Schädel-Hirn-Trauma




Traumatic brain injuries (TBI) are common and come with a large cost to both society and the individual. The diagnosis of traumatic brain injury is a clinical decision, however, imaging, particularly CT, plays a key role in diagnostic work-up, classification, prognostication and follow-up.
They can be broadly divided into closed and penetrating head injuries :
- closed head injury
- vastly more common
- blunt trauma: motor vehicle collision, assault, sport, industrial/workplace accidents, etc.
- blast injuries
- non-accidental injury in children
- penetrating head injury
- high-velocity penetrating brain injury e.g. gunshot injuries
- low-velocity penetrating brain injury e.g. stabbing
The remainder of this article focuses on closed head injury.
Epidemiology
Traumatic brain injuries are more common in young patients, and men account for the majority (75%) of cases . Although sport is a common cause of relatively mild repeated head injury potentially eventually leading to chronic traumatic encephalopathy, more severe injuries are most often due to motor vehicle accidents and assault.
Clinical presentation
Patients typically present with a combination of reduced Glasgow Coma Scale (GCS), nausea/vomiting and/or amnesia . The severity of the injury can be assessed with GCS :
- mild traumatic brain injury (TBI): GCS 14-15
- moderate TBI: GCS 9-13
- severe TBI: GCS 3-8
This scale has limitations as there are other causes for reduced GCS in trauma (alcohol, drugs, seizure, etc.).
The term concussion refers to a clinical diagnosis which has overlap with the mild end of the spectrum of traumatic brain injury, and usually is used in reference to a transient brain injury .
The potential long term sequelae of repetitive traumatic brain injury is a current area of research. Chronic traumatic encephalopathy describes neurodegeneration associated with repetitive head injuries, and characterized microscopically by accumulation of hyperphosphorylated tau in neurons.
Pathology
In the acute setting patients can present with primary brain damage :
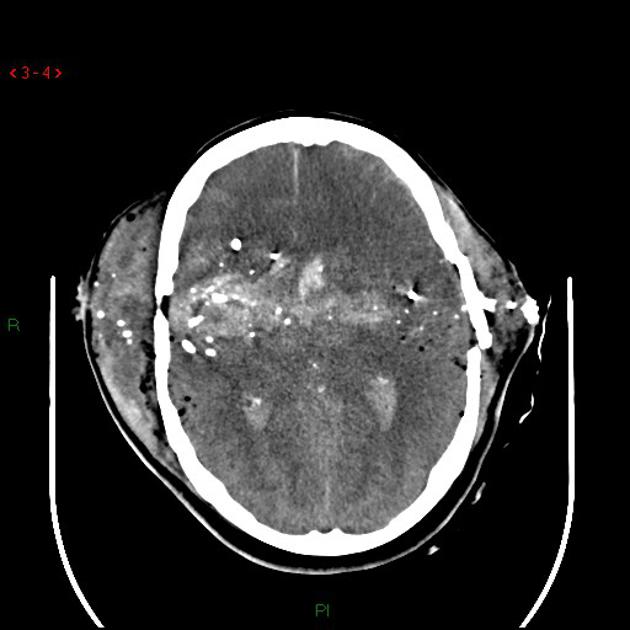
- traumatic subarachnoid hemorrhage (tSAH)
- subdural hematoma (SDH)
- extradural hematoma (EDH)
- intraventricular hemorrhage
- cerebral hemorrhagic contusion
- diffuse axonal injury (DAI)
Secondary brain damage can also occur and manifests as :
- generalized cerebral edema
- hypoxic-ischemic brain injury
- ischemic stroke from traumatic arterial dissection
- "big black brain"
Long-term sequelae of head trauma include:
- encephalomalacia/gliosis
- chronic subdural hematomas / CSF hygromas
- chronic traumatic encephalopathy
- depression, anxiety and alcohol excess
- increased risk of schizophrenia, bipolar disorder and organic mental disorders
Complications
Severe mass effect can result in:
- midline shift: associated with worse prognosis
- cerebral herniation: often requires urgent treatment
- hydrocephalus: can also be a chronic non-mass effect related complication
Associations
Other traumatic injuries are common:
- cervical spine injury: patients with GCS <8 are most at risk
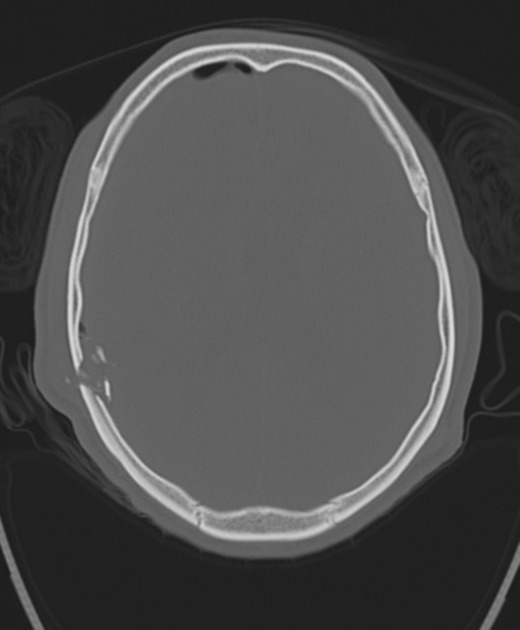
- skull fracture
- facial fracture
- pneumocephalus
- extracranial injuries in 35%
Imaging indications
The decision to perform imaging in the setting of head trauma will depend on multiple factors, including local department guidelines and access to imaging. Various clinical tools exist which help to screen for patients who require acute neuro-imaging, including: the Canadian Head CT Rule, the National Emergency X-Radiography Utilization study II (NEXUS-II) criteria, and the American College of Radiology Appropriateness Criteria for head trauma.
Potential indications for performing CT in the acute setting for patients with concussion (to exclude more serious forms of traumatic brain injury such as intracranial hemorrhage) may include the following: loss of consciousness, post-traumatic amnesia, persistent altered mental status, focal neurology, signs of skull fractures or evidence of clinical deterioration .
Radiographic features
- skull fracture
- may be associated with tearing of the underlying meninges and extra-axial hemorrhage
- anterior cranial fossa fractures are often associated with CSF leak
- fractures traversing the dural venous sinus or jugular bulb are often associated with injuries to the venous structures (e.g. compression from an extra-axial hematoma and/or thrombosis)
- extradural hematoma
- subdural hematoma (SDH)
- mixed-attenuation SDH are not necessarily acute on chronic; other causes of hypoattenuating portions of subdural hematomas include hyperacute hemorrhage and unclotted chronic blood products (particularly in patients with coagulopathy) .
- subdural hygroma
- caused by tearing of the arachnoid membrane with CSF accumulation in the subdural space.
- can occur in the first day of trauma, but mean time to appearance is 9 days after injury .
- traumatic SAH
- usually small volume sulcal SAH occurring at the site of impact (coup) or opposite the site of impact (contrecoup).
- midline traumatic SAH in the inter-hemispheric fissure or perimesencephalic cisterns may be a marker of diffuse axonal injury. SAH in the interpeduncular cisterns may indicate brainstem injury.
- isolated SAH in the basilar cisterns may require investigation for underlying vascular aneurysm.
- intraventricular hemorrhage
- in the setting of trauma, this may occur from a ruptured subependymal vein, extension from intra-parenchymal hemorrhage or retrograde distribution from the subarachnoid space.
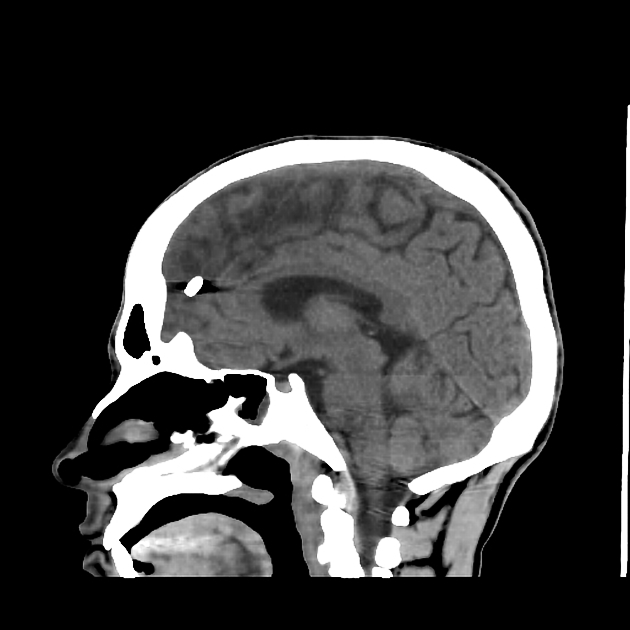
- brain contusion
- commonly at the inferior frontal lobes and anterior-inferior temporal lobes due to the ridged morphology of the inner table.
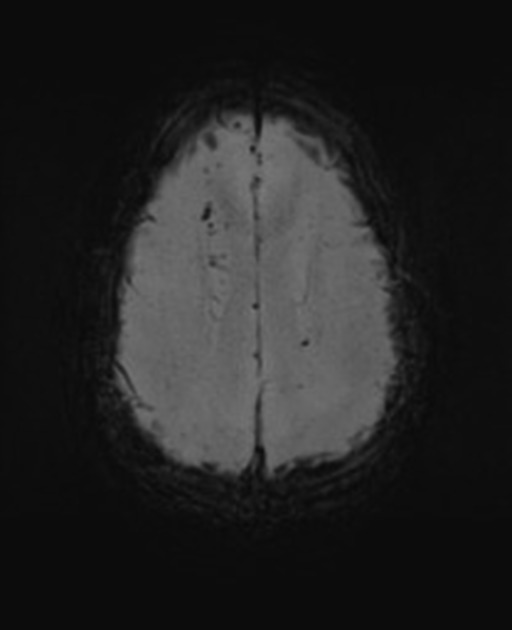
- axonal injury
- results from axonal stretch or shear stress, usually affecting organized white matter tracts (e.g. corpus callosum, internal capsule, dorsal midbrain or pons) or the grey-white matter interface (particularly in the frontal lobes).
- more sensitively detected on MRI. May be associated with restricted diffusion. Imaging often underestimate the full extent of axonal injury present
- can be hemorrhagic or non-hemorrhagic.
- graded in order of increasing severity;
- grade 1: involves subcortical white matter
- grade 2: involves corpus callosum
- grade 3: involves the brainstem
- thalamic lesions are not included in grading system but are associated with a poor prognosis when present .
- diffuse cerebral edema
- thought to be related to dysfunctional cerebral autoregulation or blood-brain barrier disruption; both vasogenic and cytotoxic edema may occur.
- vascular injuries
- arterial dissection (particularly in the setting of skull base fractures)
- pseudoaneurysm (most commonly involving the vertebral artery or anterior cerebral artery)
- extrvasation
- vascular occlusion
- traumatic carotid-cavernous fistula
- traumatic dural arteriovenous fistula
- venous thrombosis (particularly when a fracture traverses the dural venous sinus)
- second brain injuries and herniation
- subfalcine herniation, transtentorial herniation (unilateral or bilateral, downward or ascending), cerebellar tonsillar herniation
- various herniation patterns can also result in ventricular entrapment
CT
CT is the workhorse of imaging in TBI, especially in the acute setting, and is able to identify the majority of injuries at the time of presentation. It is common for multiple injuries to be present simultaneously, such as the combination of cerebral contusions and traumatic subarachnoid, subdural and extradural hemorrhage as well as skull fractures and facial fractures – these are discussed separately. Benefits of CT in the acute setting over MRI include increased sensitive for detection of fracture, vascular injury, CSF leak, and not needing to assess for MRI safety (particular in the setting of penetrating injury).
CT can also be used to formally classify the degree of injury using a formal scale (e.g. Marshall classification or Rotterdam CT score).
MRI
MRI has a supplementary role, especially in the evaluation of patients whose clinical condition do not match the CT findings (this can often occur in DAI) . MRI has increased sensitivity in detecting blood products (SAH, EDH, SDH and hemorrhagic contusions), non hemorrhagic cortical contusions, brain-stem injuries and axonal injuries . There is evidence to support the use of MRI in the setting of normal CT if there are persistent unexplained neurological findings and clinically traumatic brain injury is suspected. MRI is the preferred imaging modality in the setting of subacute or chronic traumatic brain injury with neurologic symptoms due to its higher sensitivity . Please see the relevant articles for imaging findings.
Treatment and prognosis
Large hematomas with significant mass effect require urgent neurosurgical evacuation. Hydrocephalus can develop and urgent ventricular drainage may be required. Intracranial pressure (ICP) monitor insertion is a common procedure used to help in the assessment of severe TBI.
Ongoing follow-up with CT is often required. In patients with diffuse injuries ~15% will develop new lesions, and ~35% (range 25-45%) of cerebral contusions will increase in size with progression thought to typically occur 6-9 hours after injury .
Siehe auch:
und weiter:

