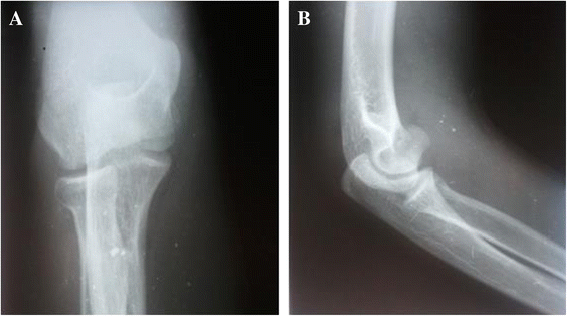
Osteonekrose der Trochlea humeri
Osteonekrose der Trochlea humeri
Aseptische Knochennekrose Radiopaedia • CC-by-nc-sa 3.0 • de
Osteonecrosis is a generic term referring to the ischemic death of the constituents of bone. It has a wide variety of causes and can affect nearly any bone in the body. Most sites of involvement have an eponym associated with osteonecrosis of that area, and these sites are discussed individually as each site has unique clinical, etiologic and prognostic features.
Terminology
Osteonecrosis vs avascular necrosis
Historically, the terms ischemic and avascular necrosis were typically reserved for subchondral (epiphyseal) osteonecrosis, whereas bone infarct referred to medullary (metaphyseal) osteonecrosis. The term avascular necrosis is usually seen in older publications. Osteonecrosis is a more general and inclusive term, and is now preferably used; it is also important to note that necrosis is always avascular. However, often both osteonecrosis and avascular necrosis are often used interchangeably, which can lead to confusion .
Epidemiology
There is no single affected demographic as the underlying predisposing factors are varied.
Pathology
Infarction begins when the blood supply to a section of bone is interrupted. Once an infarct has become established, just as in other tissues, there is a central necrotic core, surrounded by an ischemic zone, the inner portion being 'almost dead' and the outer portion being hyperemic. Beyond this is normal viable marrow. Between the normal and the ischemic zone that demarcation occurs with the development of viable granulation separating dead tissue. This leads to the double line sign on MRI.
When the infarct is subchondral, a wedge of tissue is typically affected, the apex of which points towards the center of the bone.
Etiology
- trauma (fracture or dislocation)
- caisson disease
- hemoglobinopathies, e.g. sickle cell disease
- pregnancy-related osteonecrosis
- radiotherapy
- connective tissue disorders
- renal transplantation
- corticosteroid excess (both endogenous and exogenous)
- pancreatitis
- gout
- Gaucher disease
- alcohol
- cirrhosis
- Freiberg disease
- chemotherapy
Mnemonics: STARS, PLASTIC RAGS
Eponymous names for specific sites of avascular necrosis
- Ahlback disease: medial femoral condyle, i.e. SONK
- Brailsford disease: head of the radius
- Buchman disease: iliac crest
- Burns disease: distal ulna
- Caffey disease: entire carpus or intercondylar spines of the tibia
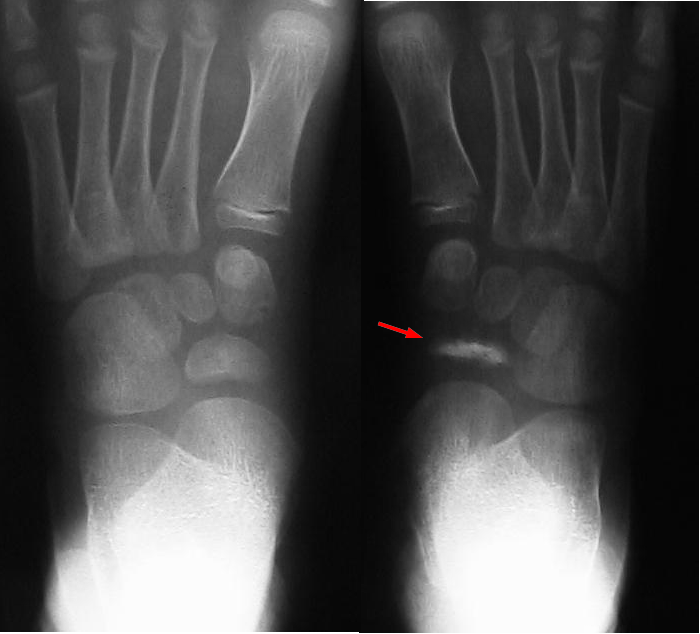
- Dias disease: trochlea of the talus
- Dietrich disease: head of metacarpals
- Freiberg infraction: head of the second metatarsal
- Friedrich disease: medial clavicle
- Hass disease: humeral head
- Iselin disease: base of 5metatarsal
- Kienböck disease: lunate
- Köhler disease: patella or navicular (children)
- Kümmell disease: vertebral body
- Legg-Calvé-Perthes disease: femoral head
- Mandl disease: greater trochanter
- Mauclaire disease: metacarpal heads
- Milch disease: ischial apophysis
- Mueller-Weiss disease: navicular (adult)
- Panner disease: capitellum of the humerus
- Pierson disease: symphysis pubis
- Preiser disease: scaphoid
- Sever disease: calcaneal epiphysis
- Siffert-Arkin disease: distal tibia
- Thiemann disease: base of phalanges
- van Neck-Odelberg disease: ischiopubic synchondrosis
Location-specific subarticles for avascular necrosis
Radiographic features
Radiographic changes alter with the stage of osteonecrosis - see Ficat staging, Steinberg classification, ARCO classification.
Radiograph
Plain radiographs are negative in early disease. In general, there is initial minor osteopenia, followed by variable changes, such as patchy sclerosis and rim calcification. Gradually microfractures of the subchondral bone accumulate in the dead bone, which is unable to repair leading to the collapse of the articular surface and the crescent sign of osteonecrosis. Eventually the cortex collapses and fragments, with superimposed secondary degenerative change.
MRI
MRI is the most sensitive (~95%) modality and demonstrates changes well before plain films changes are visible.
- reactive interface line: focal serpentine low signal line with fatty center (most common appearance and first sign on MRI)
- double line sign: T2WI serpentine peripheral/outer dark (sclerosis) and inner bright (granulation tissue) line is diagnostic (the line extends usually to the subchondral bone plate, which helps to differentiate it from subchondral fracture)
- diffuse edema: edema is not an early sign; instead, studies show that edema occurs in advanced stages and is directly correlated with pain
- rim sign: osteochondral fragmentation
- secondary degenerative change (i.e. osteoarthritis)
- on contrast-enhanced images non-viable marrow does not enhance
- in case of radiation necrosis, there is edema or fatty replacement of the adjacent bone marrow (depending on the interval between the examination and radiotherapy)
Nuclear medicine
Bone scintigraphy is also quite sensitive (~85%) and is the second option after MRI. It is a choice when multiple sites of involvement must be assessed in patients with risk factors, such as sickle cell disease. The findings are different accordingly to the time of the scan:
- early disease: often represented by a cold area likely representing the vascular interruption
- late disease: may show a "doughnut sign": a cold spot with surrounding high uptake ring (surrounding hyperemia and adjacent synovitis)
Treatment and prognosis
The goal of treatment is to reduce the load on the affected part and to promote revascularization. Treatment varies by location and includes:
- conservative: anti-inflammatory, analgesia, and reduced/non-weight bearing
- core decompression
- joint replacement for end-stage disease
Practical points
- MRI and bone scintigraphy have high sensitivity, with MRI studies being the first line for the assessment of osteonecrosis
See also
Siehe auch:
- Aseptische Knochennekrose
- Aseptische Nekrose des Capitulum humeri
- isolierte Fraktur des Trochlea humeri
und weiter:

 Assoziationen und Differentialdiagnosen zu Osteonekrose der Trochlea humeri:
Assoziationen und Differentialdiagnosen zu Osteonekrose der Trochlea humeri: