inverted papilloma
Inverted papillomas are a type of Schneiderian papilloma, representing an uncommon sinonasal tumor that mostly affects middle-aged men. On imaging, they classically demonstrate a convoluted cerebriform pattern seen on both T2 and contrast-enhanced T1 weighted MRI images.
Terminology
The term inverted papilloma is also used to describe an urothelial lesion. For a discussion of that entity, please refer to inverted papilloma of the urinary tract .
Epidemiology
Inverted papillomas account for approximately 0.5-4.0% of all nasal tumors and are most frequently seen in patients 40-60 years of age . There is a significant predilection for males (M:F ratio of ~3-5:1) .
Clinical presentation
The presentation can be similar to other sinonasal masses, with nasal obstruction, sinus pain, and epistaxis.
Pathology
Macroscopic appearance
Macroscopically inverted papillomas appear as irregular polypoid masses of variable consistency, pink in color, with a tendency to bleed .
Histology
Histology is that of ribbons of respiratory epithelium enclosed by basement membrane which grows into the subjacent stroma (thus with an inverted pattern) with characteristic micro-mucous cysts . Approximately 20% demonstrate some keratinization, and 10% dysplasia .
Location
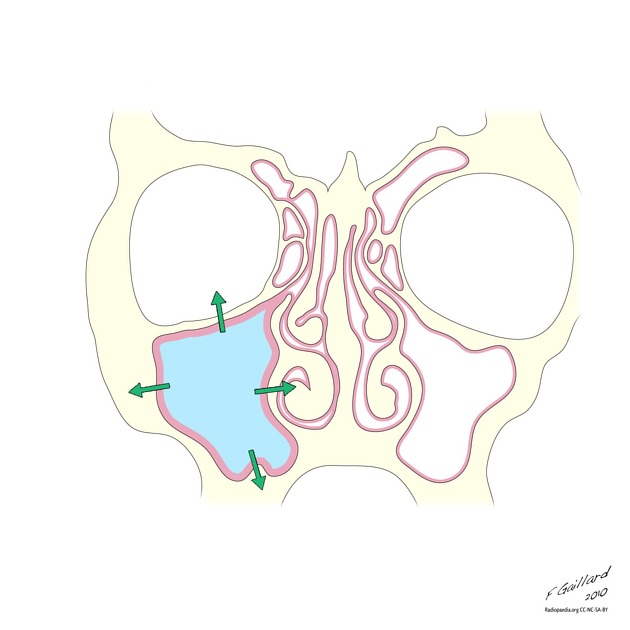
Inverted papillomas most commonly occur on the lateral wall of the nasal cavity, most frequently related to the middle turbinate/middle meatus and maxillary ostium, although they are seen elsewhere in the nasal passage. As the mass enlarges it results in bony remodeling and resorption and often extends into the maxillary antrum .
Due to the location, impairment of normal drainage of the maxillary antrum is common, although mucocele formation is rare .
Malignant transformation
Malignant transformation occurs in a variety of histologies, including keratinizing and non-keratinizing squamous cell carcinoma (by far the most common, seen in ~10% of cases) as well as much less frequently other malignant histologies including mucoepidermoid carcinoma, verrucous carcinoma, and adenocarcinoma . Tumors may be either synchronous or metachronous .
Radiographic features
Plain radiograph
Plain film no longer plays a significant role in the assessment of sinonasal disease. If obtained, the most common finding is that of a nasal mass with associated opacification of the adjacent maxillary antrum .
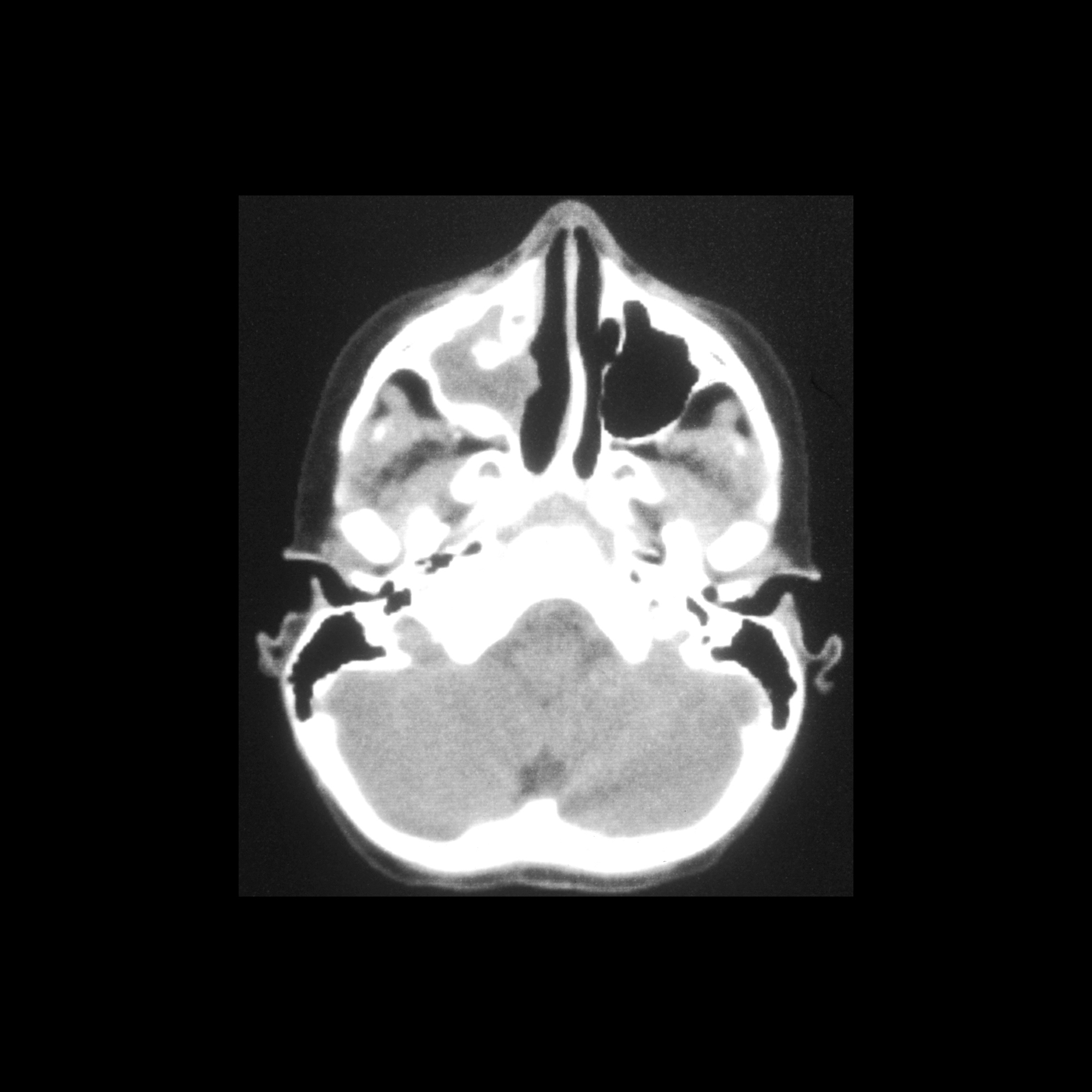
CT
CT features are mostly nonspecific, demonstrating a soft tissue density mass with some enhancement. The location of the mass is one of the few clues toward the correct diagnosis. As the mass enlarges, bony resorption and destruction may be present, with a similar pattern to that seen in patients with squamous cell carcinoma .
Intralesional calcifications representing residual bone fragments are observed in ~40% of cases.
The presence of a focal, often cone-shaped, hyperostosis has been reported to correlate with the point of origin of the lesions . This is useful not only in suggesting the diagnosis, but also to aid surgical planning, as the location of tumor origin determines the extent of surgery required.
Angiography (DSA)
Angiography has no significant role to play in the diagnosis or assessment of inverted papillomas. If performed, these tumors are mostly avascular .
MRI
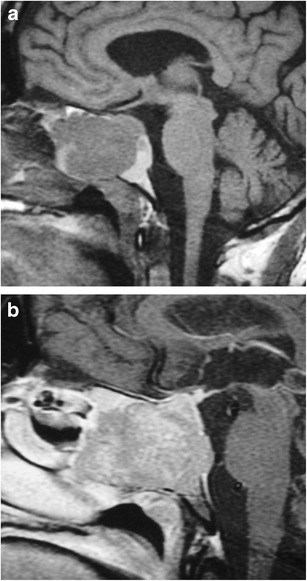
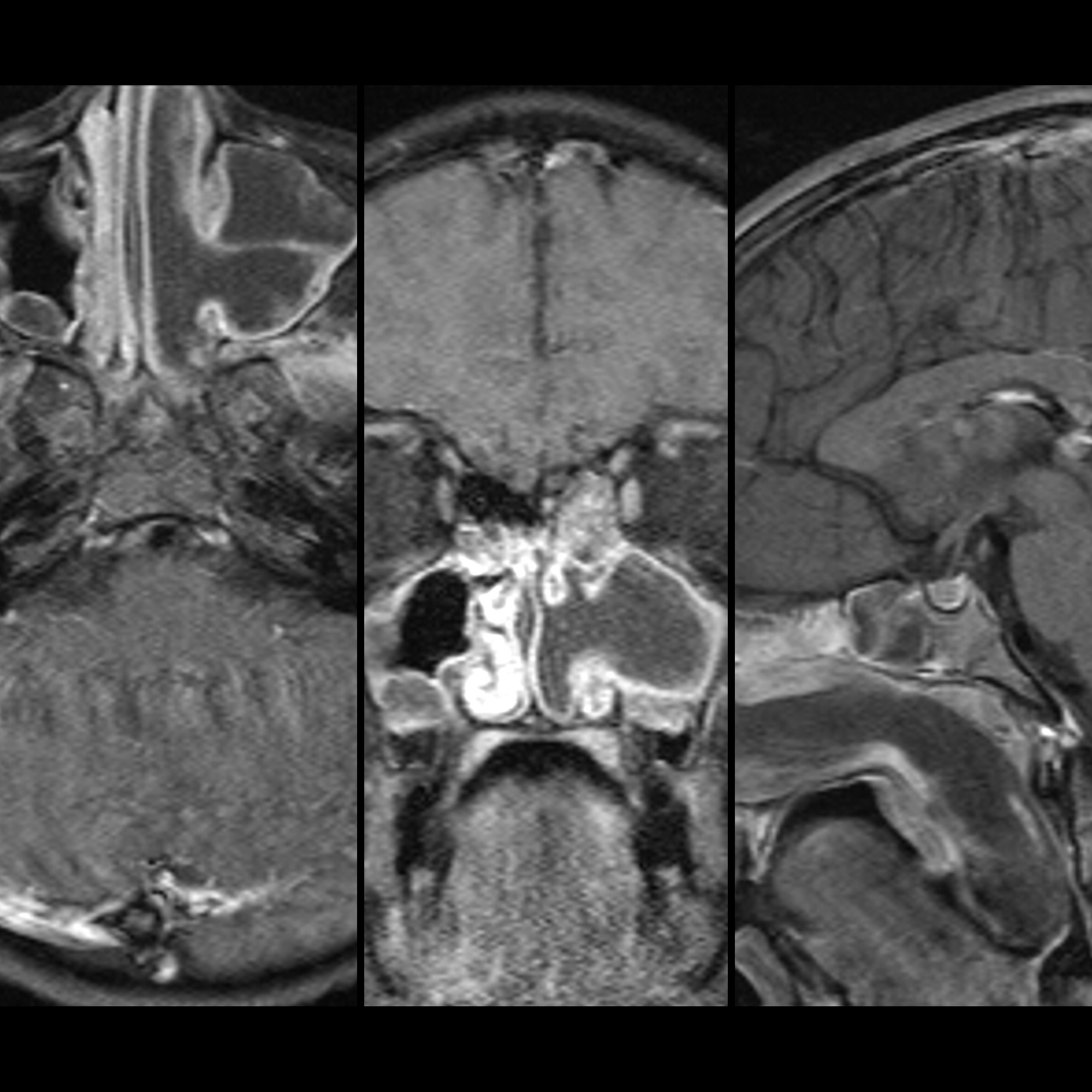
MRI often demonstrates a distinctive appearance, referred to as convoluted cerebriform pattern, seen on both T2 and contrast-enhanced T1 weighted images. This represents alternating lines of high and low signal intensity, the appearance of which has been likened to, albeit loosely, cerebral cortical gyrations. This sign is seen in 50-100% of cases and is uncommon in other sinonasal tumors .
Signal characteristics
- T1: isointense to muscle
- T2
- generally hyperintense to muscle
- alternating hypointense lines
- T1 C+ (Gd)
- heterogeneous enhancement
- alternating hypointense lines
Treatment and prognosis
Due to the high association with malignancy (see above) and their unlimited growth potential, inverted papillomas have historically been resected en bloc with the lateral nasal wall (medial maxillectomy) via an external incision . Increasingly advanced endoscopic techniques have been used to limit the size of resection, and localizing the site of tumor origin is necessary. This is often only possible at the time of surgery but can be suggested by the presence of focal hyperostosis .
Recurrence rates are nonetheless high (15-78%) and are usually attributed to incomplete local resection .
Other than malignant transformation and recurrence, morbidity stems from local growth which can be extensive extending to adjacent spaces including the orbit and intracranial compartment.
Differential diagnosis
General imaging differential considerations include:
- sinonasal carcinoma: unfortunately imaging is unable to confidently distinguish between inverted papillomas, inverted papilloma with malignancy and pure malignancy
- antrochoanal polyp: non-enhancing, peripheral mucosal enhancement may be present
- inflammatory polyp: non-enhancing, peripheral mucosal enhancement may be present
- juvenile nasopharyngeal angiofibroma (JNA)
- olfactory neuroblastoma
- paranasal sinus mucocele
Siehe auch:
- Sinusitis maxillaris
- Verlegung Sinus maxillaris
- Juveniles Angiofibrom
- Ästhesioneuroblastom
- Tumoren der Nasennebenhöhlen
- Mukozele der Nasennebenhöhlen
- Plattenepithelkarzinom der Nasennebenhöhlen
- antrochoanal polyp
- Tumoren der Kieferhöhle
und weiter:

 Assoziationen und Differentialdiagnosen zu Invertiertes Papillom:
Assoziationen und Differentialdiagnosen zu Invertiertes Papillom: