optic nerve sheath meningioma





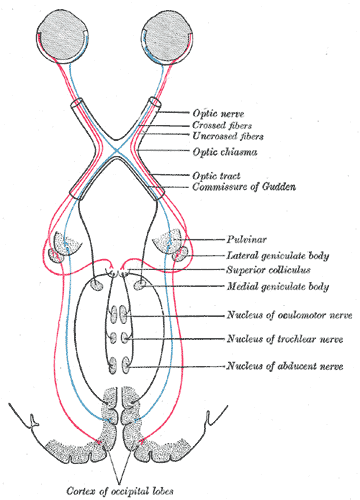
Optic nerve meningiomas are benign tumors arising from the arachnoid cap cells of the optic nerve sheath and represent ~20% of all orbital meningiomas, the majority of which are direct extensions from intracranial meningiomas.
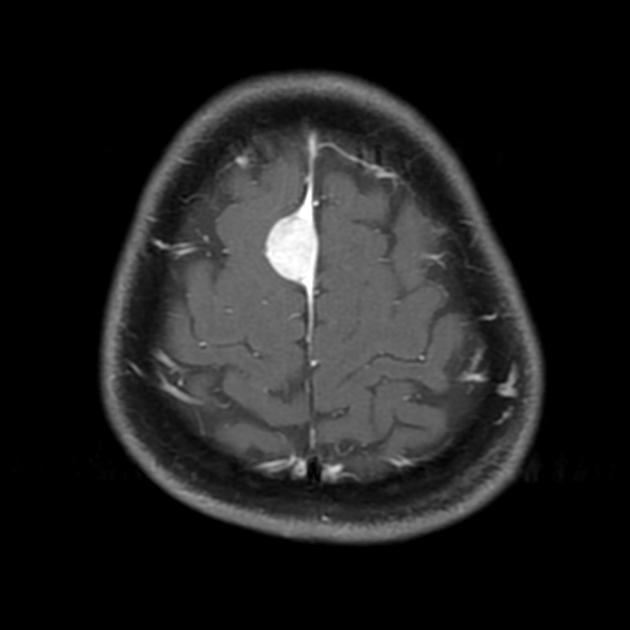
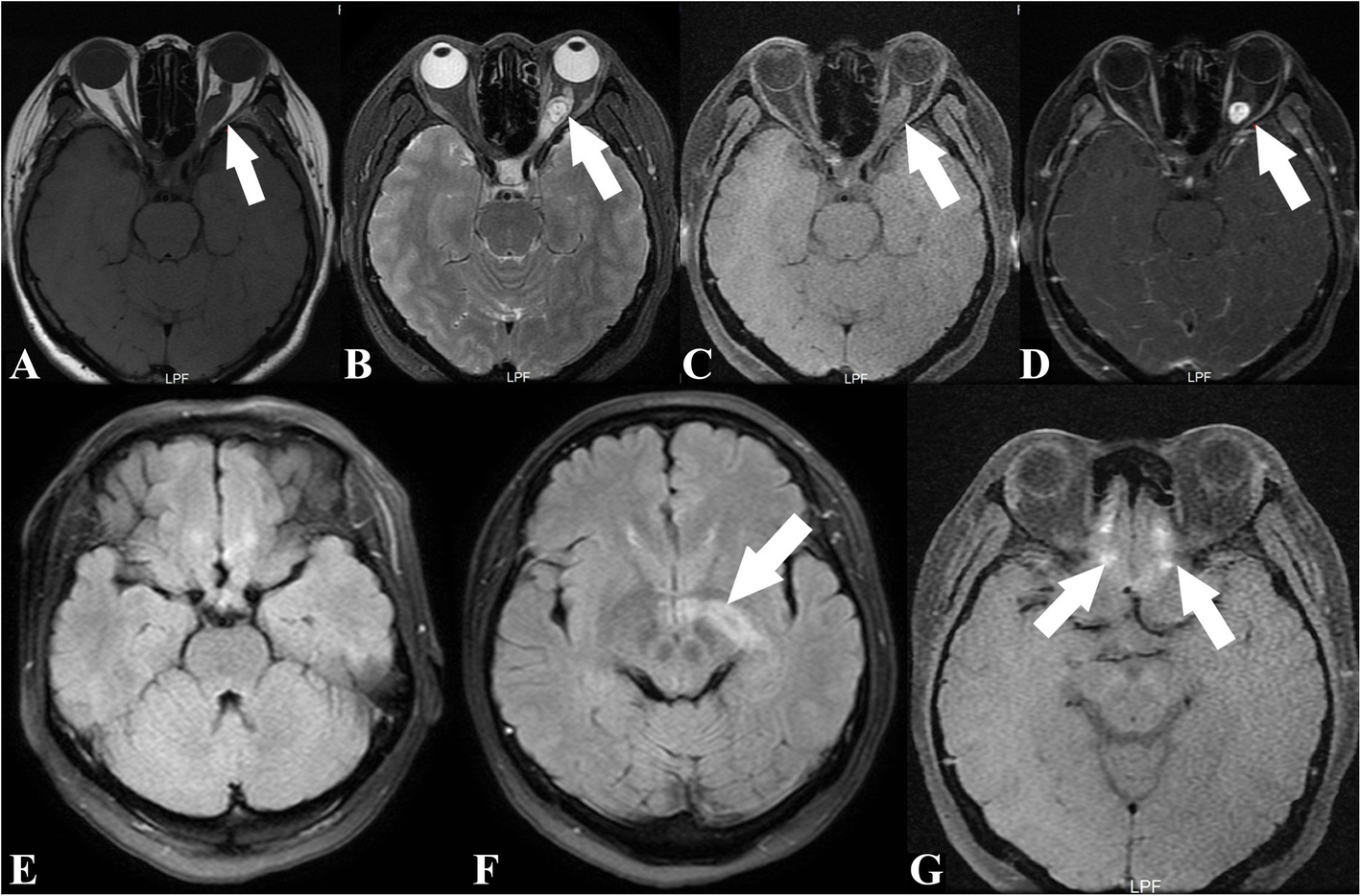
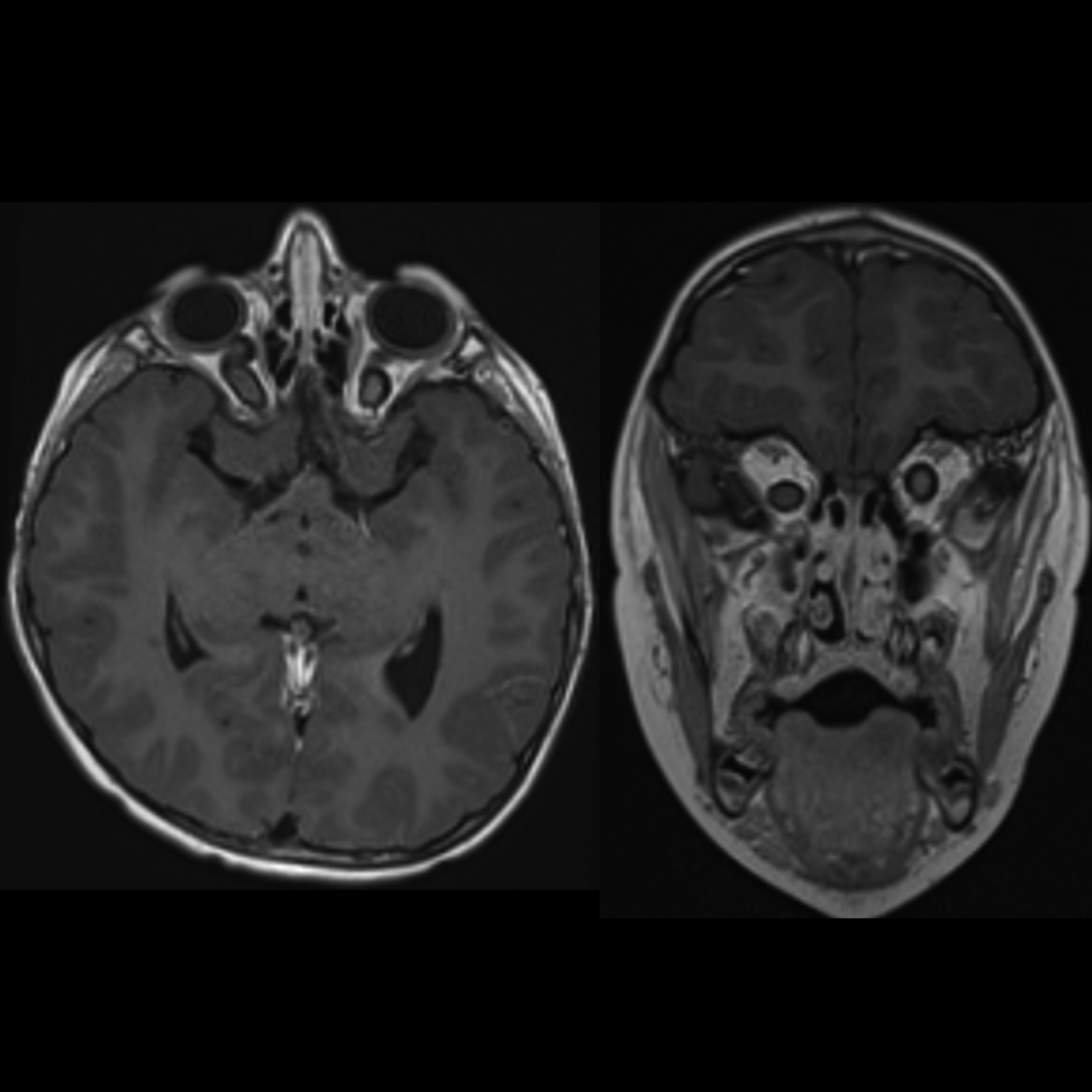
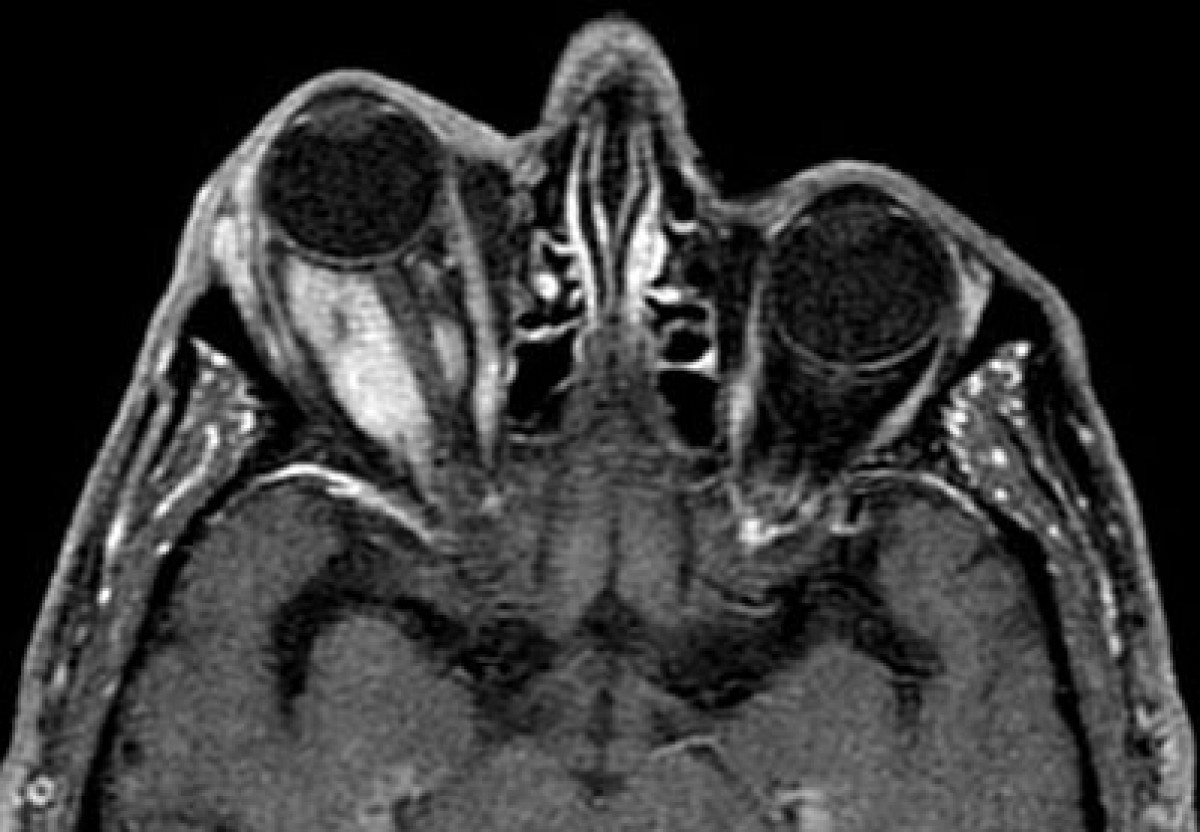
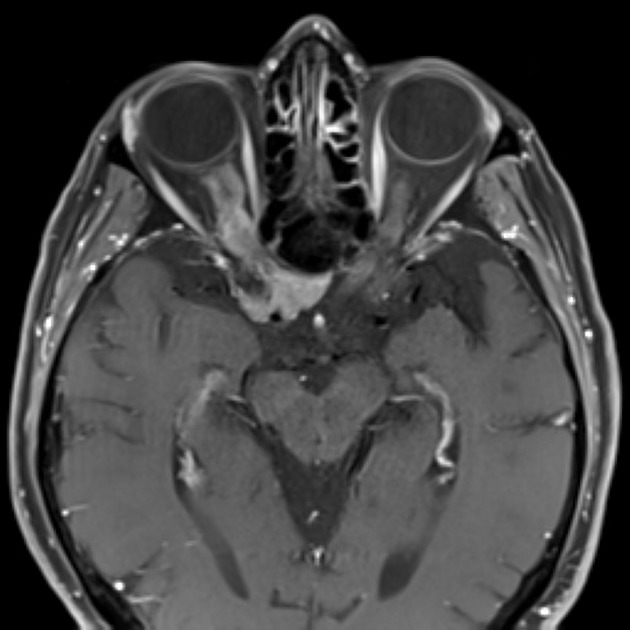
These tumors typically appear as masses within the optic nerve, isointense to grey matter on both T1 and T2 weighted imaging, demonstrating vivid enhancement which clashes with the non-enhancing optic nerve ("tram-track sign" on axials or "non-enhancing dot sign" on coronals).
Epidemiology
Optic nerve meningiomas account for approximately a third of all optic nerve neoplasms; optic nerve gliomas are the most common entity. Unlike optic nerve gliomas which occur primarily in children, optic nerve meningiomas are usually seen in adults (mean age at presentation 40 years) , however up to 25% present in children, in which case they tend to be more aggressive .
Similar to meningiomas elsewhere there is a female predilection .
The vast majority of cases are sporadic, although patients with neurofibromatosis type II (NF2) are at increased risk.
Clinical presentation
Clinical presentation is with a combination of:
- present to a greater or lesser degree in 95% of cases
- initially, visual obscurations may be transient
- painless and progressive
- more pronounced with lesions that affect the orbital apex
- exacerbated during pregnancy
- present to a greater or lesser degree in 60-90% of cases
- more pronounced with anterior lesions near the globe
- occurs later, as a tumor enlarges
- may be exacerbated by associated hyperostosis
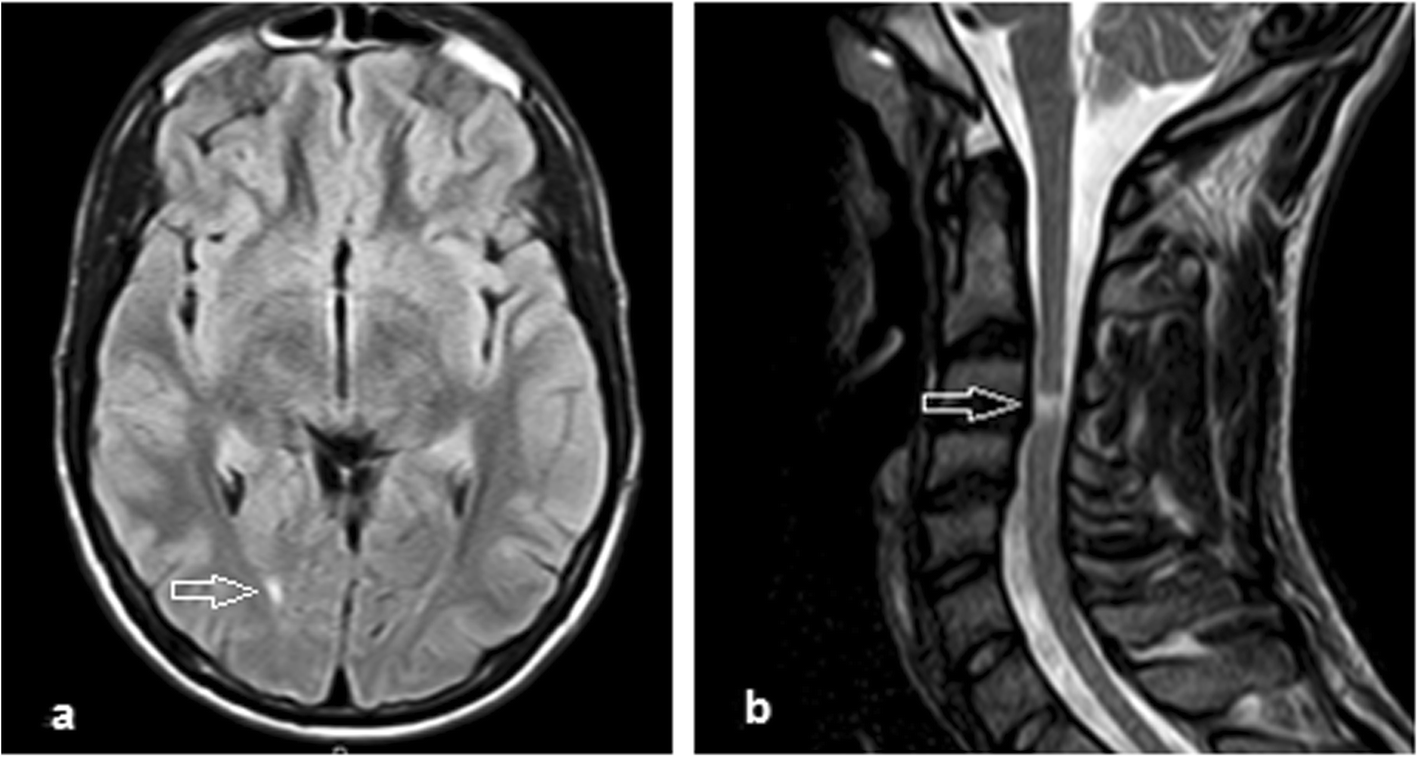
These lesions are almost always unilateral, with the exception of NF2 patients who may develop bilateral tumors. Occasionally a unilateral tumor will grow posteriorly, across the chiasm and along the contralateral nerve.
A particular clinical presentation is worth mentioning due to the potential pitfall. An intracanalicular lesion may cause marked visual loss with a very small tumor and clinical presentation may be similar to optic neuritis. As these patients are often middle-aged women, the diagnosis of multiple sclerosis may be suspected. Thus in patients being imaged for 'optic neuritis' careful inspection of the optic canals is important .
Pathology
Optic nerve meningiomas arise from the arachnoid cap cells of the optic nerve sheath, and as such are on the inside of the dura (remember that the arachnoid layer is immediately deep to the inner layer of the dura mater). The tumor extends through the overlying dura and typically has a smooth or somewhat lobulated contour. The optic nerve, which is usually circumferentially encased, gradually atrophies due to compression .
The most common type of meningioma histologically is the meningothelial variety .
Radiographic features
Meningiomas of the optic nerve sheath have the same imaging characteristics as meningiomas elsewhere. The morphology of the tumor is variable:
- tubular: 65%
- exophytic: 25%
- fusiform: 10%
Occasionally cysts filled with arachnoid fluid develop between the globe and the anterior margin of the tumor as a result of impaired CSF flow backward. These are known as perioptic cysts .
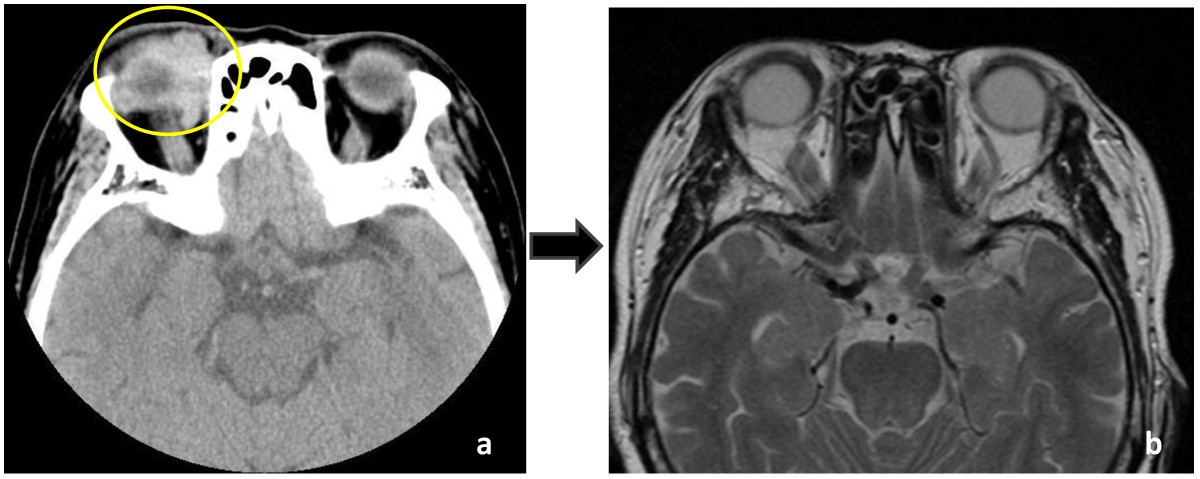
CT
The tumor is usually isoattenuating to the optic nerve on non-contrast studies, although calcification is sometimes seen. Following administration of contrast, the tumor enhances .
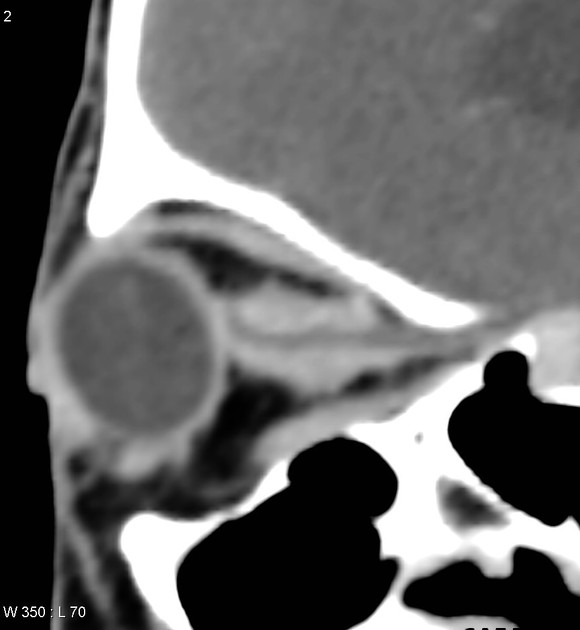
On axial or oblique sagittal imaging the enhancing tumor surrounding the non-enhancing optic nerve results in the so-called tram-track sign. This is most evident in tumors with tubular growth pattern.
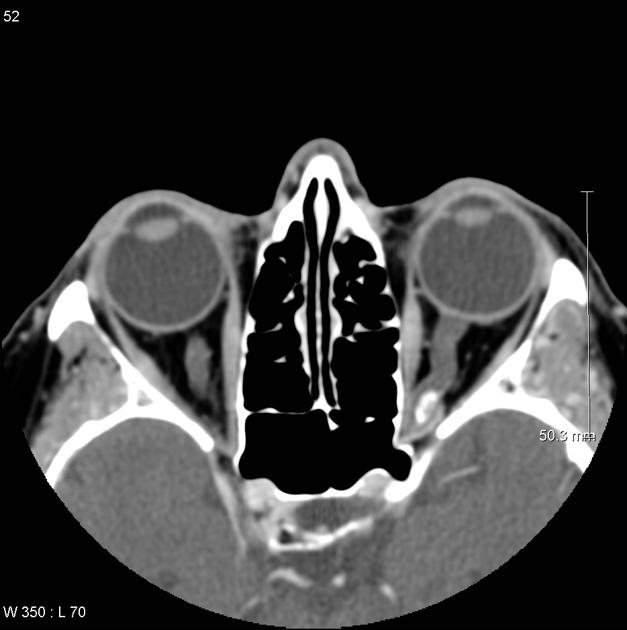
On coronal imaging, the tumor appears as a cuff of enhancing tumor around a central non-enhancing dot (optic nerve) giving a doughnut appearance (doughnut sign).
Tumor extending into the optic canal may lead to canal widening, or alternatively hyperostosis .
MRI
Appearances on MRI are similar to those on CT with a greater ability to delineate posterior extension. Imaging should include thin axial and coronal (+/- sagittal) T1, fat-suppressed T2 and fat-suppressed postcontrast T1 sequences.
- T1: isointense to somewhat hypointense compared to the optic nerve
- T1 C+ (Gd): homogeneous enhancement
- T2: isointense to somewhat hyperintense compared to the optic nerve
Careful examination of the orbital apex and optic nerve canals is essential if small intracanalicular tumors are to be identified .
Treatment and prognosis
Treatment of these lesions is problematic and depends on the degree of visual impairment and proptosis. In patients with preserved vision and no proptosis, conservative management with frequent ophthalmologic and radiological follow-up is usually preferred. When vision begins to fail surgical intervention is tempting but often of limited success as far as preserving vision is concerned. Fenestration of the dural sheath has been tried but is of no benefit .
Severe proptosis requires surgery but almost invariably results in loss of vision.
Another indication for surgery is imaging evidence of posterior growth, as this not only makes future attempts at surgical excision much harder, but the mass also threatens the contralateral eye.
Radiotherapy has an increasing role in the management of these lesions. Conventional radiotherapy has been used both pre-operatively and postoperatively for many years. More recently stereotactic radiotherapy has been employed as an alternative to surgery, and may well be superior. Care must be exercised however due to the proximity of other important radiosensitive structures .
Differential diagnosis
A number of entities can mimic an optic nerve meningioma and result in enlargement of the optic nerve. More common entities to be considered in the differential include:
Siehe auch:
- Meningeom
- intraorbitale Raumforderungen
- Sarkoidose
- Dura mater
- Encephalomyelitis disseminata
- inflammatorischer Pseudotumor der Orbita
- orbitales Lymphom
- intraconal orbital compartment
- Metastasen in der Orbita
- Nervus opticus
- Opticusgliom
- tram-track sign
- Neurofibromatose Typ 2
- intracranial meningiomas
- verdickter Nervus Opticus
- Tumoren des Nervus opticus
- Meningeom der Orbita
und weiter:

 Assoziationen und Differentialdiagnosen zu Meningeom Nervus opticus:
Assoziationen und Differentialdiagnosen zu Meningeom Nervus opticus: