necrotizing fasciitis






Necrotizing fasciitis (rare plural: necrotizing fasciitides) refers to a rapidly progressive and often fatal aggressive necrotizing soft tissue infection primarily involving and spreading along the fascia.
Terminology
As fascia is variably defined, there can be confusion as to what it constitutes. While anatomy texts often define superficial fascia as including the subcutaneous fat layer, the latest international nomenclature, Terminologia Anatomica, abandoned the term and most surgeons consider "fascia" to refer primarily to the deep (investing) fascia . Therefore, findings of infection in the subcutaneous tissue are usually considered part of cellulitis, while fasciitis is reserved for the involvement of the deep fascia .
Epidemiology
Necrotizing fasciitis is relatively rare, although its prevalence is thought to be rising.
Risk factors
The most common risk factor is diabetes mellitus, especially in combination with peripheral arterial disease. Other predisposing factors include immunocompromise due to HIV infection, cancer, alcoholism, and organ transplants. However, infections can occur in otherwise healthy individuals following surgery, penetrating trauma, minor wounds such as insect bites or abrasions, or even blunt trauma with no clear portal of entry .
Clinical presentation
The most common clinical findings overlap with that of non-necrotizing soft tissue infection, including local edema and erythema . Findings that are more concerning for necrotizing infection include acute onset severe pain, crepitus, skin necrosis, bullae and signs of systemic toxicity/sepsis such as fever and hypotension . Necrotizing fasciitis is ultimately a surgical diagnosis, based on direct inspection of friable superficial fascia and foul grey "dishwater" exudate .
Pathology
Microbiologically, there are two major recognized forms:
- polymicrobial (type I): most common; involves both anaerobic and aerobic organisms, such as Clostridium, Bacteroides, and Peptostreptococcus in the former group, and Enterobacteriaceae family members and Staphylococcus aureus in the latter group
- monomicrobial (type II): less common (10-15%); most commonly involves group A streptococci, the “flesh-eating bacteria” and may be complicated by toxic shock syndrome ; less commonly due to Staphylococcus aureus
The presence of anaerobes (or facultative anaerobes) in type I infection is responsible for the hallmark finding of gas formation found later in the course of polymicrobial necrotizing fasciitis. However, the finding is not present in monomicrobial necrotizing fasciitis due to group A streptococci.
Soft tissue infarction is the end result with liquefaction of fat and muscle.
Location
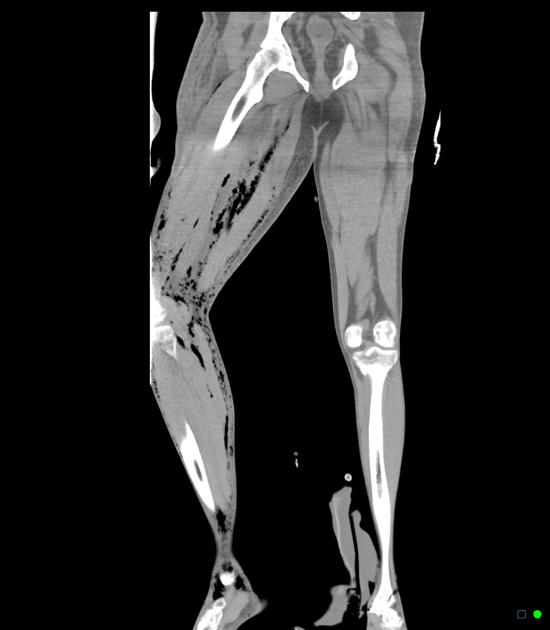
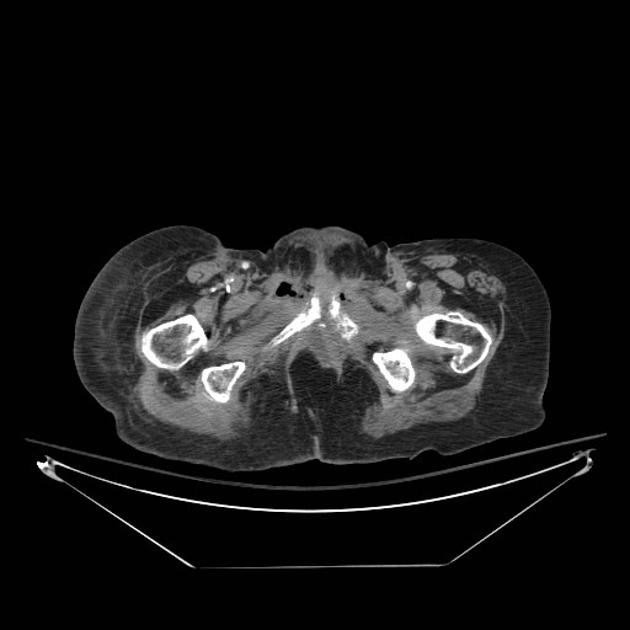
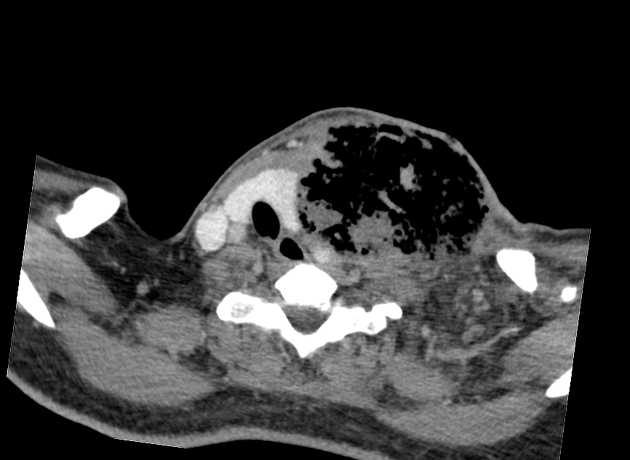
While it can affect any part of the body, 50% of cases involve the lower extremities. Other common areas include the upper extremities, the perineum (Fournier gangrene), and head and neck region . In neonates, the most common area involved is the trunk .
Radiographic features
Imaging is more sensitive than physical exam for detecting the hallmark feature of soft tissue gas (subcutaneous emphysema) and can also identify findings contributing to infection such as foreign bodies . However, no imaging modality can exclude the diagnosis with certainty and a study with only non-specific evidence of soft tissue inflammation should not preclude or delay surgical exploration and intervention in cases with high clinical suspicion for necrotizing infection.
Plain film
Radiographs can be normal until the advanced stages of infection and necrosis. Early findings are non-specific, similar to those of cellulitis, such as increased soft-tissue thickness and opacity. Soft tissue gas is seen in only a minority of cases.
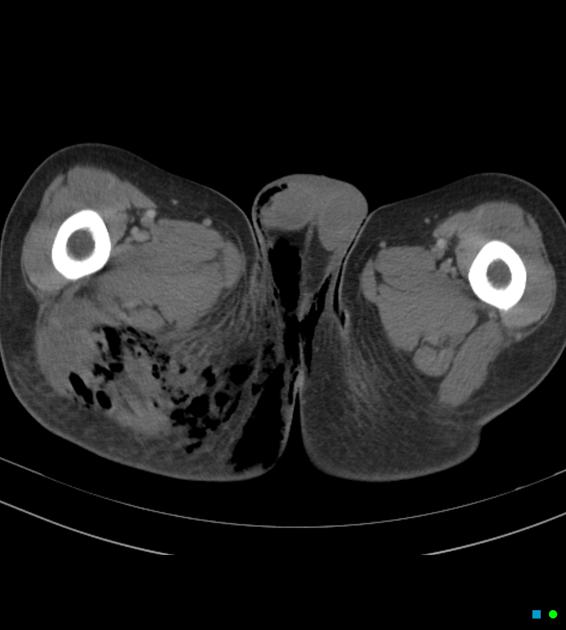
CT
CT is the most commonly used imaging modality for evaluation of suspected necrotizing fasciitis owing to its speed and sensitivity for gas in the soft tissues. The sensitivity of CT is 80%, but the specificity is low given overlapping features with non-necrotizing fasciitis . Gas within fluid collections tracking along fascial planes is the most specific finding but is not always present .
Other, non-specific findings include:
- asymmetrical fascial thickening associated with fat stranding
- edema extending into the intermuscular septa and the muscle
- thickening of one or both of the superficial and deep fascial layers
Although fascial fluid collections are typically non-focal, abscesses may be seen.
On contrast-enhanced CT, diffuse enhancement of fascia and / or underlying muscle can be seen but is present in both necrotizing or non-necrotizing fasciitis . On the other hand, absent enhancement of the thickened fascia suggests necrosis .
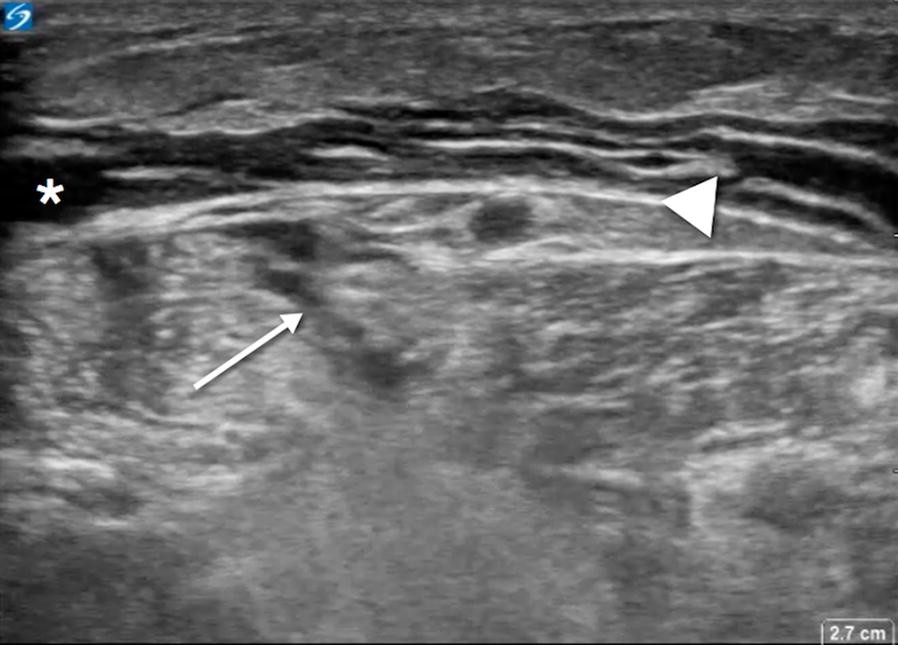
Ultrasound
Ultrasound may be more useful in children (with a rising incidence after primary varicella infection ). Sonographic findings include distorted and thickened fascial planes with turbid fluid accumulation in the fascial layers and subcutaneous edema. Soft tissue gas appears as a layer of echogenic foci with posterior dirty shadowing .
MRI
MRI is the gold standard imaging modality for the investigation of necrotizing fasciitis with a sensitivity of 93% . Findings include :
- T2 FS or STIR
- fascial thickening ≥3 mm and hyperintensity, starting in the superficial fascia and often involving deep intramuscular fascia in multiple compartments
- subfascial and interfascial fluid collections
- low signal foci of gas
- subcutaneous edema, although commonly seen with cellulitis as well
- T1
- subtle loss of muscle texture and possible high signal intensity compatible with intramuscular hemorrhage
- low signal foci of gas
- T1+C
- variable fascial contrast enhancement: increased early due to capillary permeability but absent later due to necrosis
Treatment and prognosis
Necrotizing fasciitis is a surgical emergency. Definitive diagnosis and treatment involve prompt surgical fasciotomy with aggressive debridement of the necrotic tissue. Antibiotics are started with broad-spectrum coverage, including anaerobes, and tailored when culture data are available. Subsequent repeat (second look) surgery is necessary until no necrotic tissue is found. Any delay in treatment may cause extensive soft tissue loss and loss of limb. Amputation may be required to pre-empt further spread of infection. Mortality rates can range between 9-25% .
Differential diagnosis
For soft tissue inflammatory findings, consider :
- non-necrotizing fasciitis, cellulitis, and/or myositis
- ischemic myonecrosis
- dermatomyositis
- graft versus host disease
For gas within soft tissues, consider:
- gas gangrene (clostridial myonecrosis)
- penetrating trauma or percutaneous/surgical procedure
- communication from the aerodigestive tract (e.g. pneumomediastinum, esophageal perforation)
History and etymology
The entity was described by Hippocrates in the 5th century BC as a complication of erysipelas, termed hospital gangrene in a large series by Joseph Jones (an American army surgeon during the American Civil War), and finally called "necrotizing fasciitis" in 1952 in an article by B Wilson .
See also
Siehe auch:
- Weichteilemphysem
- Fournier-Gangrän
- infektiöse Myositis
- gasbildende Weichteilinfektionen
- streptococcal myositis
und weiter:
 Assoziationen und Differentialdiagnosen zu Nekrotisierende Fasziitis:
Assoziationen und Differentialdiagnosen zu Nekrotisierende Fasziitis:



