Pigmentierte villonoduläre Synovialitis Schulter

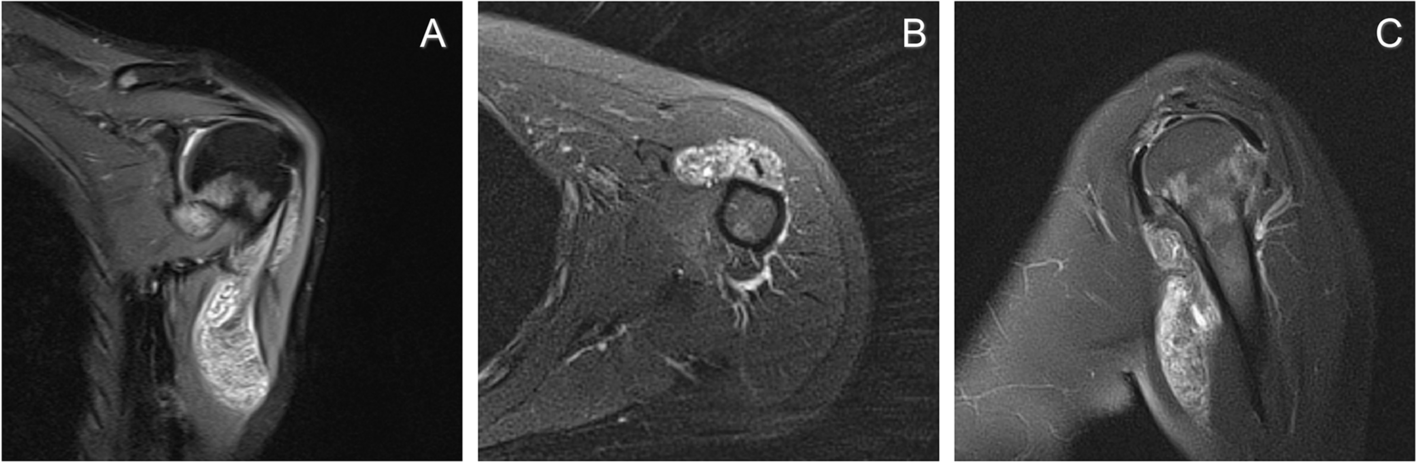
Pigmentierte villonoduläre Synovialitis Schulter
Pigmentierte villonoduläre Synovialitis Radiopaedia • CC-by-nc-sa 3.0 • de
Pigmented villonodular synovitis (PVNS) is a rare benign proliferative condition affecting synovial membranes of joints, bursae or tendons resulting from possibly neoplastic synovial proliferation with villous and nodular projections and hemosiderin deposition. PVNS is most commonly monoarticular (~70% knee joint) but occasionally it can be oligoarticular. The histology of PVNS can look similar to some aggressive neoplasms (rhabdomyosarcoma, synovial sarcoma, epithelioid sarcoma) and imaging, therefore, has a crucial role in guiding the pathologist.
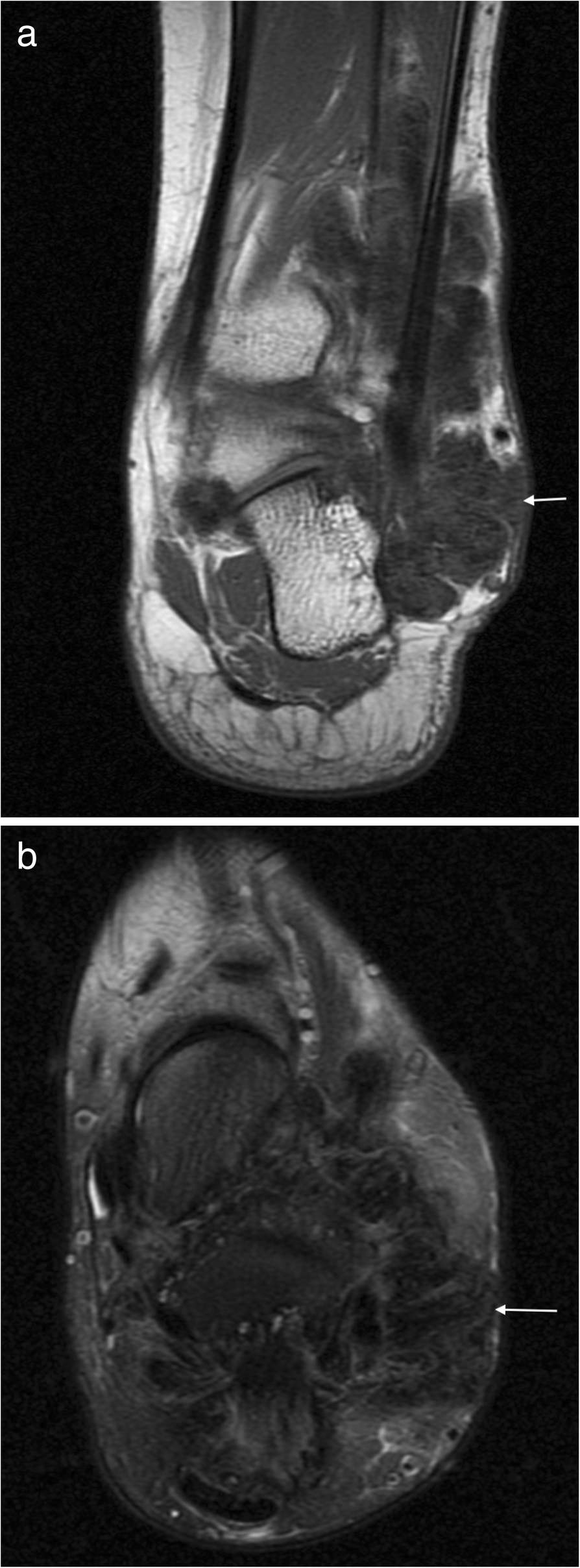
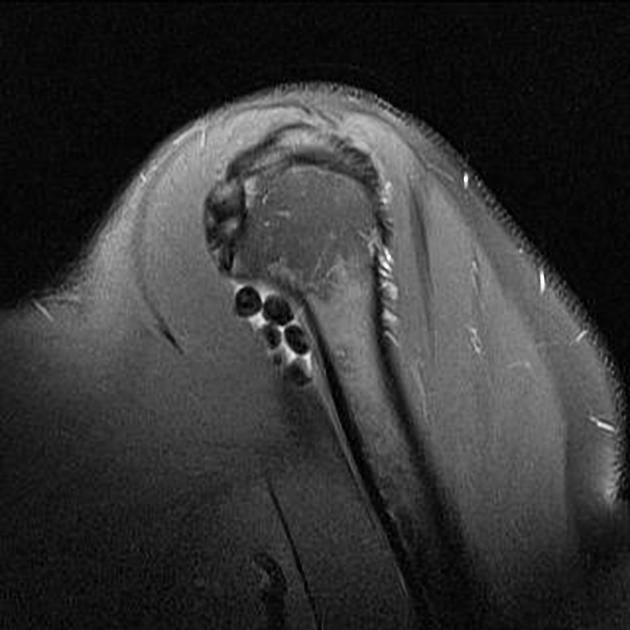
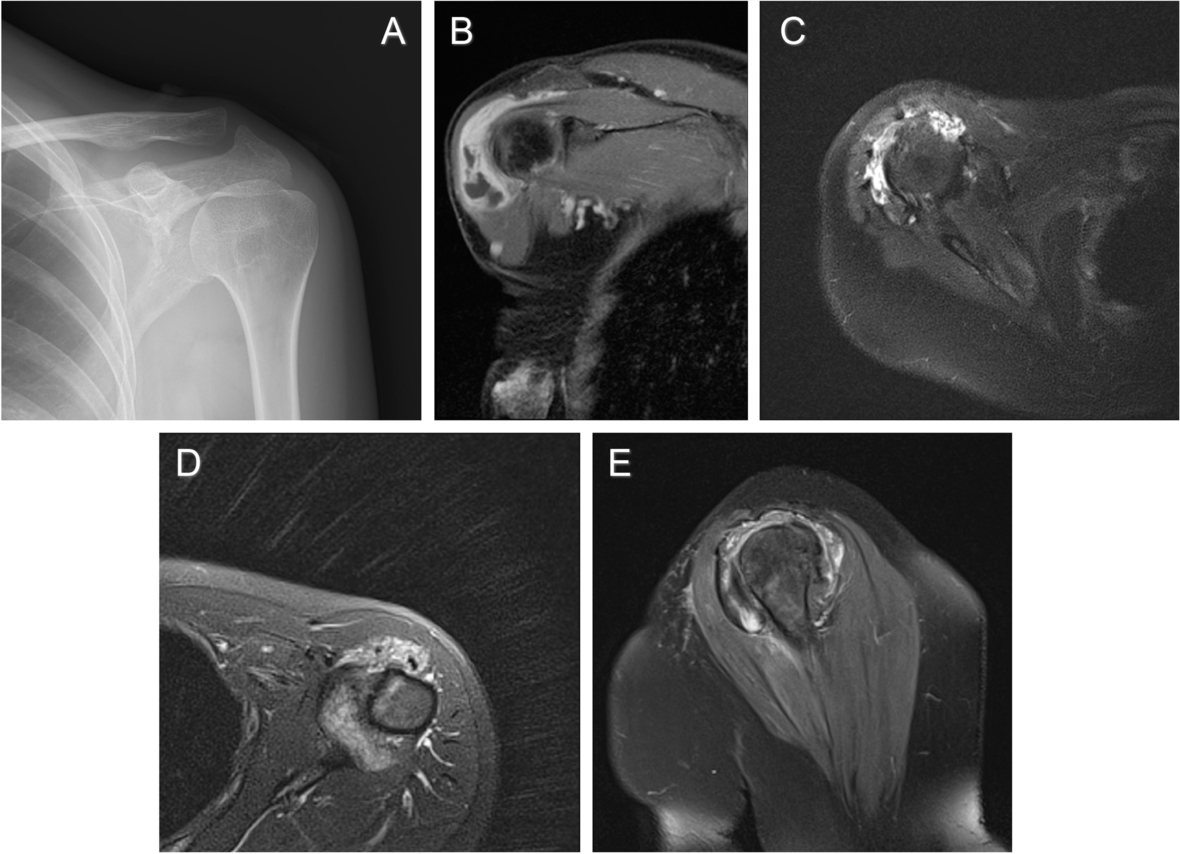
Radiographs show non-specific features such as joint effusion and bone erosions, CT and ultrasound can also demonstrate the hypertrophic synovium as a slightly hyperdense/echogenic soft tissue mass. MRI is the best approach showing the mass-like synovial proliferation with lobulated margins, with low signal intensity and “blooming” artifact on gradient echo due to hemosiderin deposition.
Epidemiology
PVNS occurs predominantly in the early to middle age (2 to 5 decades) . In intra-articular disease, there is no gender predilection, whereas extra-articular disease has a slight female predominance.
Clinical presentation
Presentation is usually with joint swelling, pain and occasionally joint dysfunction. Usually, symptoms have been present for many months before the diagnosis is made.
Although unusual in the pediatric population, it is sometimes seen and is more frequently poly-articular. It has also been described in association with :
- cherubism
- extremity lymphedema
- mandibular lesions
- multiple lentigines syndrome
- Noonan syndrome
- vascular lesions
Pathology
Traditionally, most authors believed that PVNS is a result of reactive chronic inflammation but the capability of these lesions for autonomous growth, the malignant transformation potential, and recently found constant cytogenetic aberrations in most cases are suggesting that PVNS has a neoplastic origin .
Malignant transformation of PVNS is rare, and controversy exists as to histologic criteria for its diagnosis.
Macroscopic appearance
Macroscopically the synovium is diffusely thickened with multiple villous and nodular projections. Their color is typically dark brown and heterogeneous with areas of yellow discolouration (xanthoma cells).
Histology
On microscopy, mononuclear histiocytes predominate mixed in with variable numbers of multinucleated giant cells (absent in 20% of cases). Overall there is a diffuse infiltrative growth pattern . It is important to note that histologically the appearance of PVNS may mimic aggressive neoplasms such as rhabdomyosarcoma, synovial sarcoma, or epithelioid sarcoma, and thus the role of imaging in guiding the pathologist is crucial.
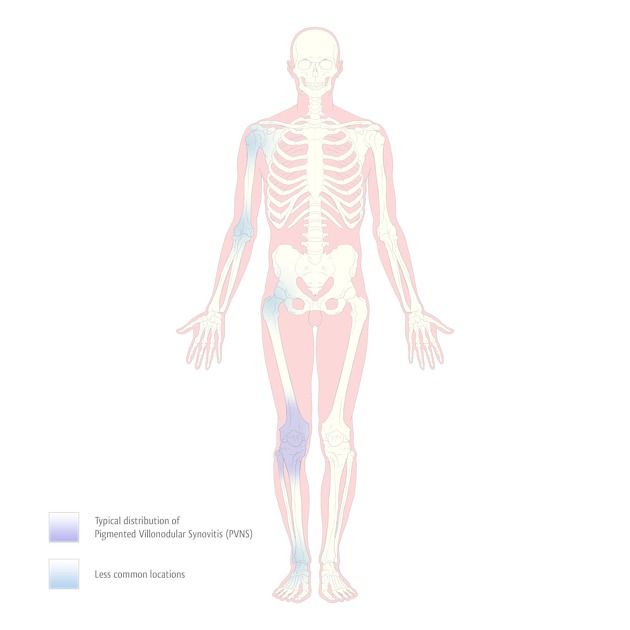
Location
- knee (by far the most frequently affected joint ): 66-80%
- hip: 4-16%
- ankle
- shoulder
- elbow
- spine
- other joints
Classification
All synovial membranes may be affected, and pathologists tend to classify the spectrum of histologically identical entities under the umbrella of tenosynovial giant cell tumor. Other sites with a synovial lining that may be affected include bursae and tendon sheaths. The condition is then known as pigmented villonodular bursitis (PVNB) when in a bursa and tenosynovial giant cell tumor when in a tendon sheath.
PVNS/B/TS are divided into a localized and diffuse form:
- localized: most common and usually extra-articular (PVNB and PVNTS)
- diffuse (i.e. involves all of the contiguous synovium): is the most common form of an intra-articular disease, although local intra-articular involvement is also sometimes seen
Typically PVNS is a monoarticular condition and joints with large synovial surfaces are predictably most frequently affected. The remainder of this article focuses on intra-articular disease (PVNS).
Radiographic features
Plain radiograph
On radiographs, features are relatively nonspecific with appearances mainly being those of a joint effusion. Bone density and joint space are preserved until the late stages. No calcification is seen. Extrinsic marginal pressure erosions may be present, but it is not possible to distinguish PVNS from synovial chondromatosis (non-ossified synovial osteochondromatosis). There may be suggestion of focal areas of soft tissue swelling surrounding the joint +/- dense soft-tissues from hemosiderin deposition.
CT
Joint effusions commonly co-exist. The hypertrophic synovium appears as a soft tissue mass, which on account of hemosiderin, may appear slightly hyperdense compared to adjacent muscle. Calcification is very rare in the synovial mass (cf. synovial sarcoma where it is common). Erosions are often well seen on CT.
MRI
MRI typically shows mass-like synovial proliferation with lobulated margins. This may be extensive in the diffuse form or limited to a well-defined single nodule in the localized form with low signal intensity due to hemosiderin deposition.
Signal characteristics include:
- T1: low to intermediate signal
- T1 C+ (Gd): variable enhancement
- T2
- low to intermediate signal
- some areas of high signal may be present likely due to joint fluid or inflamed synovium
- STIR: predominantly high signal
- GE: low and may demonstrate blooming
Treatment and prognosis
Treatment is with complete synovectomy, which offers a good prospect of cure, provided all the synovium is excised. This can be difficult and therefore adjuvant treatment is often employed, especially external beam radiotherapy which offers excellent control. Intra-articular injection of yttrium-90 is an alternative.
Medical therapy is also being investigated in refractory cases including α-TNF (tumor necrosis factor) blockade and infliximab.
Recurrence rates after total synovectomy are reported to be ~15% (range 7-20%) .
History and etymology
The term PVNS was first proposed by Jaffe et al. in 1949 . The first description of the condition was by Chassaignac in 1852 who had described a nodular lesion of the synovial membrane that affected the flexor tendons of the fingers .
Differential diagnosis
On MRI there is little differential in classic examples:
- scarring/capsulitis
- siderotic synovitis
On plain film the differential is wide, and findings are non-specific:
- joint effusion
- synovial chondromatosis (non-ossified)
- lipoma arborescens
Practical points
- calcification, in essence, excludes the diagnosis of PVNS
- gradient echo is the key sequence, showing low signal and blooming
See also
Siehe auch:
 Assoziationen und Differentialdiagnosen zu Pigmentierte villonoduläre Synovialitis Schulter:
Assoziationen und Differentialdiagnosen zu Pigmentierte villonoduläre Synovialitis Schulter: