Osteomyelitis























Osteomyelitis (plural: osteomyelitides) refers to inflammation of bone that is almost always due to infection, typically bacterial. This article primarily deals with pyogenic osteomyelitis, which may be acute or chronic.
Other non-pyogenic causes of osteomyelitis are discussed separately:
- fungal osteomyelitis
- skeletal syphilis
- tuberculous osteomyelitis
Epidemiology
Osteomyelitis can occur at any age. In those without specific risk factors, it is particularly common between the ages of 2-12 years and is more common in males (M: F of 3:1) .
Pathology
In most instances, osteomyelitis results from haematogenous spread, although direct extension from trauma and/or ulcers is relatively common (especially in the feet of diabetic patients).
In the initial stages of infection, bacteria multiply, triggering a localized inflammatory reaction that results in localized cell death. With time, the infection becomes demarcated by a rim of granulation tissue and new bone deposition.
Although no organisms are recovered in up to 50% of cases , when one is isolated, Staphylococcus aureus is by far the most common pathogen. Different organisms are more common in specific clinical scenarios :
- Staphylococcus aureus: 80-90% of all infections
- Escherichia coli: intravenous drug users (IVDU) and genitourinary tract infection
- Pseudomonas spp.: IVDU and genitourinary tract infection
- Klebsiella spp.: IVDU and genitourinary tract infection
- Salmonella spp.: sickle cell disease
- Haemophilus influenzae: neonates
- group B streptococci: neonates
Other uncommon infective agents include
- fungi - fungal osteomyelitis
Location
Frequency by location, in descending order :
- lower limb (most common)
- vertebrae: lumbar > thoracic > cervical
- radial styloid
- sacroiliac joint
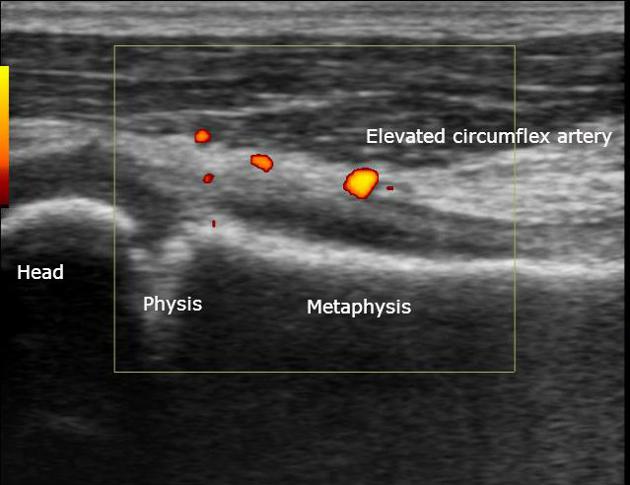
The location of osteomyelitis within a bone varies with age, on account of changes in vascularization of different parts of the bone :
- neonates: metaphysis and/or epiphysis
- children: metaphysis
- adults: epiphyses and subchondral regions
Variants
Radiographic features
In some instances, radiographic features are specific to a region or a particular type of infection, for example:
Below are the general features of osteomyelitis.
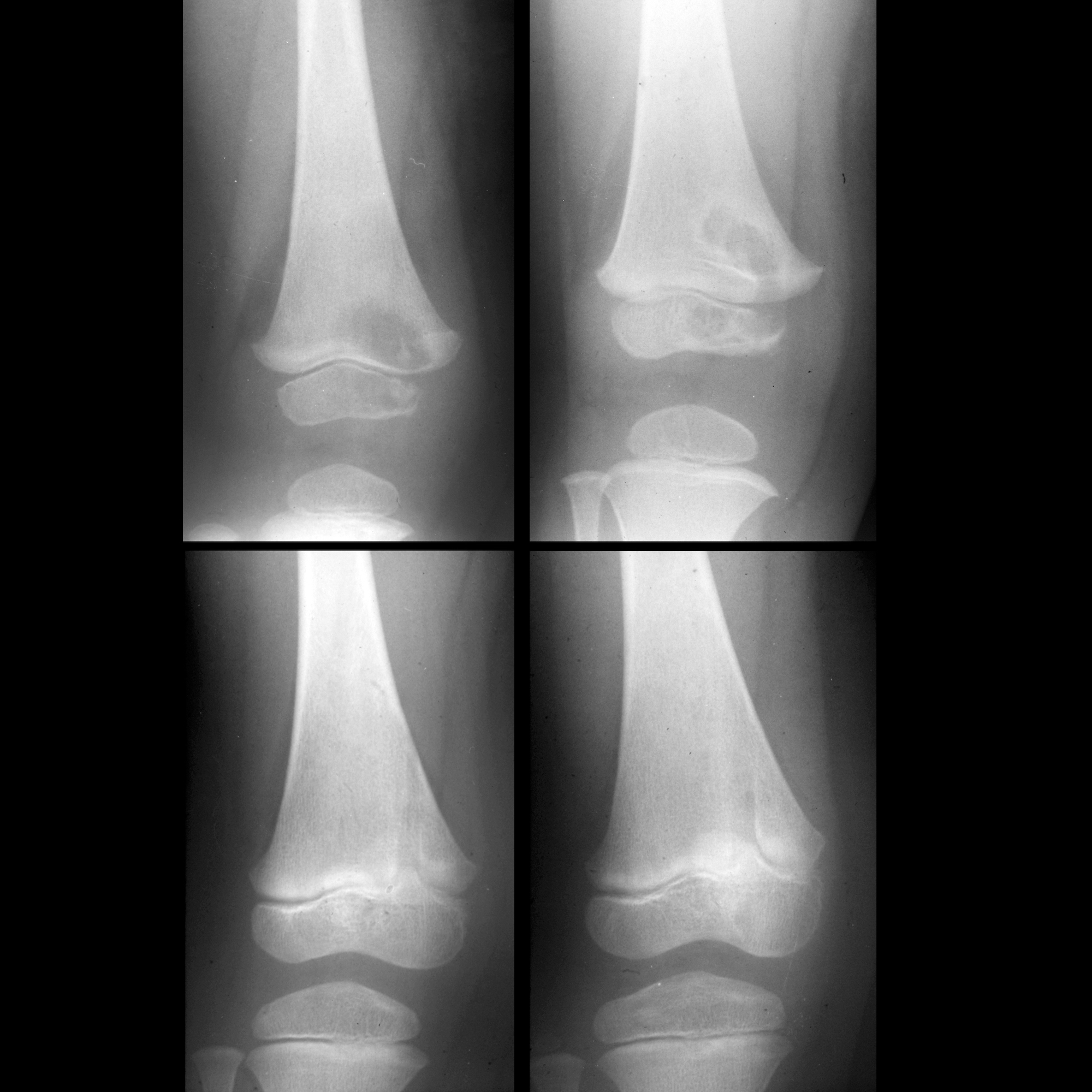
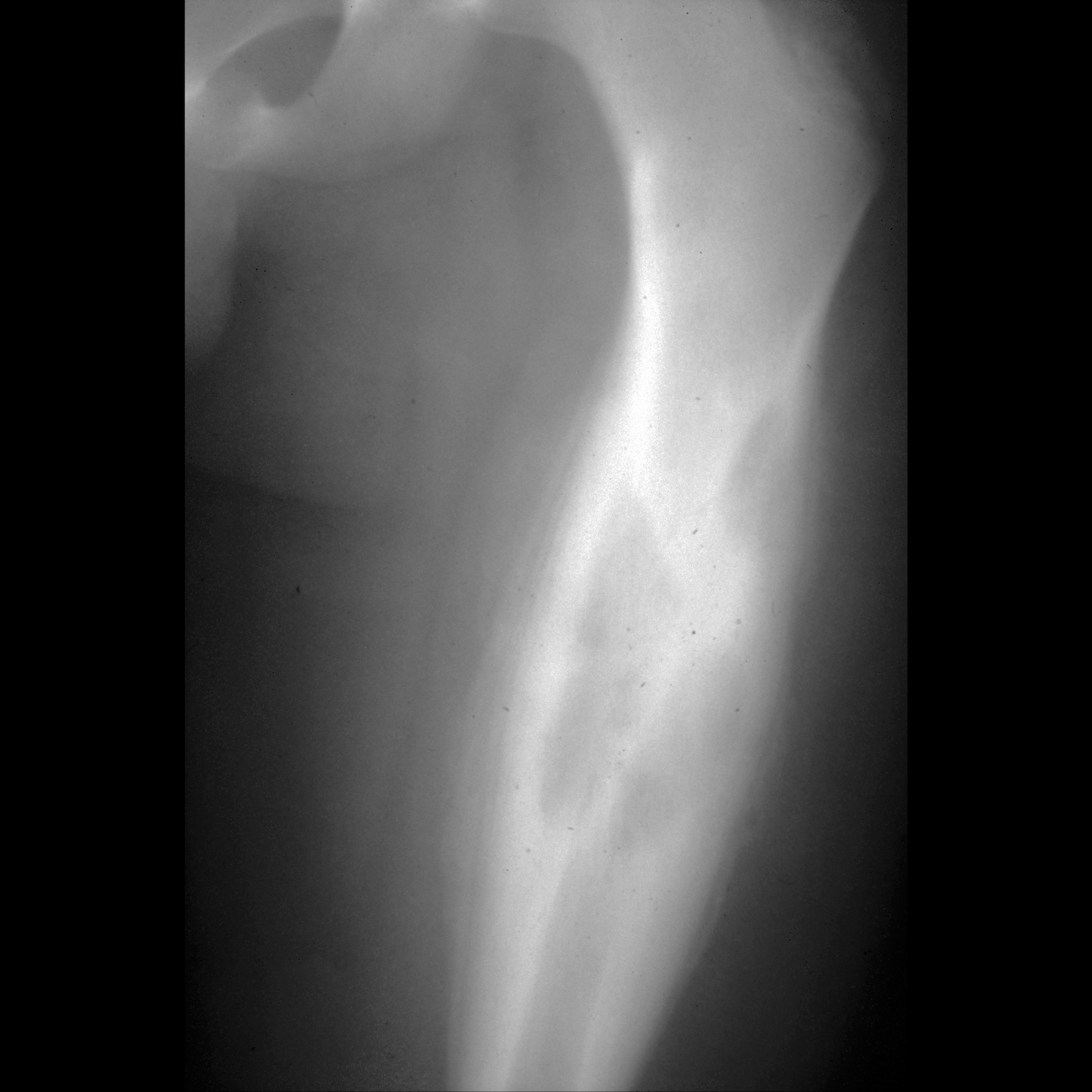
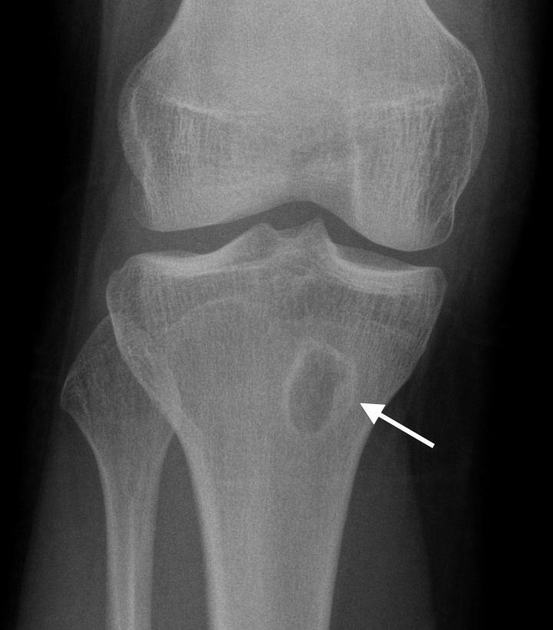
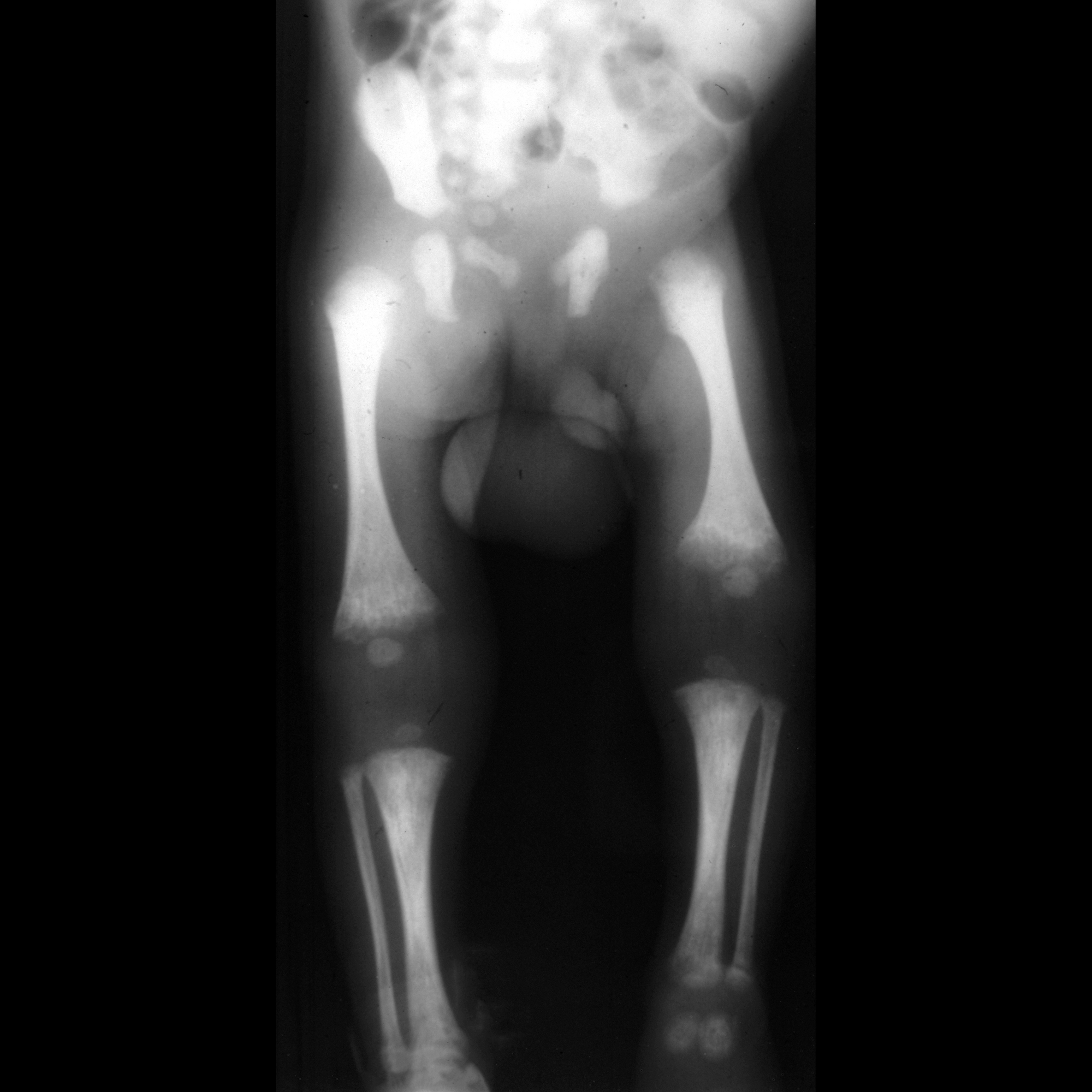
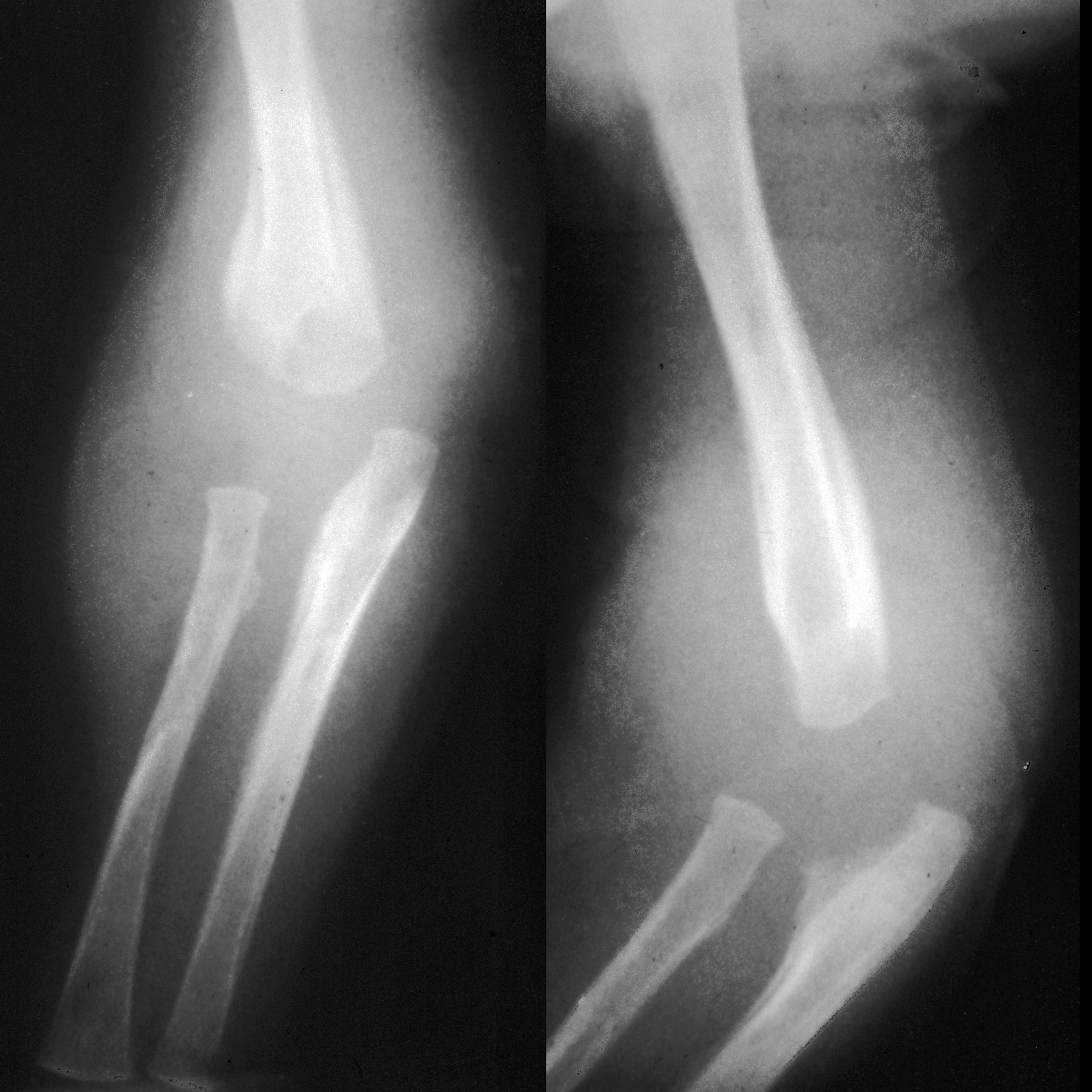
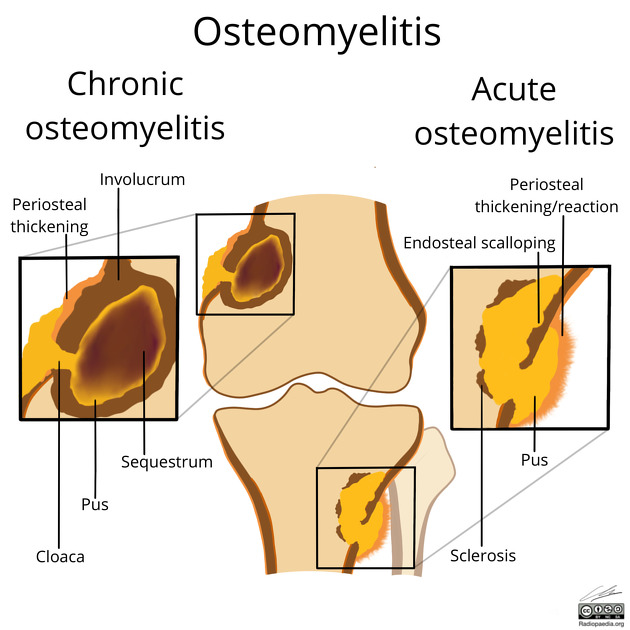
Plain radiograph
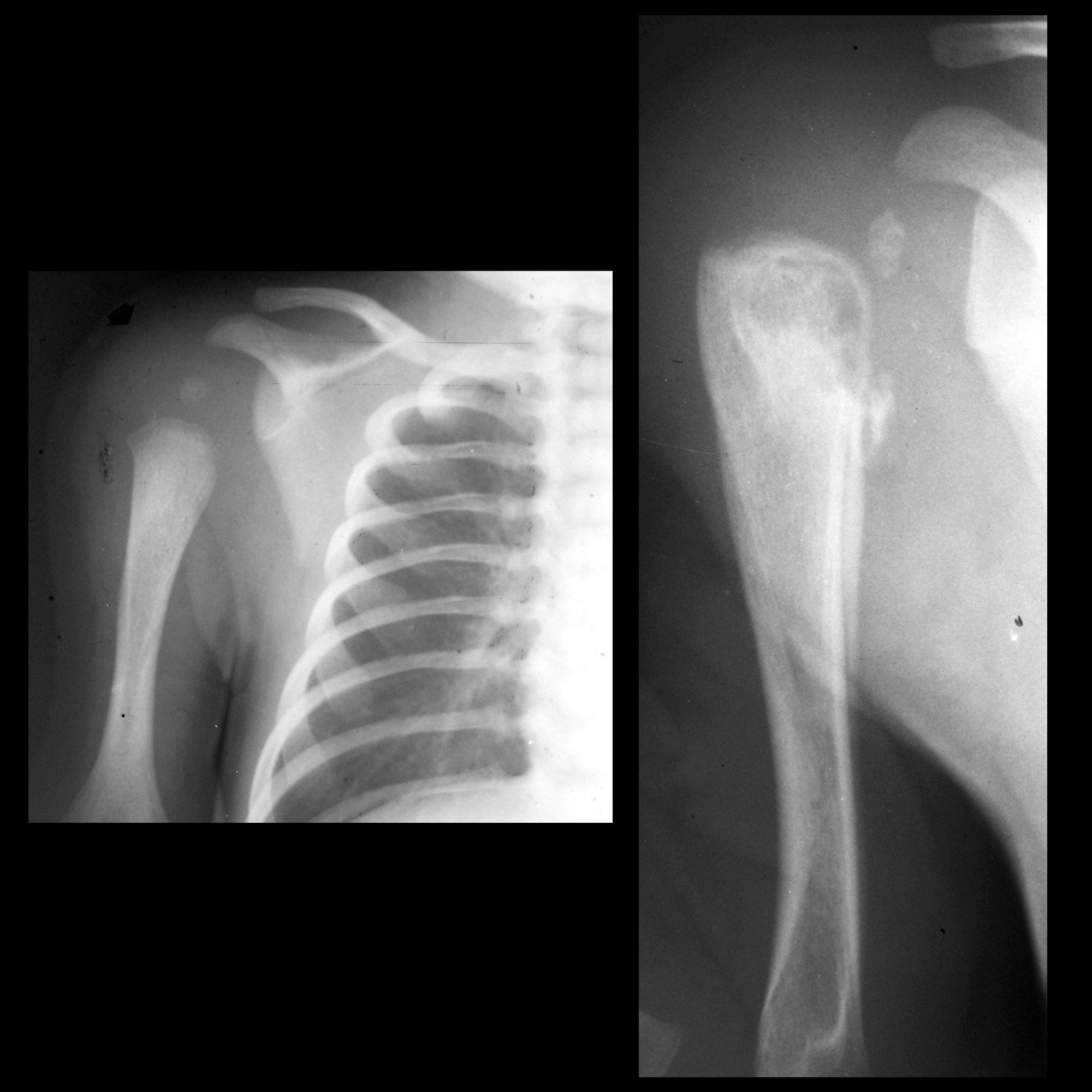
The earliest changes are seen in adjacent soft tissues +/- muscle outlines with swelling and loss or blurring of normal fat planes. An effusion may be seen in an adjacent joint.
In general, osteomyelitis must extend at least 1 cm and compromise 30 to 50% of bone mineral content to produce noticeable changes on plain radiographs. Early findings may be subtle, and changes may not be obvious until 5 to 7 days from onset in children and 10 to 14 days in adults. On radiographs taken after this time period, a number of changes may be noted:
- regional osteopenia
- periosteal reaction/thickening (periostitis): variable; may appear aggressive, including the formation of a Codman's triangle
- focal bony lysis or cortical loss
- endosteal scalloping
- loss of trabecular bone architecture
- new bone apposition
- eventual peripheral sclerosis
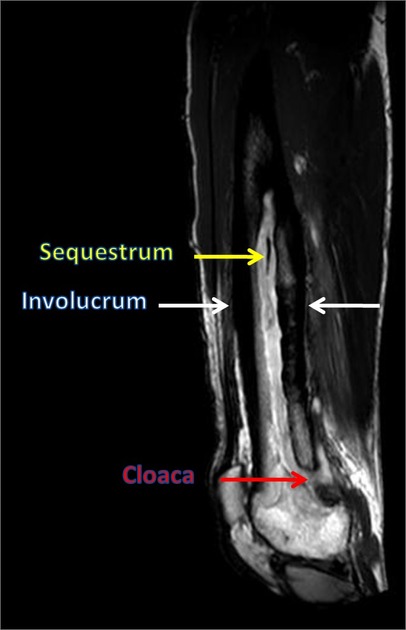
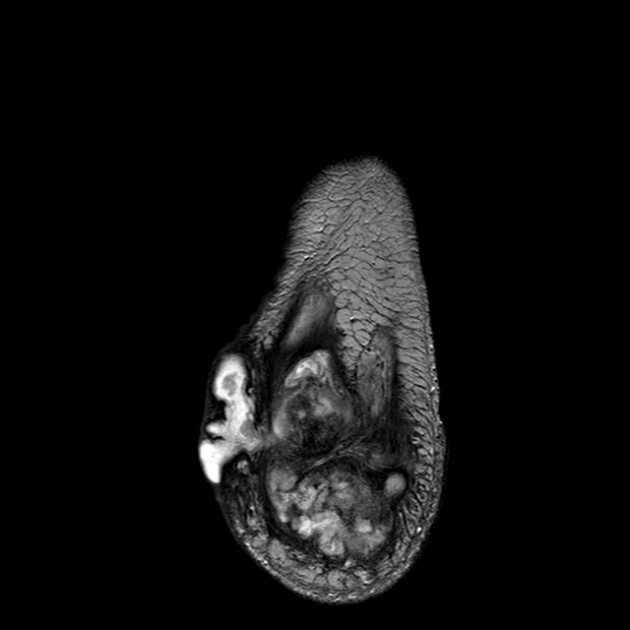
In chronic or untreated cases, eventual formation of a sequestrum, involucrum, and/or cloaca may be seen.
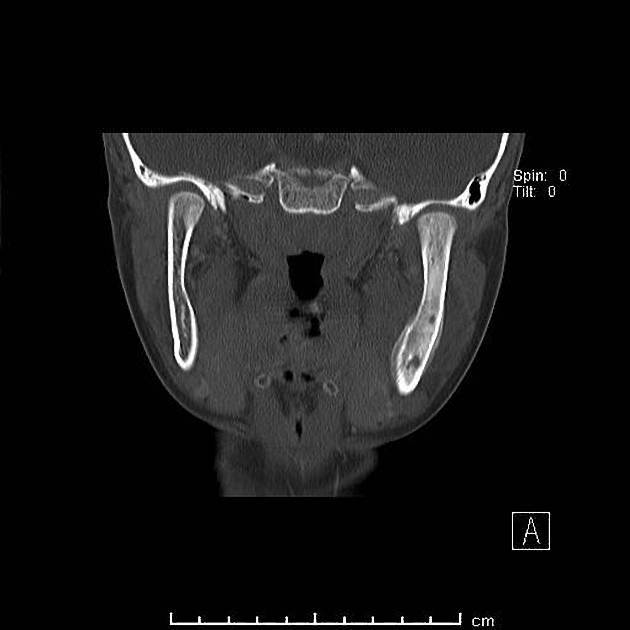
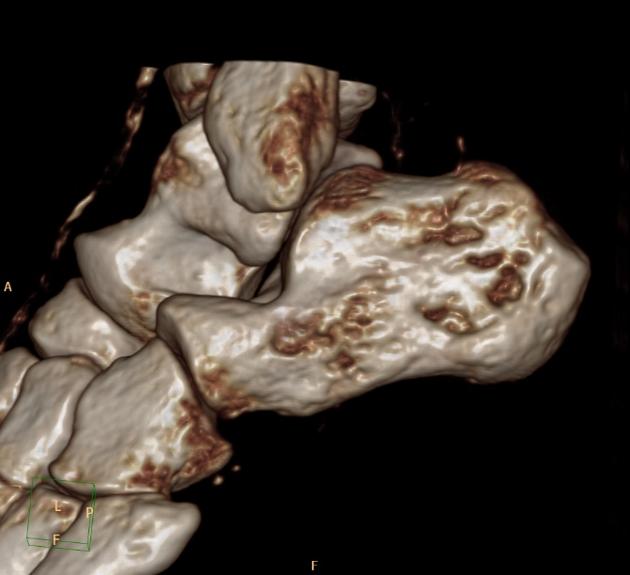
CT
CT is superior to both MRI and plain film in depicting the bony margins and identifying a sequestrum or involucrum. The CT features are otherwise similar to plain films. The overall sensitivity and specificity of CT is low, even in the setting of chronic osteomyelitis, and according to one study are 67% and 50%, respectively .
Some limitations CT include :
- inability to confidently detect marrow edema; therefore, a normal CT does not exclude early osteomyelitis.
- image degradation by streak artifact when metallic implants are present
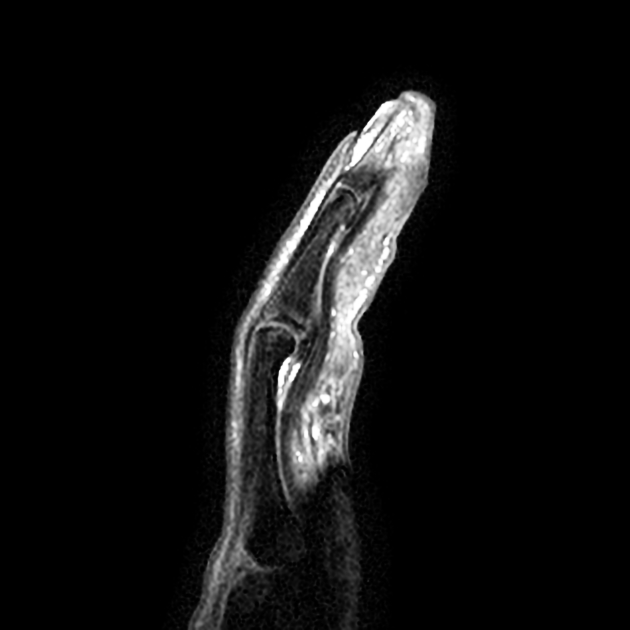
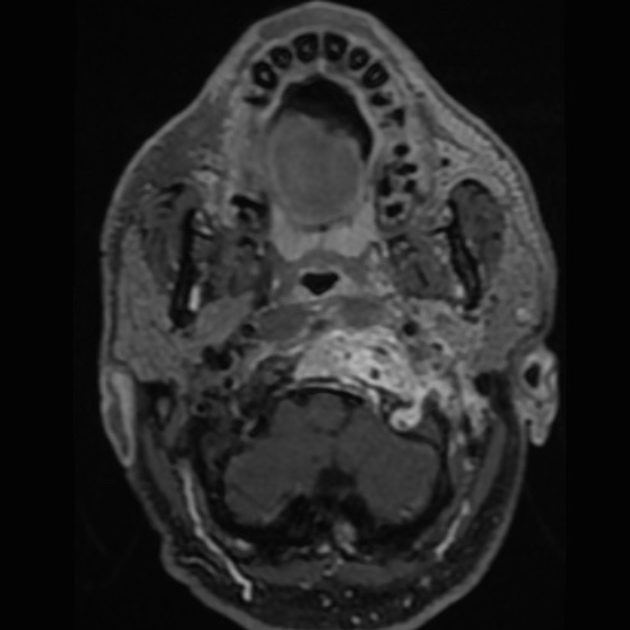
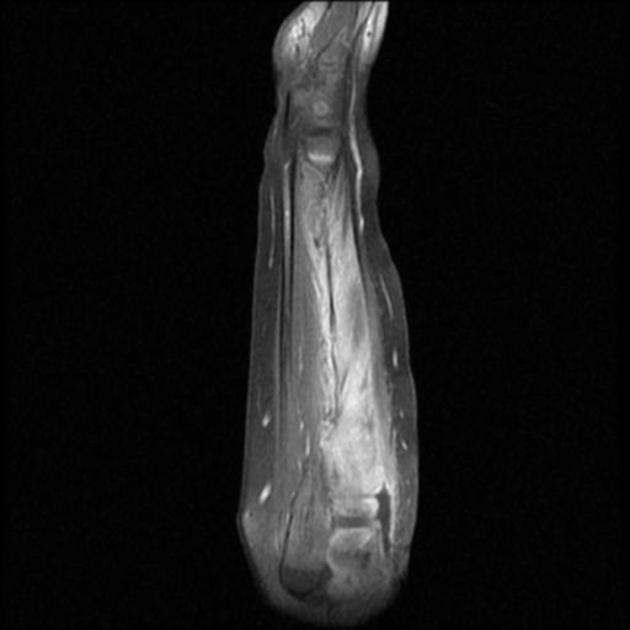
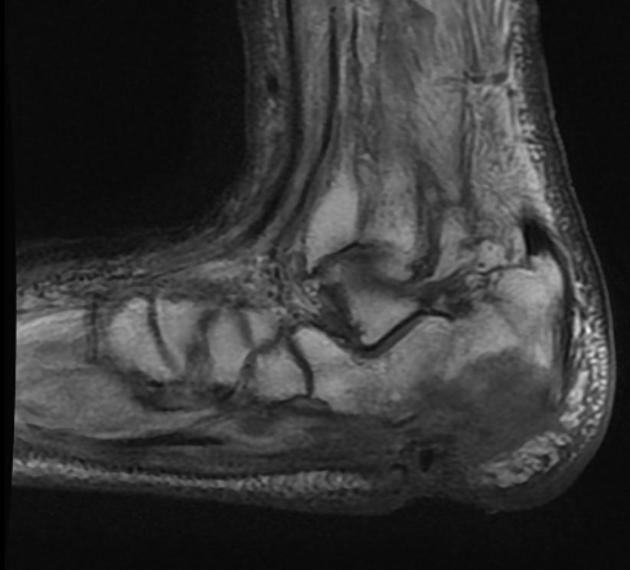
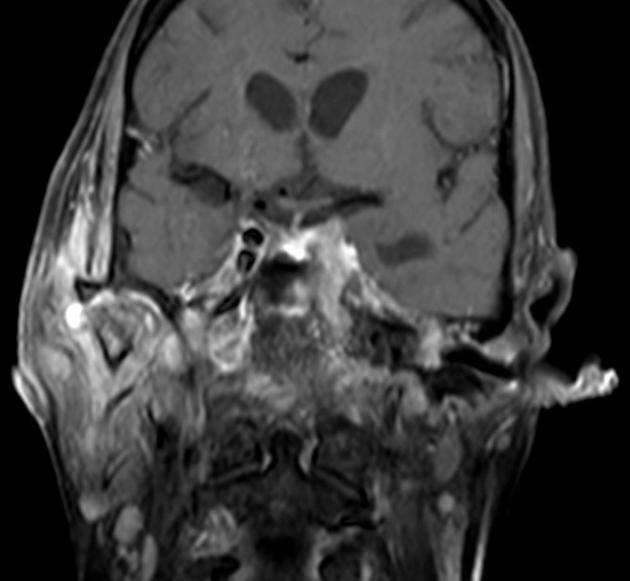
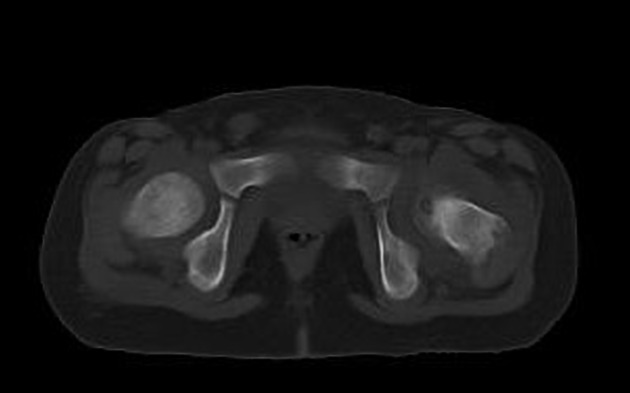
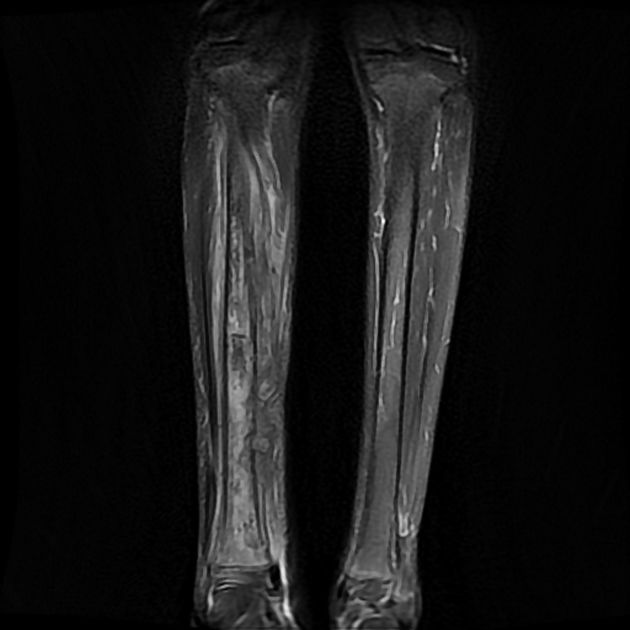
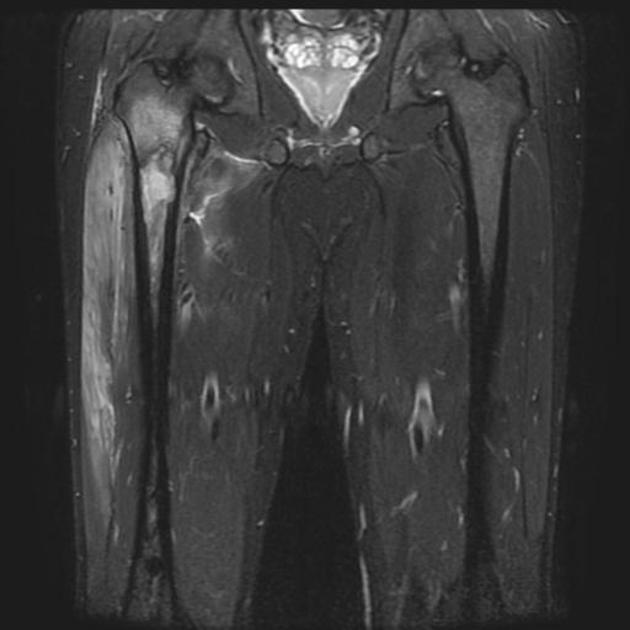
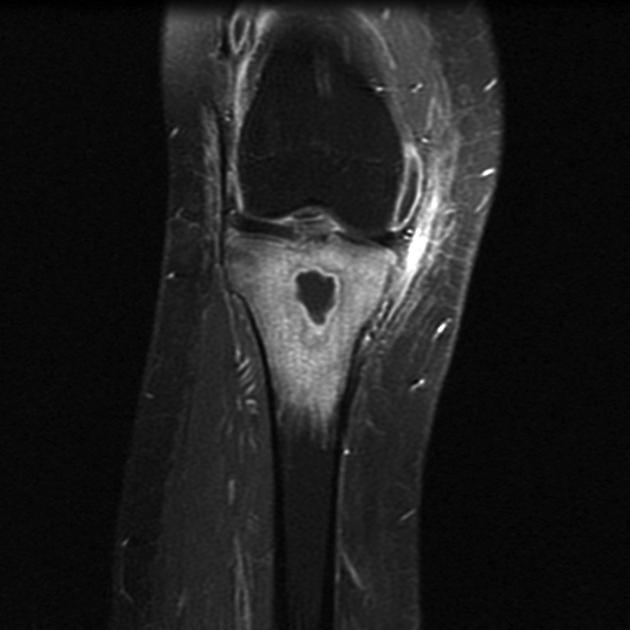
MRI
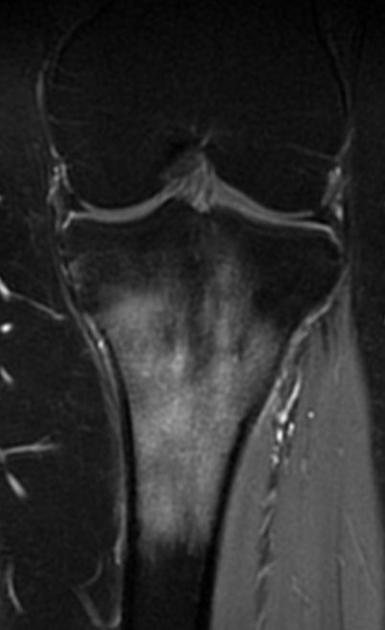
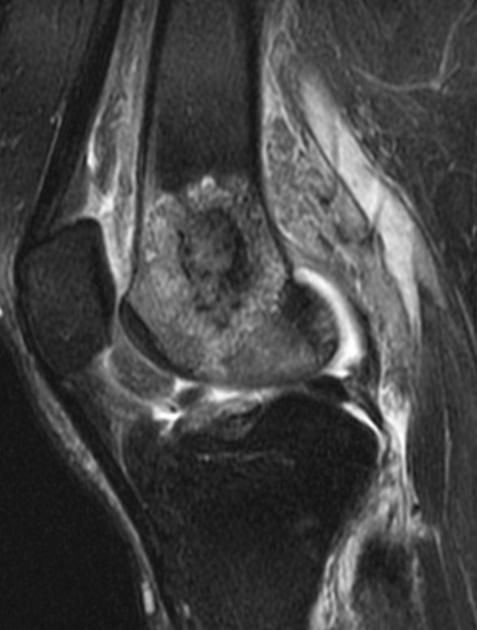
MRI is the most sensitive and specific and is able to identify soft-tissue/joint complications .
Bone marrow edema is the earliest feature of acute osteomyelitis seen on MRI and can be detected as early as 1 to 2 days after the onset of infection .
- T1
- intermediate to low signal central component (fluid)
- surrounding bone marrow of lower signal than normal due to edema
- cortical bone destruction
- T2
- bone marrow edema
- central high signal (fluid)
- T1 C+
- post-contrast enhancement of bone marrow, abscess margins, periosteum, and adjacent soft tissue collections
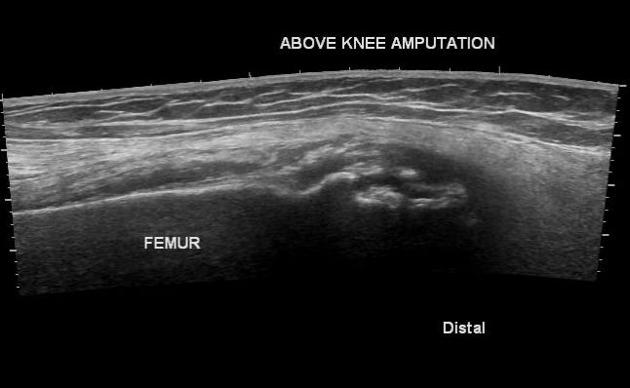
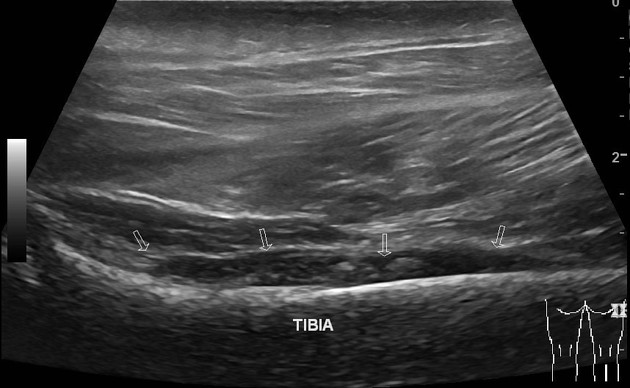
Ultrasound
Although ultrasound excels as a fast and inexpensive examination of the soft tissues and can guide the drainage of soft tissue collections, it has little role in the direct assessment of osteomyelitis, as it is unable to visualize within the bone.
It does, however, have a role in the assessment of soft tissues and joints adjacent to infected bone, as it can be used to visualize soft tissue abscesses, cellulitis, subperiosteal collections, and joint effusion.
Ultrasound is also useful in assessing the extraosseous components of orthopedic instrumentation, as it is not affected by metal artifacts .
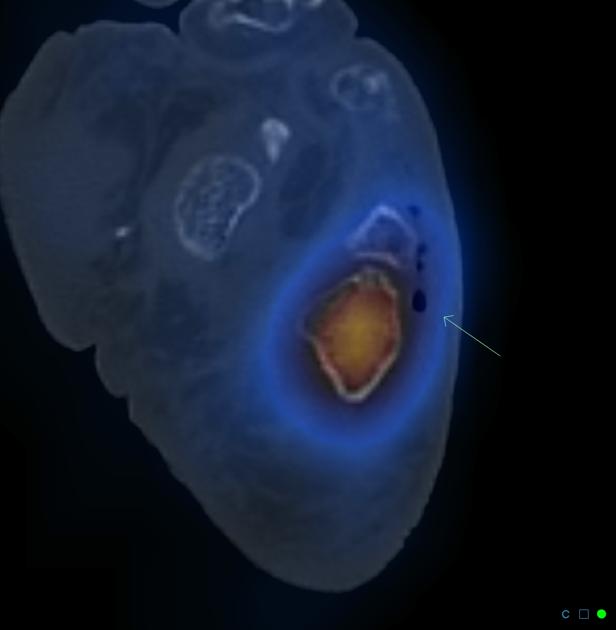
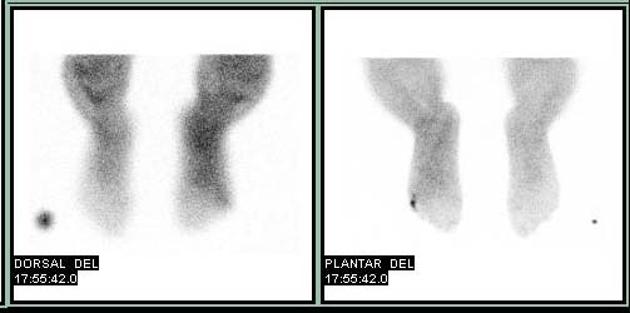
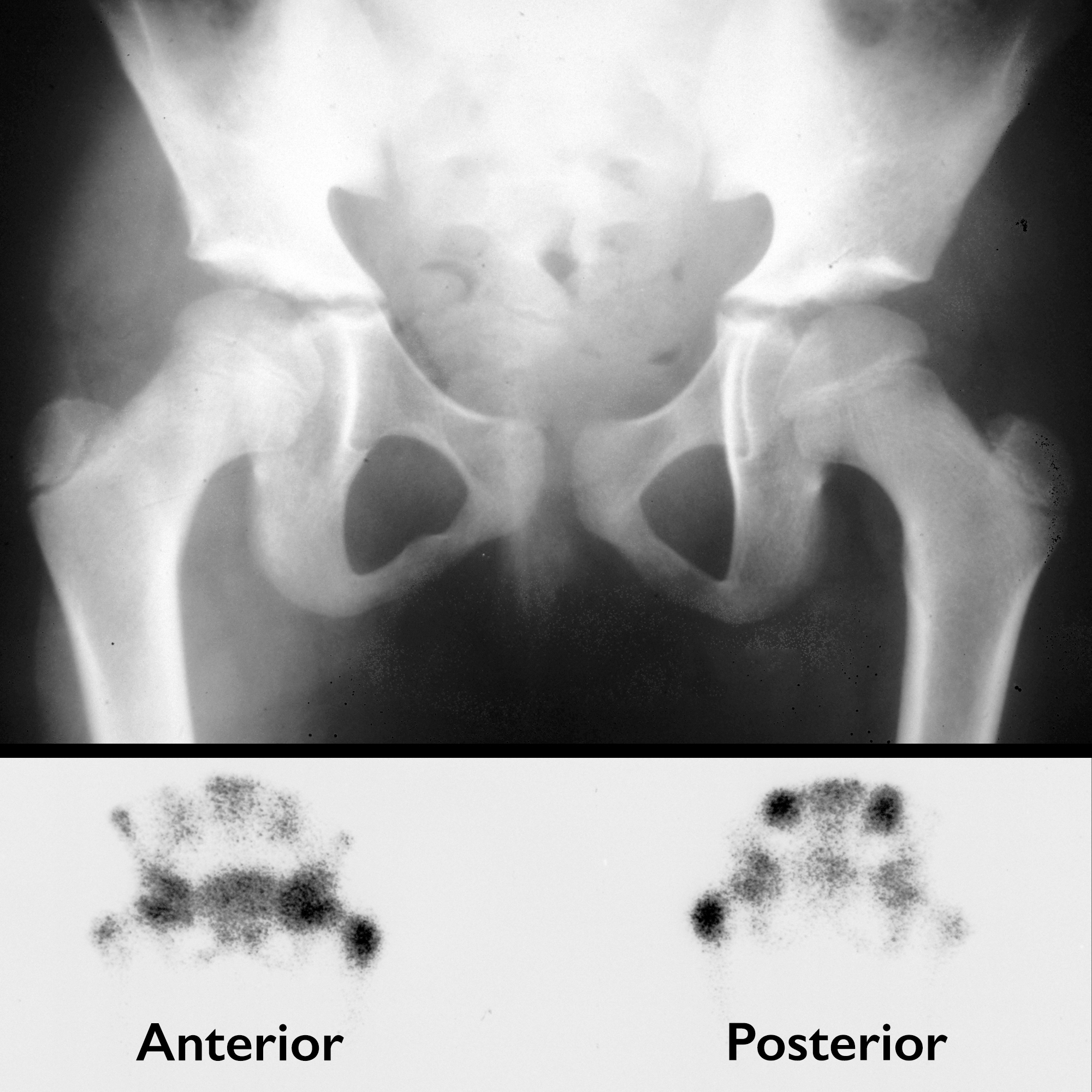
Nuclear medicine
A number of techniques may be employed to detect foci of osteomyelitis.
These include :
Bone scintigraphy (Tc-99m)
Increased osteoblastic activity results in increased levels of radiotracer uptake in the surrounding bone, usually both on blood pool and delayed views. It is highly sensitive but not particularly specific.
Indium-111labeled WBC scintigraphy
May be useful in cases of:
- diabetic osteomyelitis, especially combined with Tc-99m-phosphonate imaging ; however, MRI is now generally used in conjunction with plain films
- orthopedic implants
- vertebral osteomyelitis (Ga-67 is best)
- ulcers in bedridden patients with potential underlying osteomyelitis (In-111 with Tc-99m-phosphonate)
Gallium-67 scintigraphy
- radiogallium attaches to transferrin, which leaks from the bloodstream into areas of inflammation, showing increased isotope uptake in infection, sterile inflammatory conditions, and malignancy
- imaging is usually performed 18 to 72 hours after injection and is often performed in conjunction with radionuclide bone imaging
- one difficulty with gallium is that it does not show bone detail particularly well and may not distinguish well between bone and nearby soft tissue inflammation
- gallium scans may reveal abnormal accumulation in patients who have active osteomyelitis when technetium scans reveal decreased activity (“cold” lesions) or perhaps normal activity
- gallium accumulation may correlate more closely with inflammatory activity in cases of osteomyelitis than does technetium uptake
PET-CT
PET-CT systems are relatively novel techniques that are being applied. FDG-PET may have the highest diagnostic accuracy for confirming or excluding chronic osteomyelitis in comparison with bone scintigraphy, MRI, or leukocyte scintigraphy. It is also considered superior to leukocyte scintigraphy in detecting chronic osteomyelitis in the axial skeleton .
Treatment and prognosis
Treatment of osteomyelitis is typical with intravenous antibiotics, often for extended periods. If a collection, sequestrum, or involucrum is present, drainage and/or surgical debridement is often necessary. Amputation is performed after failure of medical therapy or when the infection is life-threatening.
Complications include :
- sinus tract formation with occasional superimposed squamous cell carcinoma (Marjolin ulcer)
- secondary sarcoma (e.g. osteosarcoma): rare
- pathological fracture
- secondary amyloidosis
Differential diagnosis
General imaging differential considerations include:
- Charcot joint
- metastases
- primary bone neoplasm
- Langerhans cell histiocytosis (LCH)

 Assoziationen und Differentialdiagnosen zu Osteomyelitis:
Assoziationen und Differentialdiagnosen zu Osteomyelitis: