Multiparametric prostate MRI




Prostate MRI has become an increasingly frequent examination faced in daily radiological practice and is usually acquired as either multiparametric or biparametric MRI of the prostate.
Note: This article aims to outline the concept of an MRI protocol for the assessment of the prostate.
Recommendations, given in the Prostate Imaging-Reporting and Data System (PI-RADS) v2.1 document published by an internationally representative group involving the American College of Radiology (ACR), European Society of Urogenital Radiology (ESUR), and AdMeTech Foundation, have been taken into consideration .
Protocol specifics will vary slightly depending on the specific indication, MRI scanner type, specific hardware and software, radiologist and perhaps referrer preference, patient factors e.g. implants, and time constraints.
Multiparametric vs biparametric prostate MRI
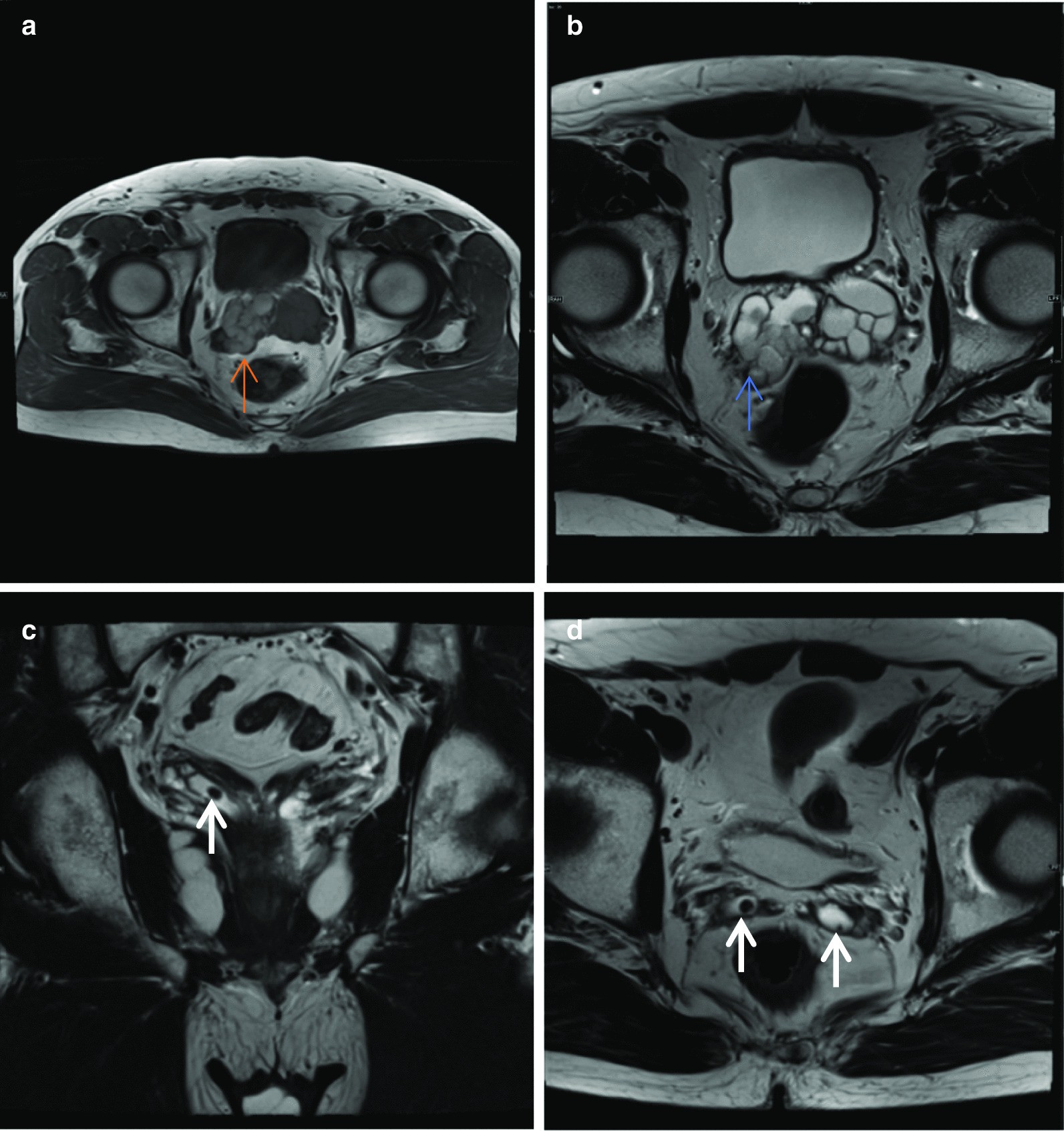
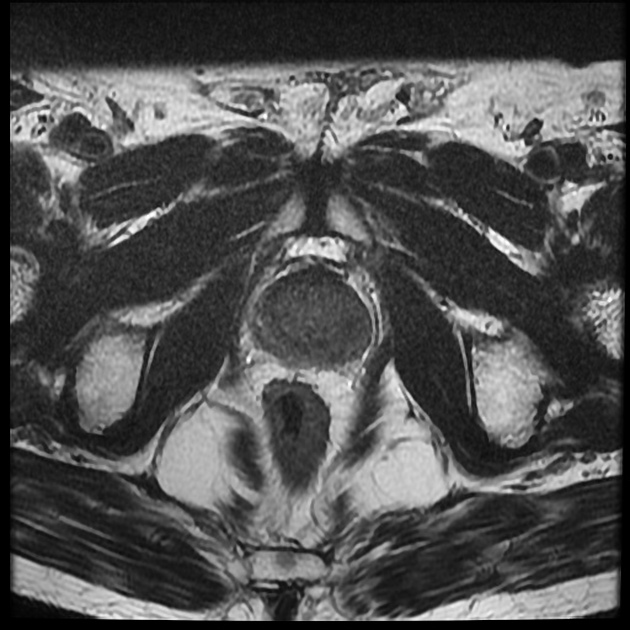
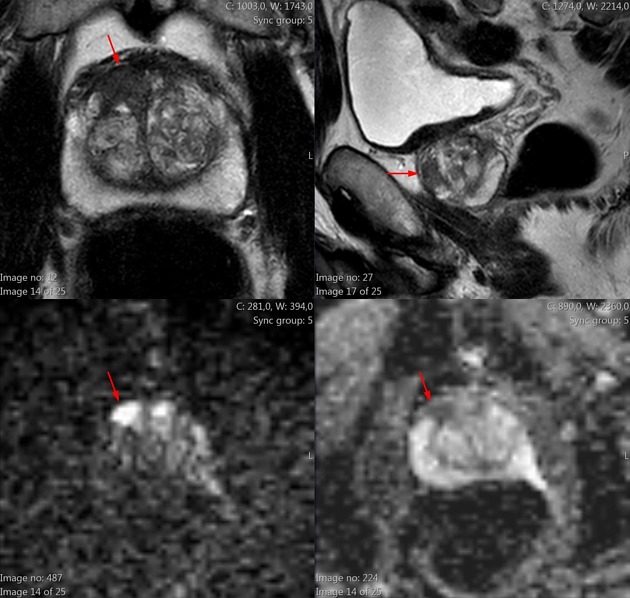
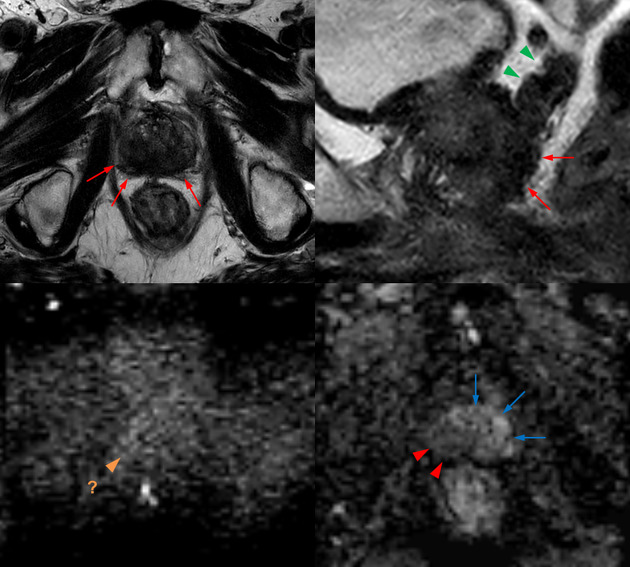
A multiparametric MRI (mpMRI) of the prostate combines the anatomic information from T1 and T2 weighted sequences with functional information from diffusion-weighted imaging (DWI) and dynamic contrast enhancement (DCE). In some situations other techniques like MR spectroscopy (MRS) have also been employed, although the latter is not widely used.
Due to the limited role of dynamic contrast enhancement in the detection of prostate cancer, some institutions acquire a biparametric MRI (bpMRI) basically consisting of T1 and T2-weighted images as well as diffusion-weighted images omitting contrast media .
Indications
The detection and localization of clinically significant prostate cancer in patients with negative biopsy or without a previous biopsy is a major goal of multi- or biparametric MRI of the prostate .
Other important indications include :
- active surveillance
- locoregional prostate cancer staging
- detection of locoregional recurrence in a post-prostatectomy setting
1.5 vs 3 tesla
Due to an improved signal-to-noise ratio (SNR), the multi- and biparametric MRI protocols for the prostate definitely benefit from increased field strength. However, nowadays with newer scanner types a multi- or biparametric prostate MRI can be conducted with reasonably decent quality even without endorectal coils and should/might be considered in the following situations:
- uni- or bilateral hip arthroplasty or other metallic implants of the pelvis
- MR conditional implants or devices requiring a lower field strength
- extensive tattoos in the pelvic girdle area
Patient preparation
There is no clear consensus regarding all aspects of patient preparation and their clinical significance.
- prevention of diagnostic compromise due to post-biopsy change
- an interval of ≥ 6 weeks should be considered
- bowel motion artefact reduction
- antispasmodic agents (e.g. hyoscine butylbromide – Buscopan ®) – cave: driving
- fasting period for 4 hours – seems reasonable
- bowel evacuation – recommended before the examination
- abstinence from ejaculation
- aims at a proper distention of seminal vesicles
- no clearly established benefit
- probably more of use in staging cases
Patient positioning
A diagnostic multi- or biparametric MRI of the prostate is conducted with the patient in the supine position.
Technical parameters
Coil
Multi-phased-array coils are recommended.
- anterior surface coil, posterior coil
- cardiac coil
Scan geometry
- in-plane spatial resolution: varies with the sequence and the plane
- field of view (FOV): 120-200 mm for
- slice thickness: ≤3 mm for all but axial T1 weighted images
Planning
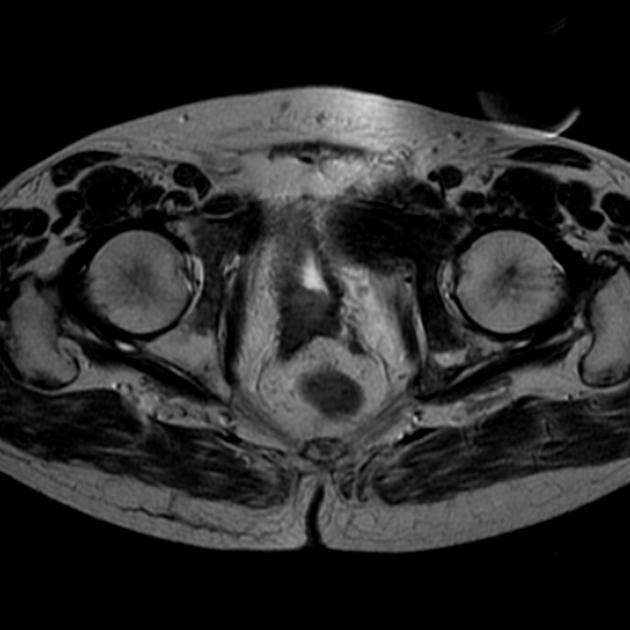
A typical MRI of the prostate should look like the following:
- axial images:
- angulation: strictly axial to the body axis, perpendicular to the body z-axis
- volume: from the bulb of the corpus spongiosum including the whole seminal vesicles
- slice thickness: ≤3 mm, no gap except for overview
- in-plane spatial resolution: ≤ 0.5 x 0.5 mm
- sagittal images:
- angulation: strictly sagittal to the body axis
- volume: from right to left iliac fossa including internal obturator muscle
- slice thickness: ≤3 mm, no gap
- in-plane spatial resolution: ≤ 0.7 x 0.7 mm
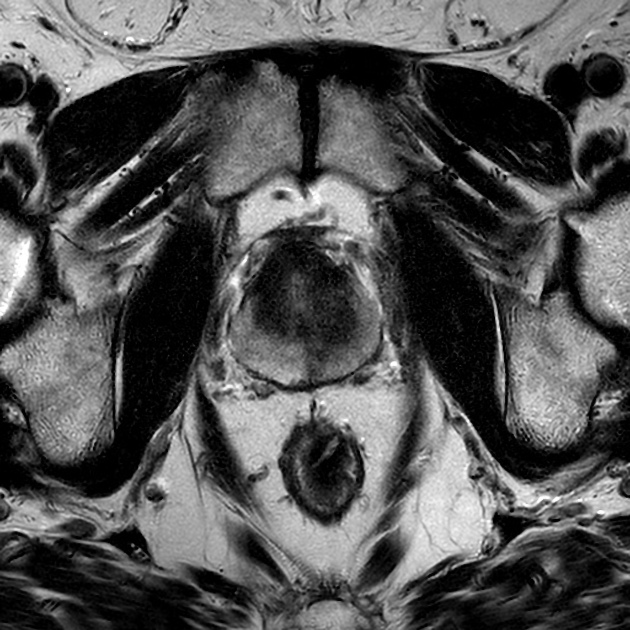
- coronal images:
- angulation: strictly coronal to the body axis
- volume: from the anterior edge of the pubic bone to the mid rectum or ischial bones
- slice thickness: ≤3 mm, no gap
- in-plane spatial resolution: ≤ 0.7 x 0.7 mm
- axial oblique images*:
- angulation: perpendicular to the z-axis of the prostate
- volume: should include the whole prostate and both seminal vesicles
- slice thickness: ≤3 mm, no gap
- in-plane spatial resolution: ≤ 0.5 x 0.5 mm
- coronal oblique images*:
- angulation: parallel to the posterior boundary of the prostate (will often equal the coronal body axis)
- volume: should include the whole prostate and both seminal vesicles
- slice thickness: ≤3 mm, no gap
- in-plane spatial resolution: ≤ 0.7 x 0.7 mm
Sequences
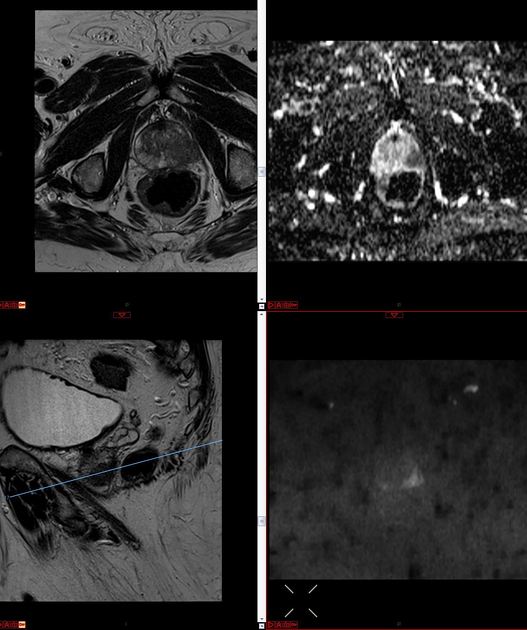
A standard MRI of the prostate consists of T1 and T2 weighted images depicting prostate morphology, diffusion-weighted images and in case of a multiparametric acquisition dynamic contrast enhancement.
Standard sequences
- T1 weighted
- purpose: general overview, detection of prostatic hemorrhage, pelvic bone and soft-tissue characterization, assessment of lymph nodes
- technique: T1 fast spin echo
- planes: axial
- slice thickness and in-plane resolution: might be increased for increased anatomic coverage
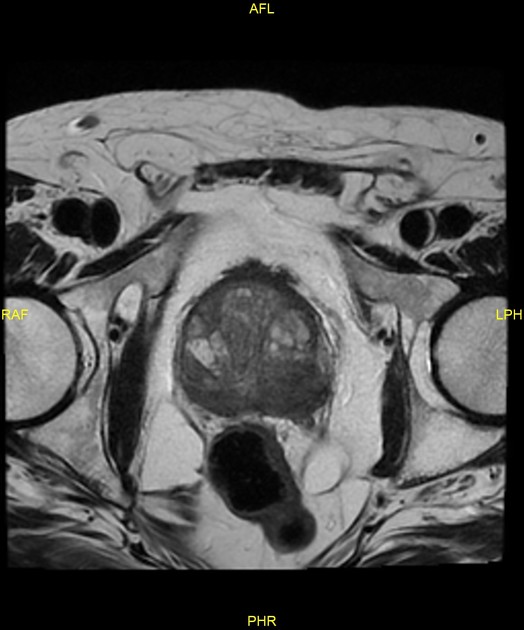
- T2 weighted
- purpose: glandular morphology, main sequence for the evaluation of the transition zone, assessment of extraprostatic extension (EPE) and seminal vesicle invasion (SVI)
- technique: T2 fast spin echo
- planes: axial (oblique*), sagittal, coronal (oblique*)
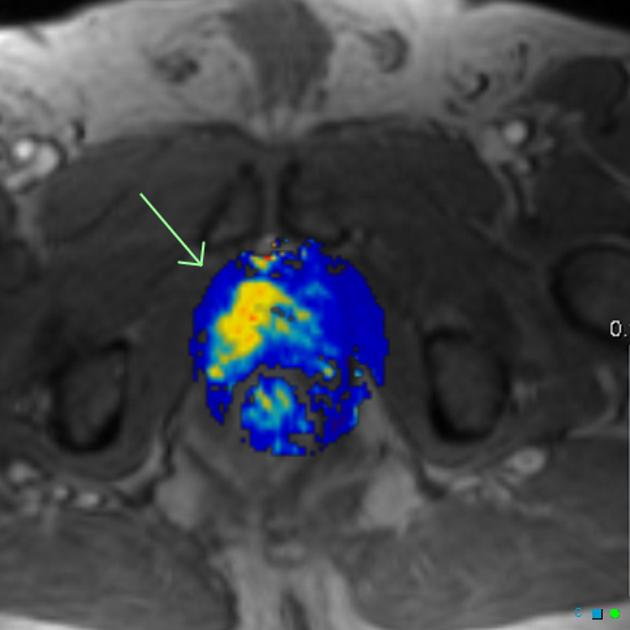
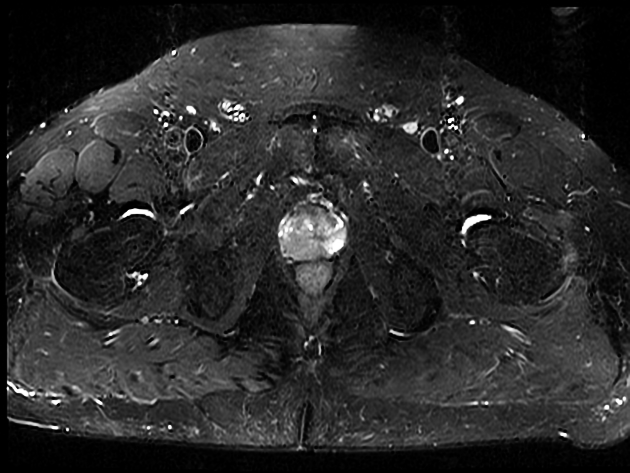
- DWI
- purpose: reflects the random motion of water molecules and adds a key functional component in the depiction of hypercellular tissue, main sequence for the evaluation of the peripheral zone
- technique
- at least b50-100 & b800-1000 for ADC calculation
- separate acquisition or calculation of high b-value ≥1400
- planes: axial (oblique*)
- in-plane spatial resolution: ≤ 2 x 2 mm
Optional sequences
- dynamic contrast enhancement (DCE)
- purpose: might improve differentiation of equivocal versus likely malignant peripheral lesions, important for the evaluation of locoregional recurrence in a post-prostatectomy setting
- technique: T1 GRE
- injection: 0.1 mmol/kg at 3ml/s
- planes: axial (oblique*)
- in-plane spatial resolution: ≤ 2 x 2 mm
- temporal resolution: ≤ 15 sec some recommendations are < 10 sec
- T2 weighted (3D)
- purpose: glandular morphology
- technique: T2 fast spin echo
- planes: axial
- in-plane spatial resolution: isotropic ≤ 0.7 mm
Practical points
- use the same examination volumes and angulations for axial T2, DWI and DCE
- use same slice thickness for all sequences except 3D imaging
- if possible calculate high b-value
- in a patient with hip arthroplasty
- plan a multiparametric acquisition right away - DWI is more likely to suffer from artefacts
- use metal artefact reduction algorithms if applicable
See also
Siehe auch:
- MR spectroscopy in prostate cancer
- extracapsular extension of prostate cancer
- PI-RADS
- ESUR prostate MR guidelines
- Staging Prostatakarzinom
und weiter:

 Assoziationen und Differentialdiagnosen zu MRT der Prostata:
Assoziationen und Differentialdiagnosen zu MRT der Prostata: