Cardiac CT
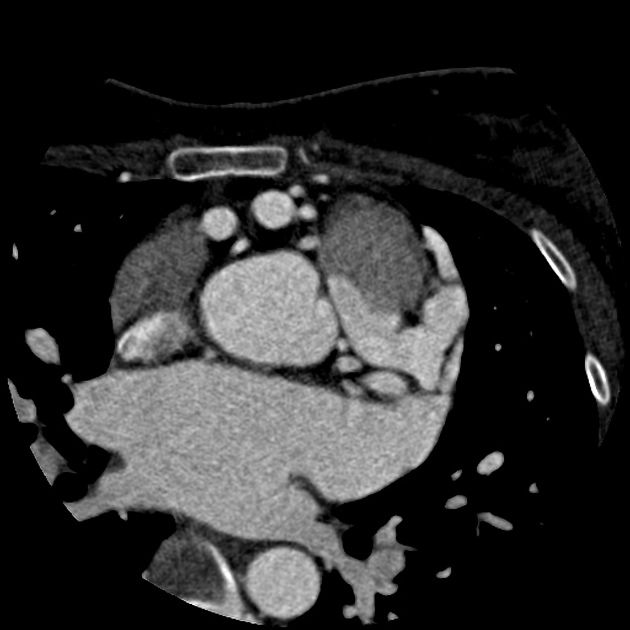


Computed tomography of the heart or cardiac CT is routinely performed to gain knowledge about cardiac or coronary anatomy, to detect or diagnose coronary artery disease (CAD), to evaluate patency of coronary artery bypass grafts or implanted coronary stents or to evaluate volumetry and cardiac function (including ejection fraction).
Technique
Usually, coronary CT angiography (cCTA) is performed as it contains data about coronary and cardiac anatomy. Due to recent innovations during the last two decades, new cCTA protocols allow for significant dose reductions with reported mean sub-milliSievert doses. However, each examination must be tailored to each patient depending on patient characteristics and clinical indication.
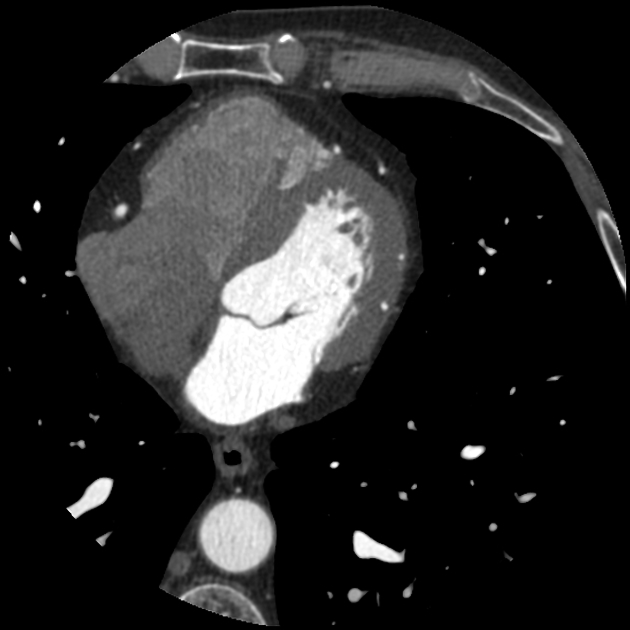
Calcium scoring
When evaluating the heart for potential CAD, usually a nonenhanced calcium scoring sequence is first performed to assess for coronary artery calcification. This low-dose technique allows for a detection of calcifications of the coronary arteries. Although this technique does not give any information about potential hemodynamically relevant stenoses, an Agatston score can be calculated based on that data. The calculated Agatston score allows for an early risk stratification of patients with a high Agatston score (>160) have an increased risk for a major adverse cardiac event (MACE) .
Coronary CT angiography
In contrast to other CT angiography examinations, cCTA usually requires a rather high flow rate for the contrast media injection, usually between 4-5 mL/sec through an antecubital vein. Beta blockers and sublingual nitrates are usually administered before the examination to lower the heart rate, avoid arrhythmia and dilate the coronary arteries.
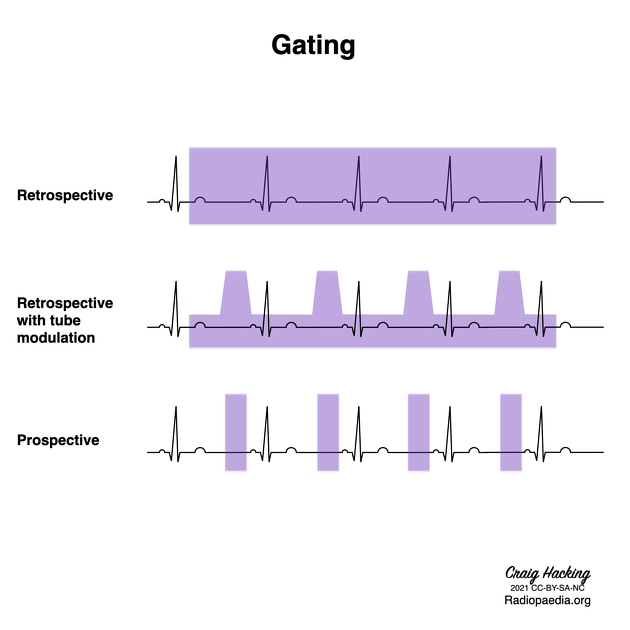
To allow for an improved image quality and dose reduction, cCTA is usually ECG-triggered to adapt the scan sequence to the patient's heartbeat.
Retrospectively ECG-gated cCTA protocols
This is an established and robust technique which works as a standard spiral CT acquisition. After detection of the heart rhythm, the scan covers the whole heart during multiple cardiac cycles. Therefore, information from different phases of the cardiac cycle is gained and can be used. This is especially useful for cine-sequences which show the heart motion throughout the cardiac cycle. Currently, such cine sequences can only be generated from retrospectively ECG-gated cCTA data.
Although several dose-saving techniques for retrospectively ECG-gated cCTA exist (e.g. tube modulation), these protocols still result in a higher radiation dose than newly introduced prospectively ECG-gated protocols. They do however retain their clinical relevance in patients with arrhythmia and for volumetry and functional analysis.
Prospectively ECG-gated cCTA protocols
Since cardiac CT is mostly performed to evaluate coronary artery anatomy and not functional anatomy, several innovations have been introduced during the last two decades to significantly reduce radiation dose from cardiac CT.
Sequential acquisition
This technique (also called step-and-shoot mode) is based on the principle that several images acquired at different heart phases and anatomic regions of the heart can be combined for reconstruction of the whole heart.
High-pitch spiral acquisition
Dual-source CT scanners allow for a gapless acquisition with a pitch of up to 3.4 which cannot be achieved with conventional single-source CT scanners. A high-pitch spiral acquisition can be performed in less than one second and thus information from a single heartbeat can be generated. In combination with iterative reconstruction techniques, high-pitch spiral acquisition allows for cardiac CT with sub-milliSievert doses.
Limitations of prospectively ECG-gated protocols
It should be noted that all prospectively ECG-gated protocols are more susceptible to deterioration of image quality due to motion artifacts. Therefore, when choosing such a protocol, the patient's heart rate should ideally be below 65 beats per minute (bpm). In high-pitch spiral acquisition, the heart rate should even be below 60 bpm. Therefore, the cost of significant dose reduction is the limited patient population that such protocols can be applied to.
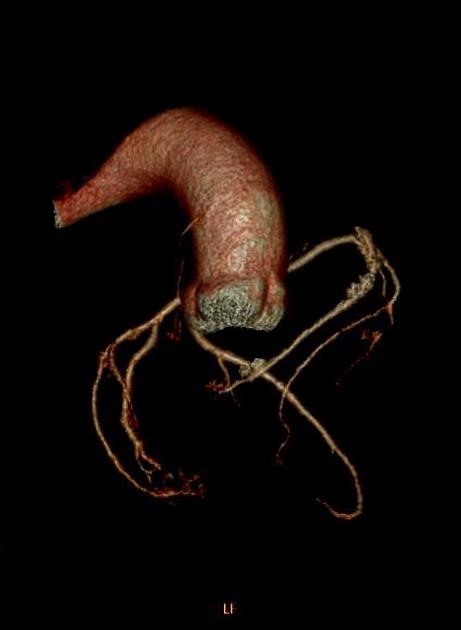
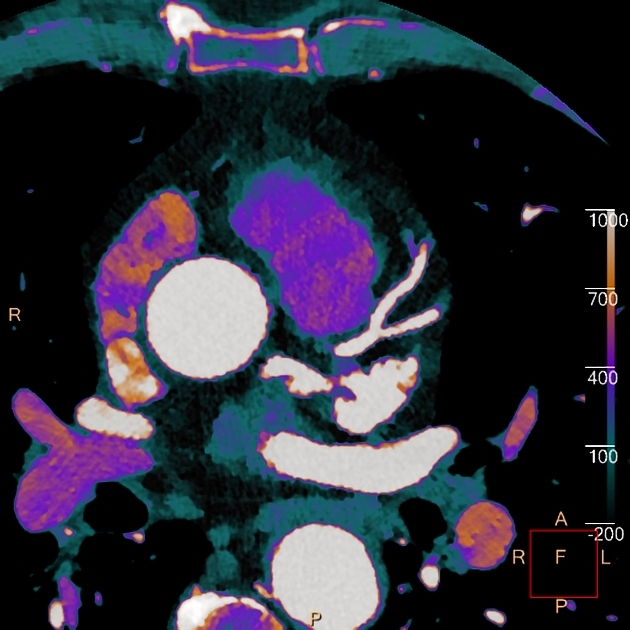
Post-processing
Due to the usually tortuous anatomy of the coronary arteries, curved multiplanar reconstructions (MPR) or maximum intensity projections (MIP) are usually generated to allow for assessment of coronary lumina on a dedicated workstation. In these images, coronary stenoses can be evaluated and lumen reduction can be measured.
Increasingly, sophisticated algorithms and machine learning techniques enable the estimation of fractional flow reserve .
Indications
- noninvasive evaluation of coronary artery anomalies and other thoracic vessels
- symptomatic patients with low/moderate probability of coronary artery disease (CAD)
- normal or uninterpretable/non-diagnostic ECG
- normal or equivocal cardiac biomarkers
- moderate risk non-acute symptomatic patients without known heart disease (may be able to exercise)
- low risk non-acute symptomatic patients without known heart disease (if the patient cannot exercise or undergo stress test)
- evaluating the patency of a coronary artery bypass graft (CABG)
- new onset heart failure
- no prior history of CAD, low/intermediate probability
- decreased ejection fraction
- preoperative assessment of the coronary arteries before noncoronary cardiac surgery if intermediate risk of CAD
- discordant ECG and imaging results after stress imaging
- new or worsening symptoms with past normal stress imaging study
- preoperative assessment for transcatheter aortic valve implantation (TAVI/TAVR)
Its utility is uncertain in some situations:
- high probability coronary artery disease
- including non-acute symptomatic patients without known heart disease
- acute chest pain of uncertain cause
- evaluation of coronary artery stents >3 mm
Contraindications
It is not indicated in some situations:
- if the patient is having an acute myocardial infarction (heart attack)
- screening of asymptomatic patients with low-to-intermediate risk of CAD
- evaluation of coronary artery stents <3 mm
- evaluation of asymptomatic patients post CABG (<5 years old) and post stent (<2 years old)
See also
Siehe auch:

