bicuspid aortic valve


Bicuspid aortic valve (BAV) refers to a spectrum of deformed aortic valves with two functional leaflets or cusps which are often unequal in size.
They are most often congenital while an acquired bicuspid valve occurs when there is fibrous fusion between the right and left cusps of a pre-existing trileaflet aortic valve.
A congenitial biscuspid aortic valve is considered to be one of the most common causes of isolated aortic stenosis . It is considered a major cause of aortic valve disease in young adults.
Epidemiology
The estimated incidence of a congenital bicuspid valve in the general population is thought to be ~2%. They may be more common in males.
Pathology
BAV refers to a spectrum of deformed aortic valves with two functional leaflets or cusps which are often unequal in size. Only two cusps, commissures and sinuses are seen in the less common "pure" BAV subtype. The more common form of BAV occurs in a valve with three cusps with underdevelopment of a commissure and fusion of two adjacent cusps to form a raphe . Over time, the abnormal stress across the valve leads to calcification, usually in adulthood.
Types
Several classification have been proposed with one of the more common being
- type I
- type Ia: raphe between right coronary cusp and left coronary cusp
- type Ib: purely bicuspid with fusion between left and right coronary cusps
- type II
- type IIa: raphe between right coronary cusp (RCC) and non coronary cusp (NCC)
- type IIb: purely bicuspid with fusion between non coronary and right coronary cusps
- type III
- type IIIa: raphe between left coronary cusp (LCC) and non coronary cusp (NCC)
- type IIIb: purely bicuspid with fusion between non coronary and left coronary cusps
Associations
- dilatation of the proximal ascending aorta: most frequent association
- other congenital cardiac disease:
- atrial and ventricular septal defects
- patent ductus arteriosus
- hypoplastic left heart syndrome
- coarctation of the aorta: approximately 70% (range 50-85%) of coarctations are thought to associated with bicuspid aortic valves
- Turner syndrome: 10-12 % of women with Turner syndrome
- autosomal dominant polycystic kidney disease
- intracranial aneurysm
Radiographic features
Plain radiograph
The usefulness of plain chest radiographs in the detection of a bicuspid valve is considered to be rather poor. Occasionally the presence of a single calcified raphe at the expected site of the bicuspid valve, which is best seen on lateral view as aortic valve is superimposed on spine on frontal radiographs, as well as post stenotic dilatation of the ascending aorta may suggest a biscuspid valve .
Echocardiography
Transthoracic echocardiography is typically an adequate imaging modality for identifying the presence of a bicuspid aortic valve, with sensitivity and specificity approaching 92% and 96% respectively given the presence of adequate sonographic windows . It is also used to surveil the development of valvular dysfunction and the associated aortopathy.
The parasternal windows are best to evaluate the morphology of the valve, defining the number and location of the commissures, valve excursion and mobility, and the presence and location of a raphe. Evaluation of the aortic root diameter often requires additional views to be obtained in more cephalad intercostal spaces. Color flow Doppler interrogation may reveal flow turbulence and valvular regurgitation. Features which may suggest the presence of a bicuspid aortic valve include :
- systolic "doming" of the valve leaflets
- morphologically normal aortic valve leaflets assume a parallel orientation when maximally open in mid-systole
- the restricted excursion in bicuspid valves results in leaflets which assume a concave (in respect to the valvular orifice) midsystolic posture
- eccentric closure line (M-mode)
- as the valve cusps may be markedly asymmetric in size, valve closure may deviate from the midposition of the aortic lumen
- may also occur in normal, tricuspid aortic valves
- diastolic leaflet prolapse
- often associated with eccentric aortic regurgitation
- ellipsoid valvular orifice in systole
- short axis views of a tricuspid aortic valve should demonstrate a triangular orifice with straight leaflet margins
- cusp fusion with a raphe
- an echoic thickening at the free margin of the valve leaflets corresponding to the location of cusp fusion
- may give the false appearance (in diastole) of a tricuspid valve
- abnormal number and orientation of the valve commissures
- typically located at the 10, 2, and 6 o'clock positions
- the most common variant (fusion of the right and left coronary cusps) has two commissures which divide the valve horizontally, appearing approximately at the 4 and 10 o'clock positions
- this imparts an antero-posterior division to the valve
- fusion of the right and non-coronary cusps results in a more vertical division, a result of the commissure orientation at roughly 12 and 6 o'clock
The presence of associated cardiac malformations and complications should also be sought, using both standard and extended windows to evaluate for the presence and significance of:
- aortic stenosis
- most common manifestation of valvular dysfunction
- aortic regurgitation
- imaging from the suprasternal notch with spectral Doppler may assist in an assessment of severity
- infective endocarditis
- associated with severe hemodynamic compromise
- often requires surgical intervention
- bicuspid aortic valve aortopathy
- dilation of the ascending aorta distal to the sinotubular junction is characteristic, with relative sparing of the aortic root
- significantly increased risk of thoracic aortic dissection
- coarctation of the aorta
- patent ductus arteriosus
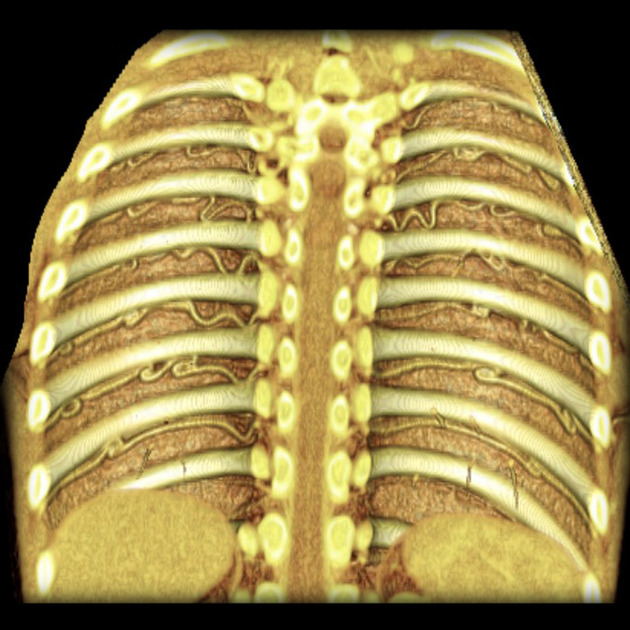
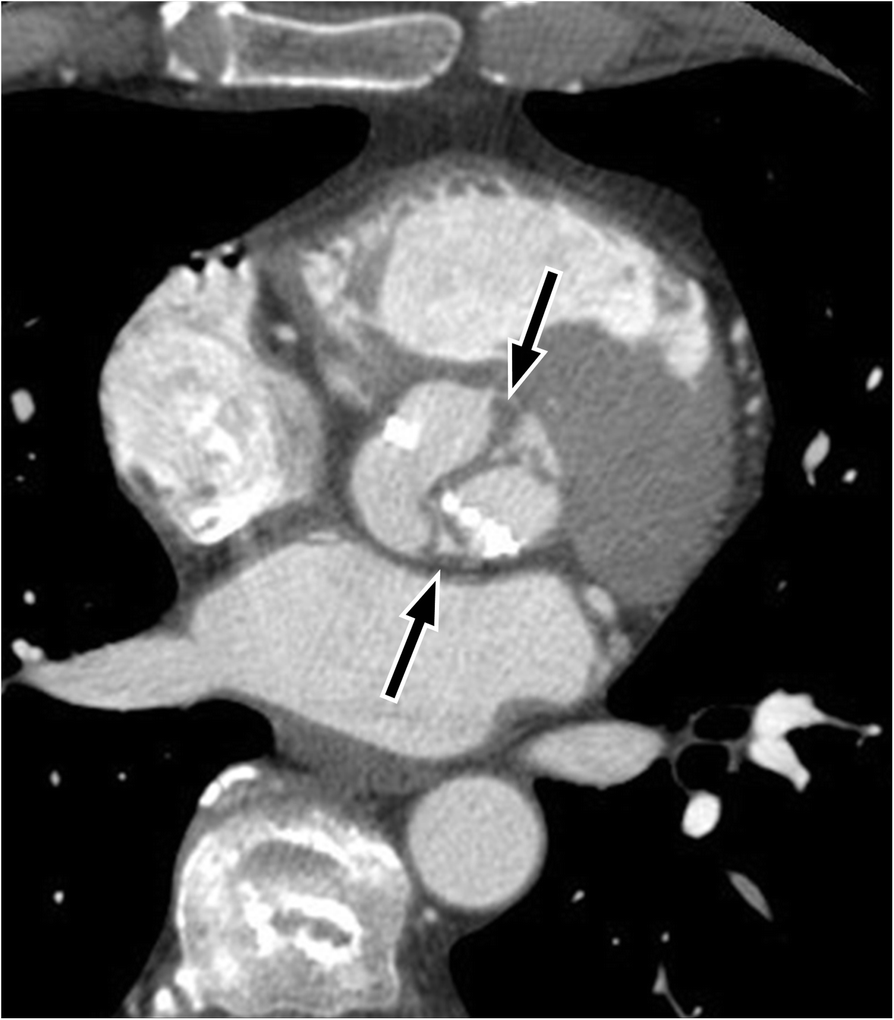
CT
At the time of writing, CT has a much higher reported detection rate for bicuspid valves and include :
- sensitivity: 94%
- specificity: 100%
- positive predictive value: 100%
- negative predictive value: 97%
Characteristic “fish-mouth” shape of the open valve in systole is noted on ECG-gated cardiac CT .
There is often earlier leaflet calcification.
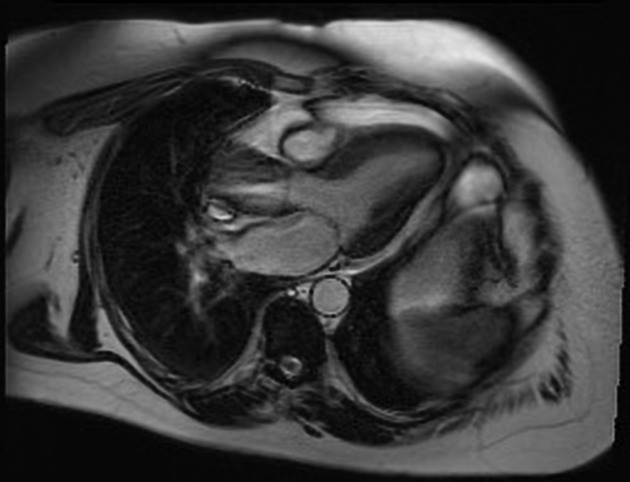
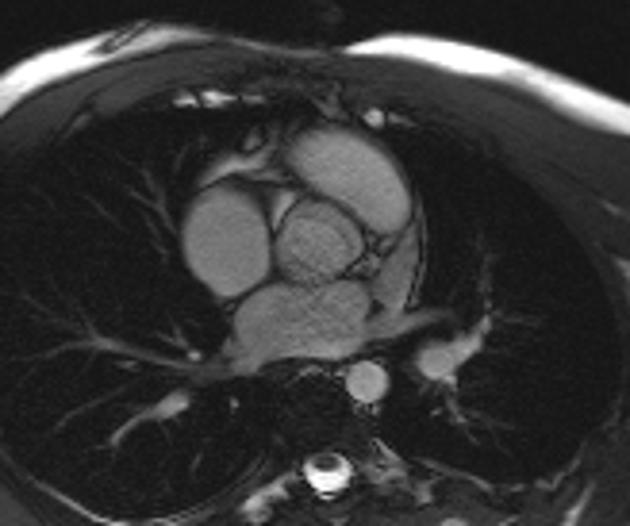
MRI
Cardiac MRI has the advantage of demonstrating the dynamic motion of the bicuspid valve when heavily calcified valves make echocardiography difficult to interpret. Furthermore, MRI can provide non-invasive assessment of the ascending aortic diameter and the presence of coarctation in a single study.
Experimental 4D MRI studies have suggested a "hurricane aorta" like flow pattern .
Treatment and prognosis
A minority of patients develop aortic regurgitation as a young adult but the majority have progressive valve stenosis, with only about 1% maintaining normal valve function over their lifetime .
High blood pressure should be controlled.
Symptomatic children have very little calcification and are treated by balloon valvuloplasty. Also, insertion of a valve in a child is not advisable, as the child will continue to grow.
In adults, aortic valve replacement is performed and occurs in a younger age group than in patients with tri-leaflet valve stenosis. Aortic root replacement is also required in 30% of patients undergoing valve replacement .
Complications
Recognized complications include:
- aortic stenosis
- this is secondary to leaflet calcification which occurs earlier (around age 40) than in patients with tri-leaflet aortic valves
- turbulent flow across the valve predisposes to leaflet calcification
- aortic insufficiency
- in children: incompetence develops secondary to redundant valve leaflets, endocarditis, or following balloon valvuloplasty
- in adults: dilatation of the ascending aorta can lead to regurgitation
- ascending aortic aneurysm
- an aortopathy is present irrespective of the valve function; aortic dilatation (and dissection) is due to abnormal media; as such, BAV can be considered a disease of both the valve and ascending aorta, and this should be a consideration in surgical decision making
- aortic dissection: secondary to aortopathy and abnormal media
- infective endocarditis: due to turbulent flow
Siehe auch:
- Aortenisthmusstenose
- autosomal-dominante polyzystische Nierenerkrankung
- Aortenstenose
- unikuspidale Aortenklappe
- Bikuspidalität
und weiter:

 Assoziationen und Differentialdiagnosen zu Bikuspidalität der Aortenklappe:
Assoziationen und Differentialdiagnosen zu Bikuspidalität der Aortenklappe: