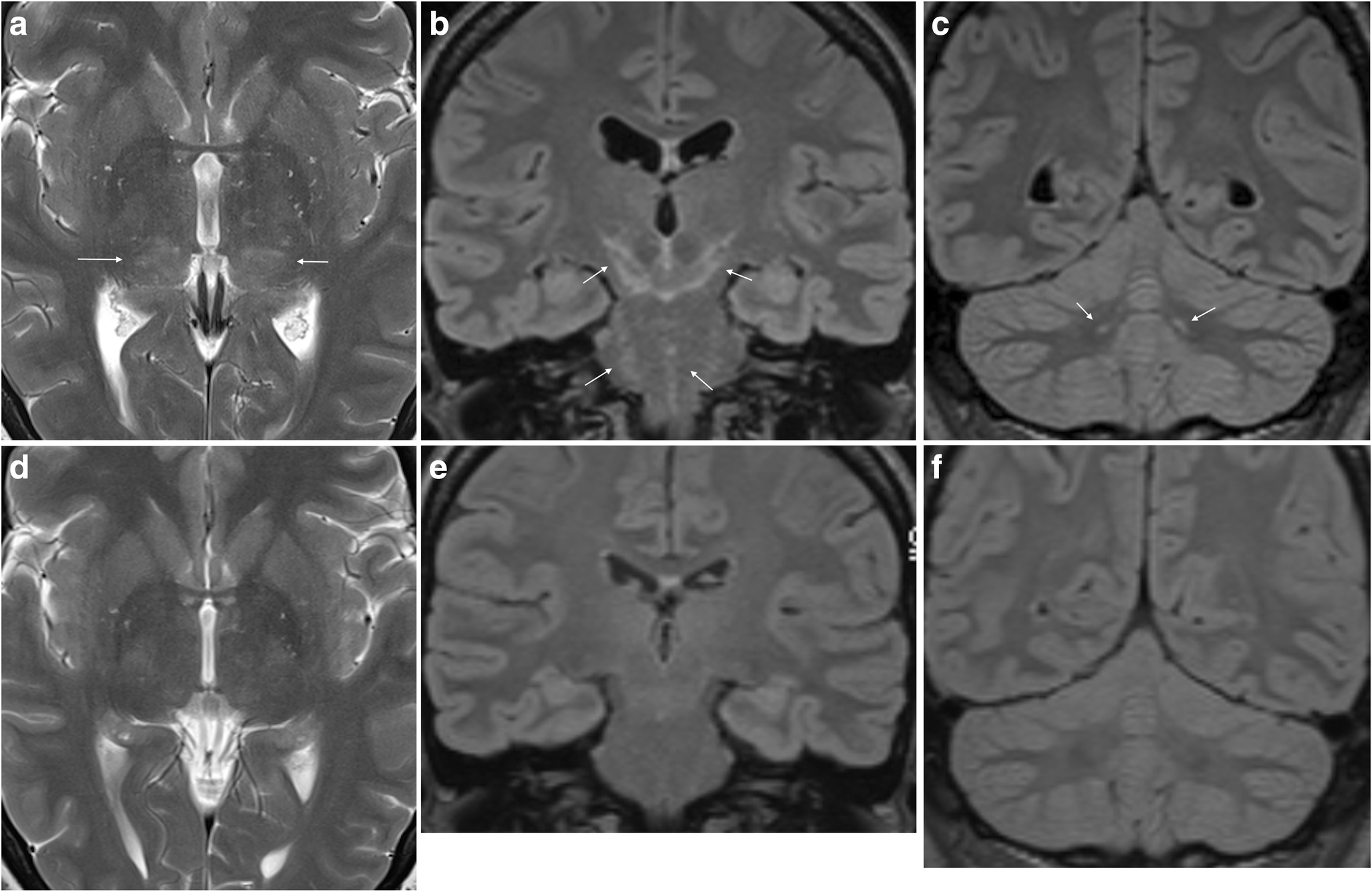
MRI
Affected areas, however, have a similar appearance regarding signal characteristics:
- T1
- may show general edema in the affected region
- if complicated by subacute hemorrhage there may be areas of hyperintense signal
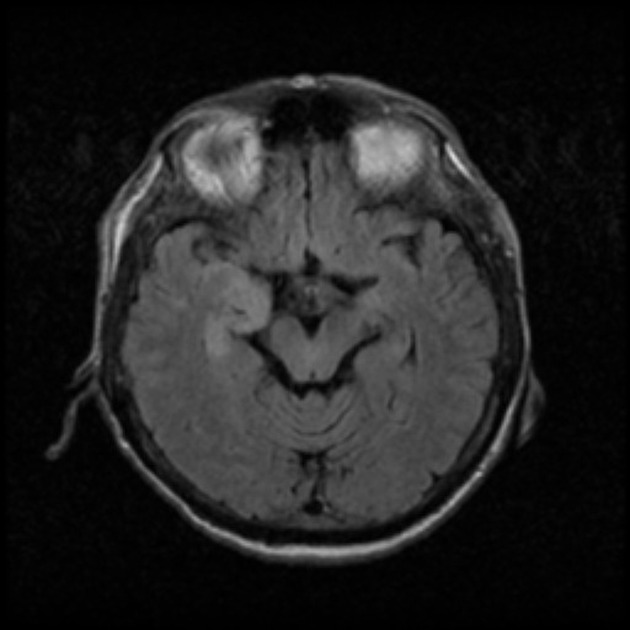
- T1 C+ (Gd)
- enhancement is usually absent early in the disease
- enhancement occurs later and is variable in pattern
- gyral enhancement
- leptomeningeal enhancement
- ring enhancement
- diffuse enhancement
- T2
- hyperintensity of affected white matter and cortex
- more established hemorrhagic components may be hypointense
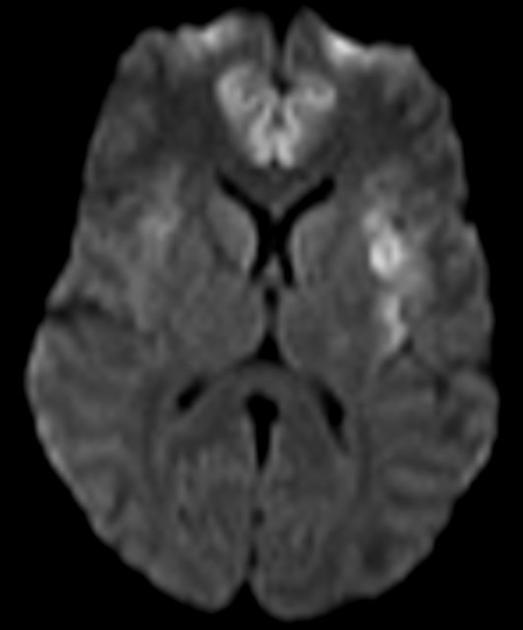
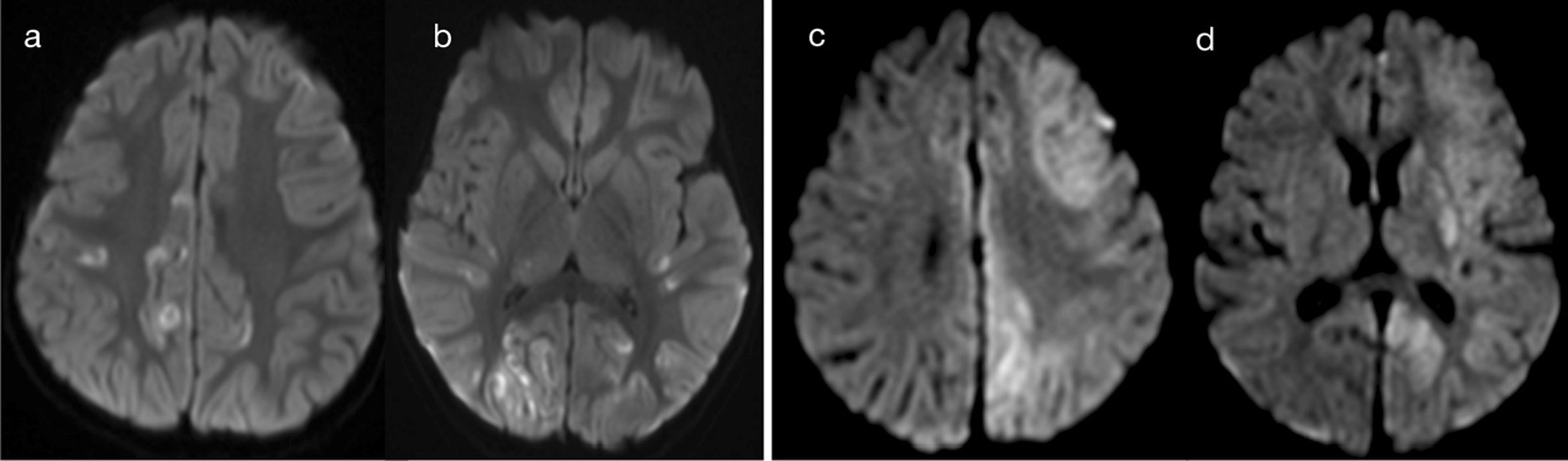
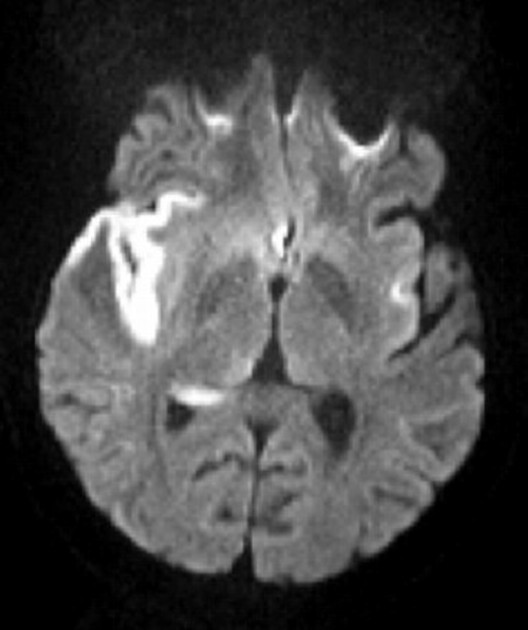
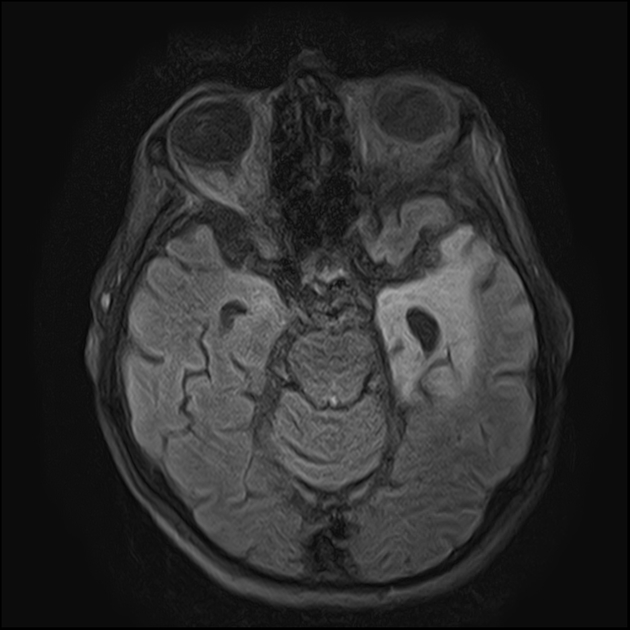
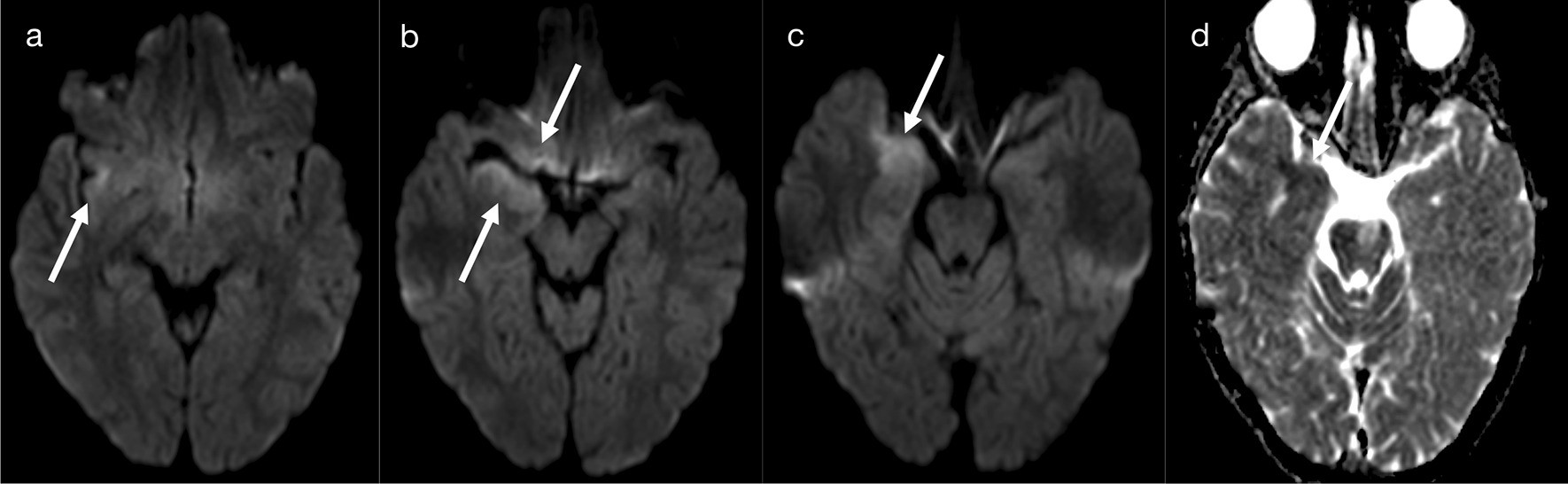
- DWI/ADC
- more sensitive than T2 weighted images
- restricted diffusion is common due to cytotoxic edema
- restricted diffusion is less intense compared to infarction
- beware of T2 shine through due to vasogenic edema
- GRE/SWI: may demonstrate blooming if hemorrhagic (rare in neonates, common in older patients)
Treatment and prognosis
Treatment is with intravenous antivirals (e.g. acyclovir), and if appropriate, antiepileptics and agents to reduce intracranial pressure.
Mortality ranges dramatically depending on how early treatment is instituted. Even in patients who are young and otherwise well, and only lethargic still have a mortality of 25%. Older patients or those comatose at the time treatment is started invariably have a much poorer outcome . Overall mortality is over 70% with only 2.5% of affected patients every fully recovering .
Differential diagnosis
General imaging differential considerations include:
- limbic encephalitis
- gliomatosis cerebri
- status epilepticus
- middle cerebral artery (MCA) infarction: typically involves the basal ganglia
- trauma
- viral encephalitides: many can have very similar appearances and are difficult to separate clinically, and the diagnosis usually requires PCR
- neurosyphilis
Siehe auch:
- Gliomatosis cerebri
- Enzephalitis
- Limbische Enzephalitis
- Virusenzephalitis
- neonatal herpes simplex encephalitis
- encephalitis due to herpesvirus family
- Herpesenzephalitis bei Erwachsenen
- bilateral temporal T2 hyperintensity
- MCA territory infarcts
und weiter:
- hyperdenses Gefäßzeichen
- hyperdense Media
- Oligodendrogliom
- Dysembryoplastischer neuroepithelialer Tumor
- diffusionsgewichtete Bildgebung
- Temporallappenepilepsie
- in utero herpes simplex infection
- human herpesvirus 6 encephalitis
- white matter changes in HIV
- Japanische Enzephalitis
- Herpes Simplex Uveitis
- long term herpes encephalitis sequelae
- neuroradiologisches Curriculum
- Rhombenzephalitis
- pädiatrische zerebrale Infektionen
- Atrophie Inselregion

 Assoziationen und Differentialdiagnosen zu Herpesenzephalitis:
Assoziationen und Differentialdiagnosen zu Herpesenzephalitis: