Splenic abscesses

Splenic abscesses, like abscesses elsewhere, are localized collections of necrotic inflammatory tissue caused by bacterial, parasitic or fungal agents. They uncommonly affect the spleen due to its efficient reticuloendothelial system phagocytic activity and, consequently, are more likely seen in immunosuppressed patients.
Epidemiology
Splenic abscesses are uncommon, and their incidence in various autopsy series is estimated at ~0.4% (range 0.14-0.7%) . The frequency may be rising due to a rise in the use of immunosuppressive agents and prevalence of immunosuppressive states, higher survival of leukemic patients, and high incidence of drug abuse .
Clinical presentation
Splenic abscesses often present with vague, non-specific signs. Fever is common . Patients may present with left upper quadrant tenderness accompanied by rigors, chills, and vomiting. In most immunocompetent patients, a complete blood count will show marked leukocytosis with a left shift.
Pathology
The main causes of splenic abscesses include:
- immunodeficiency conditions (e.g. chemotherapy/transplant recipients, leukemia and AIDS): especially in those with multiple splenic abscesses
- infection: anaerobes are thought to be the most common infective agents
- metastatic infection
- haematogenous bacterial dissemination, such as sepsis
- infective endocarditis
- contiguous infection, such as from a perinephric abscess or infected necrotic pancreatitis
- metastatic infection
- splenic infarction with superimposed infection
- trauma
Radiographic features
Plain radiograph
A plain abdominal radiograph is insensitive in the evaluation of splenic abscesses. Indirect signs include gas within the abscess, and a reactive left-sided pleural effusion .
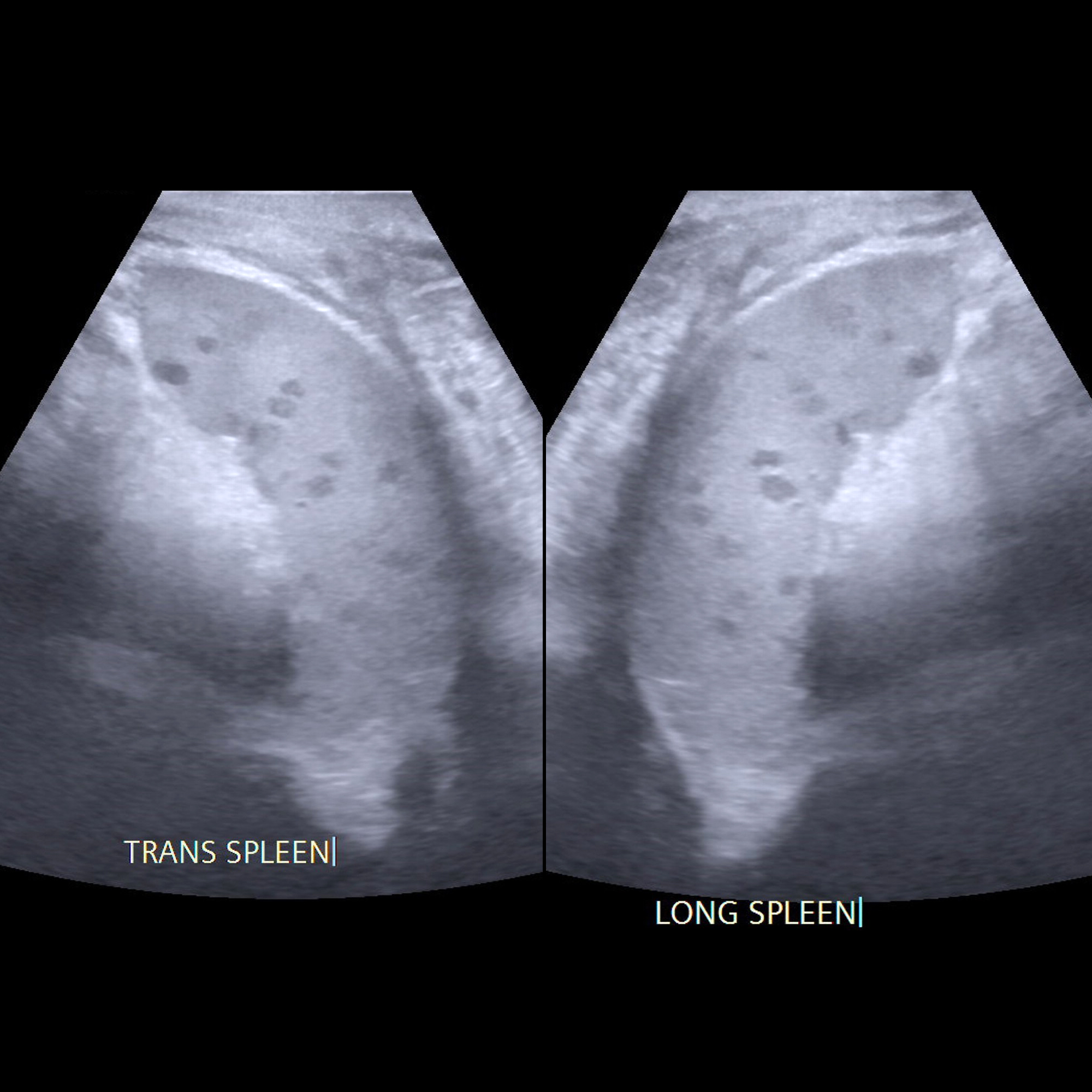
Ultrasound
Splenic abscesses are typically poorly-demarcated with a variable appearance, ranging from predominantly hypoechoic with some internal echoes to hyperechoic . They may contain septa of varying thickness. The presence of gas bubbles may also be seen with reverberation artefact, although the majority of splenic abscesses do not contain gas.
Ultrasound may also be used to guide abscess aspiration .
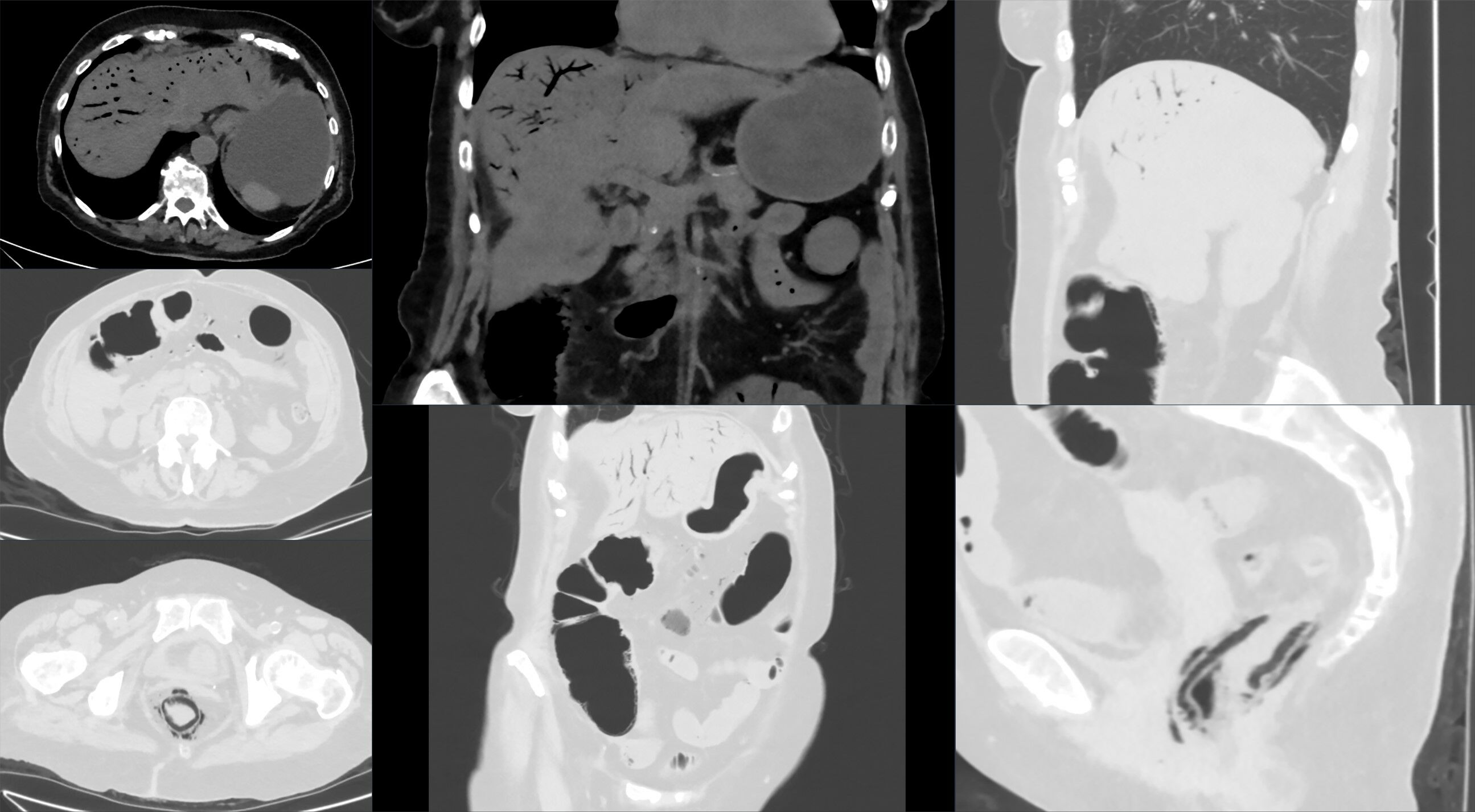
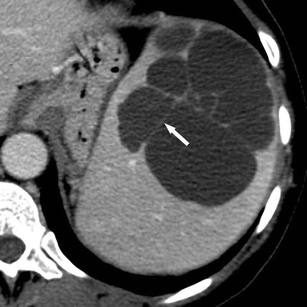
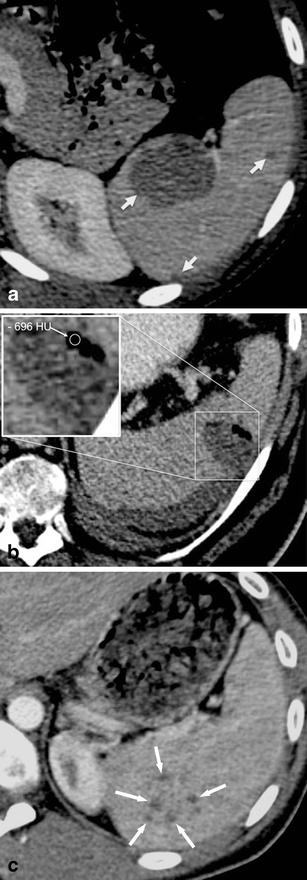
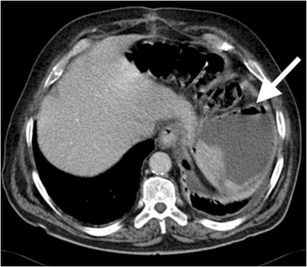
CT
Normally are centrally low-density lesions (20-40 HU ). Minimal peripheral contrast enhancement may be present once a capsule has developed. Ascites and adjacent pleural effusion can be seen.
MRI
May show solitary, multiple, or multilocular intrasplenic lesions. MR imaging characteristics can vary dependent on the size and infectious agent.
Usually, the abscesses are of fluid signal intensity :
- T1: low signal (T1 signal may increase if there is proteinaceous content)
- T2: high signal
- T1 C+ (Gd)
- there can be minimal peripheral enhancement once a capsule develops
- larger lesions can also show peripheral and perilesional enhancement
Nuclear medicine
The clinical context is vital in interpreting nuclear medicine images.
In some cases, 99mTc-HMPAO leukocyte scans or 99mTc-HIG (human polyclonal immunoglobulin) scans may show one or more intrasplenic defects .
111-In leukocyte scans and 67-Ga scans may also show a photophenic abscess cavity .
Treatment and prognosis
Traditional treatment for splenic abscess has been splenectomy and antibiotic therapy but image-guided percutaneous aspiration and drainage can also be considered. While many advocate image-guided drainage , several publications suggest that splenectomy has a better outcome than percutaneous drainage or intravenous antibiotics alone .
Differential diagnosis
As a broad differential for splenic abscesses, consider other splenic lesions.
Siehe auch:
- portalvenöses Gas
- zystische Läsionen der Milz
- septische Embolie Milz
- Infektionen der Milz
- Candidiasis der Leber und oder Milz
- fokale Milzläsionen und Anomalien
und weiter:
 Assoziationen und Differentialdiagnosen zu Milzabszess:
Assoziationen und Differentialdiagnosen zu Milzabszess: