Choledochuszyste










Choledochal cysts represent congenital cystic dilatations of the biliary tree. Diagnosis relies on the exclusion of other conditions (e.g. tumor, gallstone, inflammation) as a cause of biliary duct dilatation.
Epidemiology
Choledochal cysts are rare, with an incidence of 1:100,000-150,000. Although they may be discovered at any age, 60% are diagnosed before the age of 10 years . There is a strong female predilection with M:F ratio of 1:4. There is a greater prevalence in East Asia.
Clinical presentation
Classical presentation includes the triad of :
- abdominal pain
- jaundice
- abdominal mass
This triad is however only present in ~40% (range 19-60%) of cases, with palpable mass being the least common manifestation.
Pathology
Their etiology is uncertain, but a close association with the anomalous formation of the pancreaticobiliary ductal junction is reported in some subtypes . Due to this anomaly, there is a large common channel draining pancreatic and bile duct. Thus the pancreatic juices cause cholangitis and bile duct wall destruction, which together with distal stenosis due to scarring result in the formation of a choledochal cyst.
Associations
A number of associations are recognized, including :
- biliary atresia
- hepatic fibrosis
- associated with type V (Caroli disease)
Classification
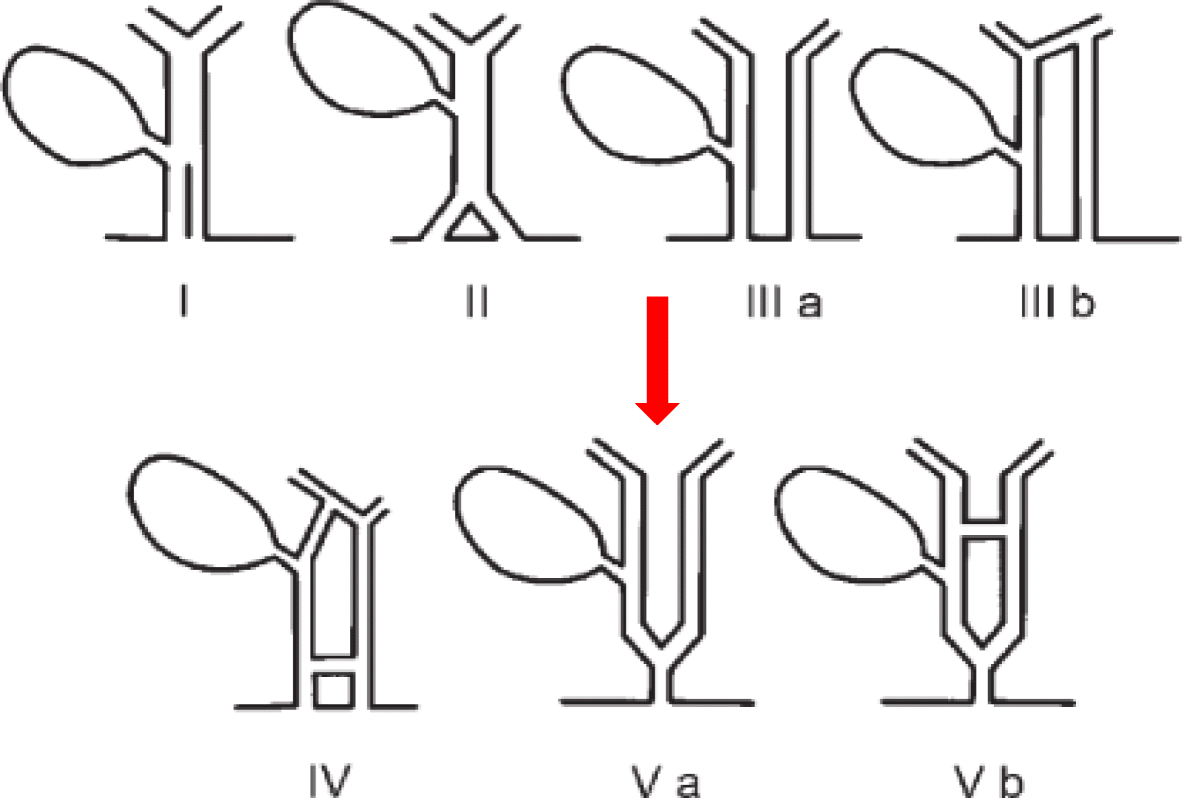
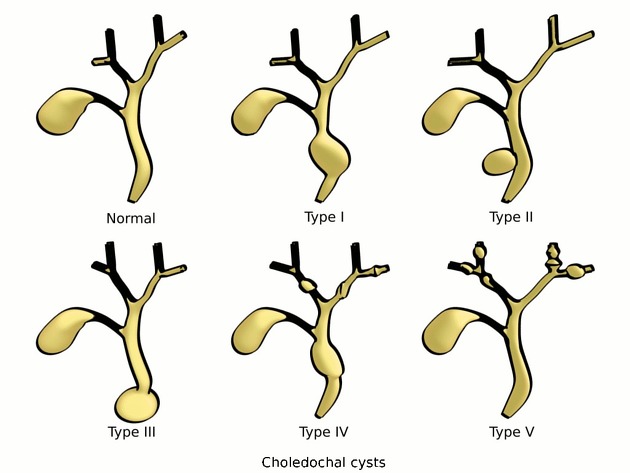
Commonly accepted classification currently is one devised by Todani et al. There are five main types, with several subtypes some of which can be pathologically unrelated:
- type I: most common, accounting for 80-90% (this type can present in utero)
- Ia: dilatation of extrahepatic bile duct (entire)
- Ib: dilatation of extrahepatic bile duct (focal segment)
- Ic: dilatation of the common bile duct portion of extrahepatic bile duct
- type II: true diverticulum from extrahepatic bile duct
- type III: dilatation of extrahepatic bile duct within the duodenal wall (choledochocoele)
- type IV: next most common
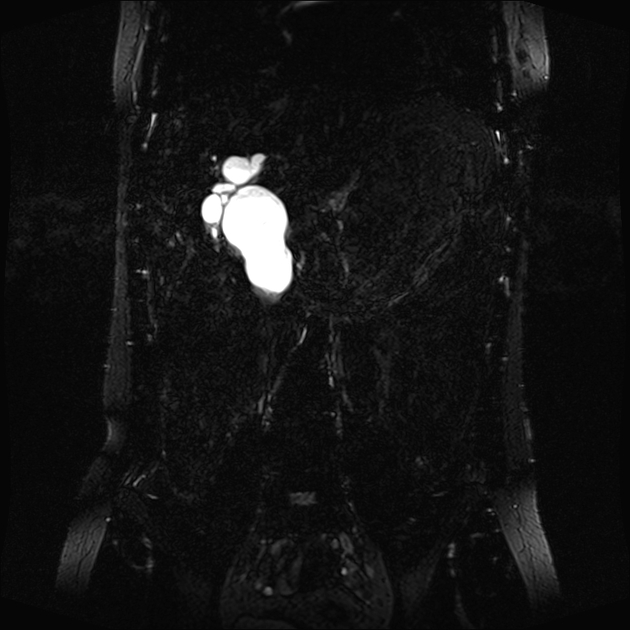
- IVa: cysts involving both intra and extrahepatic ducts
- IVb: multiple dilatations/cysts of extrahepatic ducts only
- type V: multiple dilatations/cysts of intrahepatic ducts only (Caroli disease)
The Todani classification scheme has been called into question in surgical literature, with claims that it may unfairly link multiple distinct processes into a spuriously coherent grading scheme .
The Komi classification classifies choledochal cyst into 3 types based on the anomalous union of the pancreatic-bile duct (AUPBD) .
Radiographic features
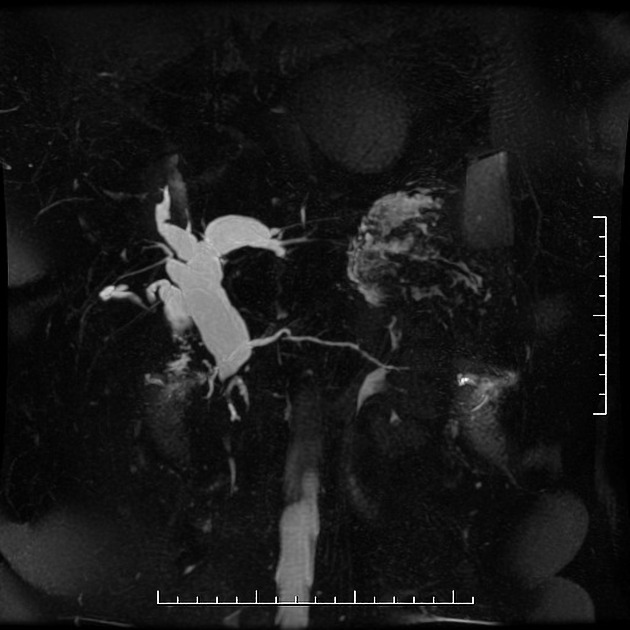
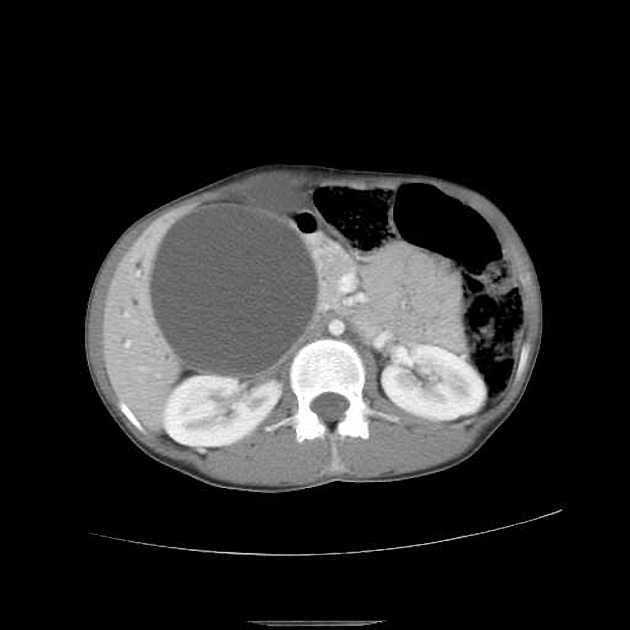
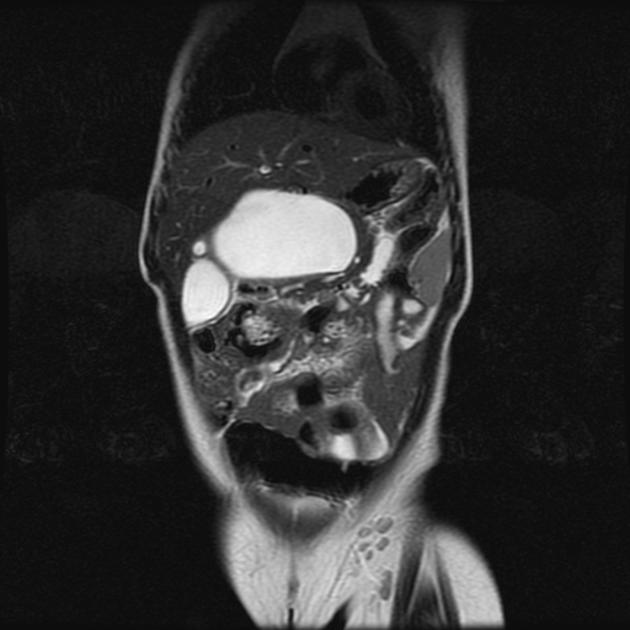
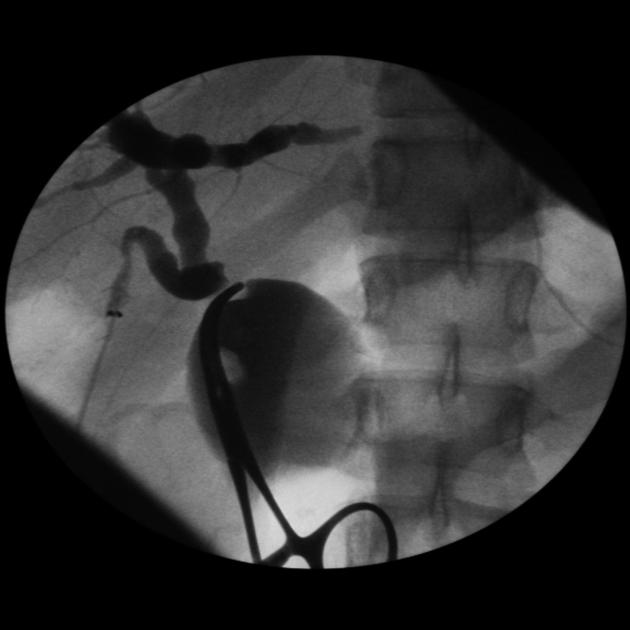
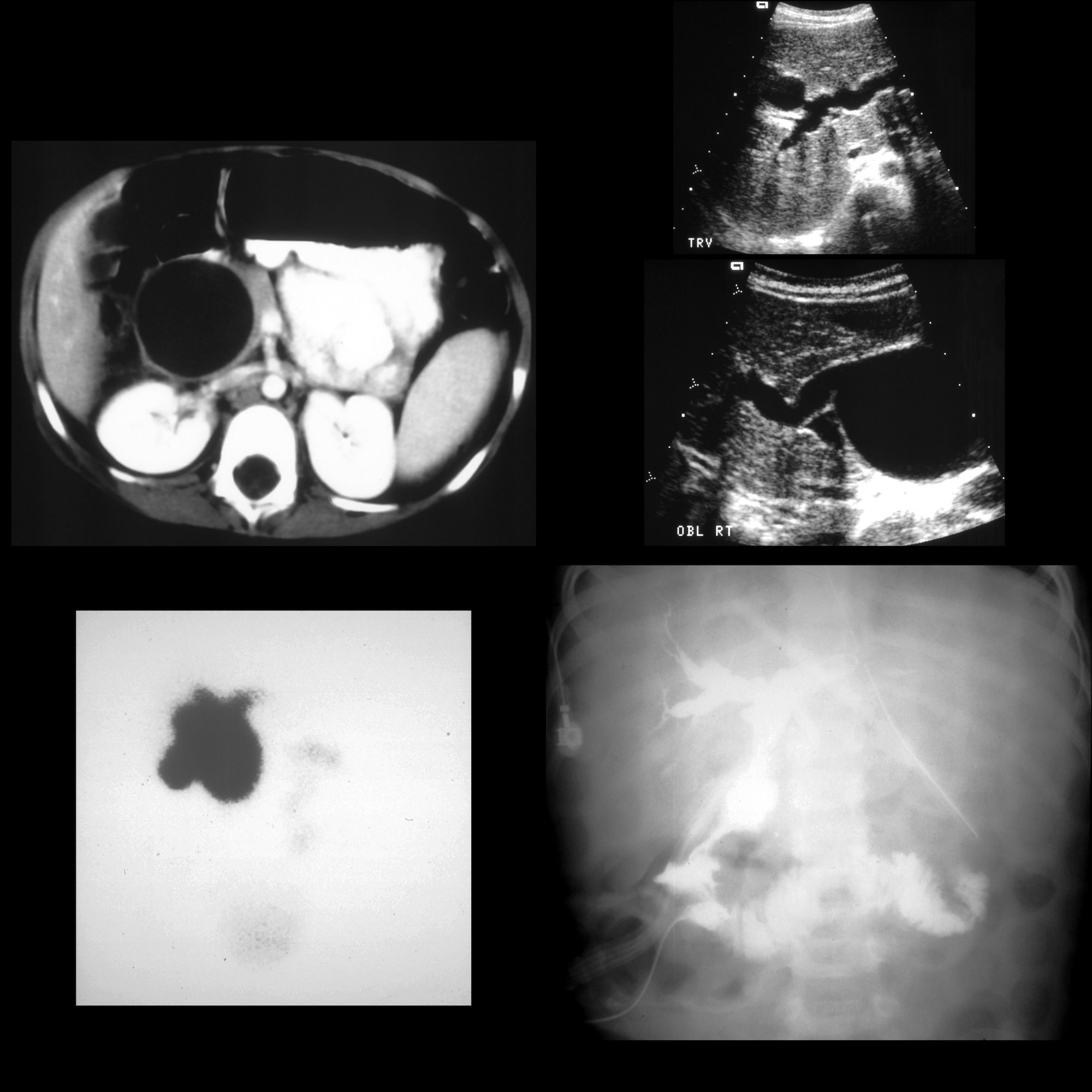
Imaging of the biliary tree can be achieved with ultrasound, CT, direct contrast studies (ERCP, PTC) or MRI.
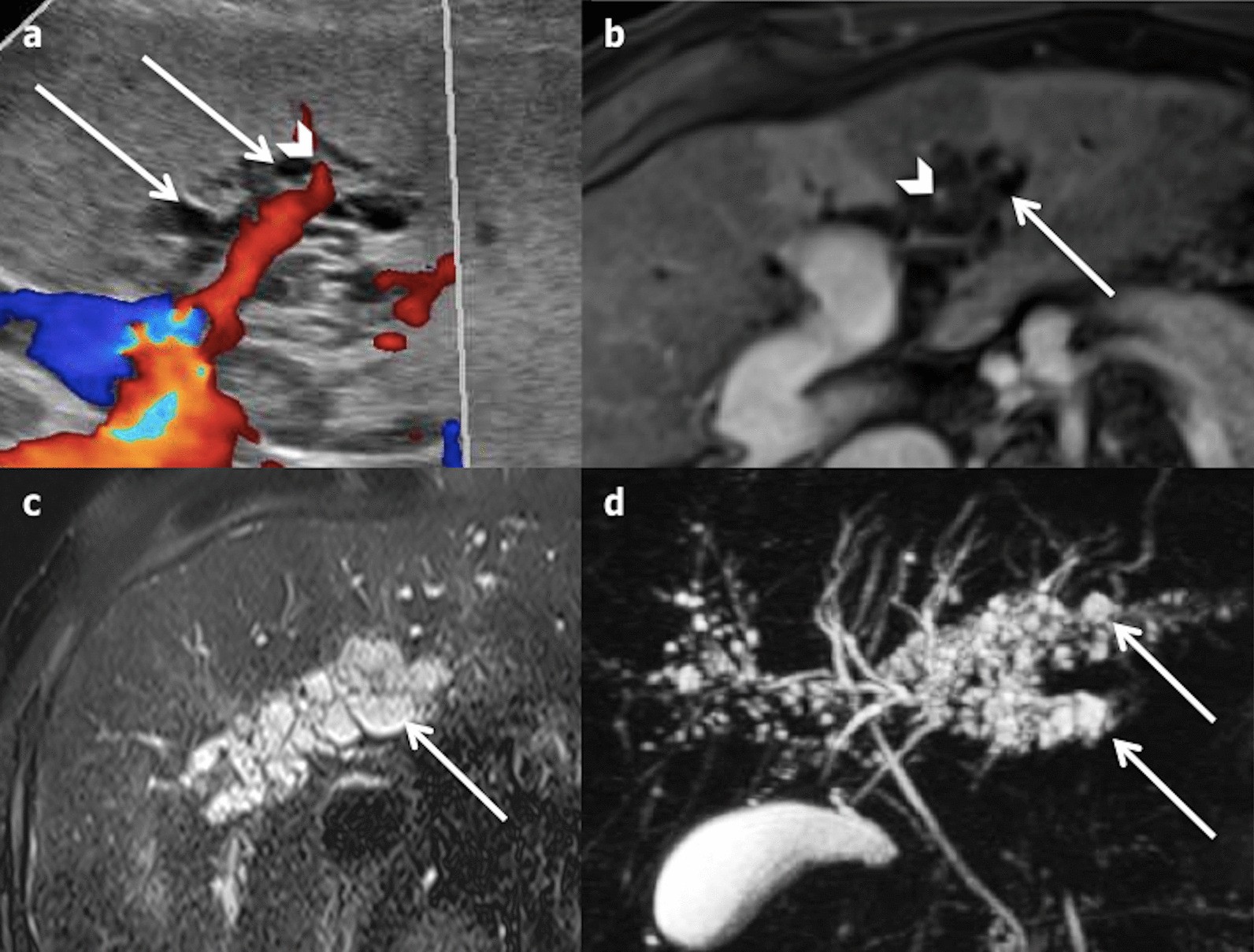
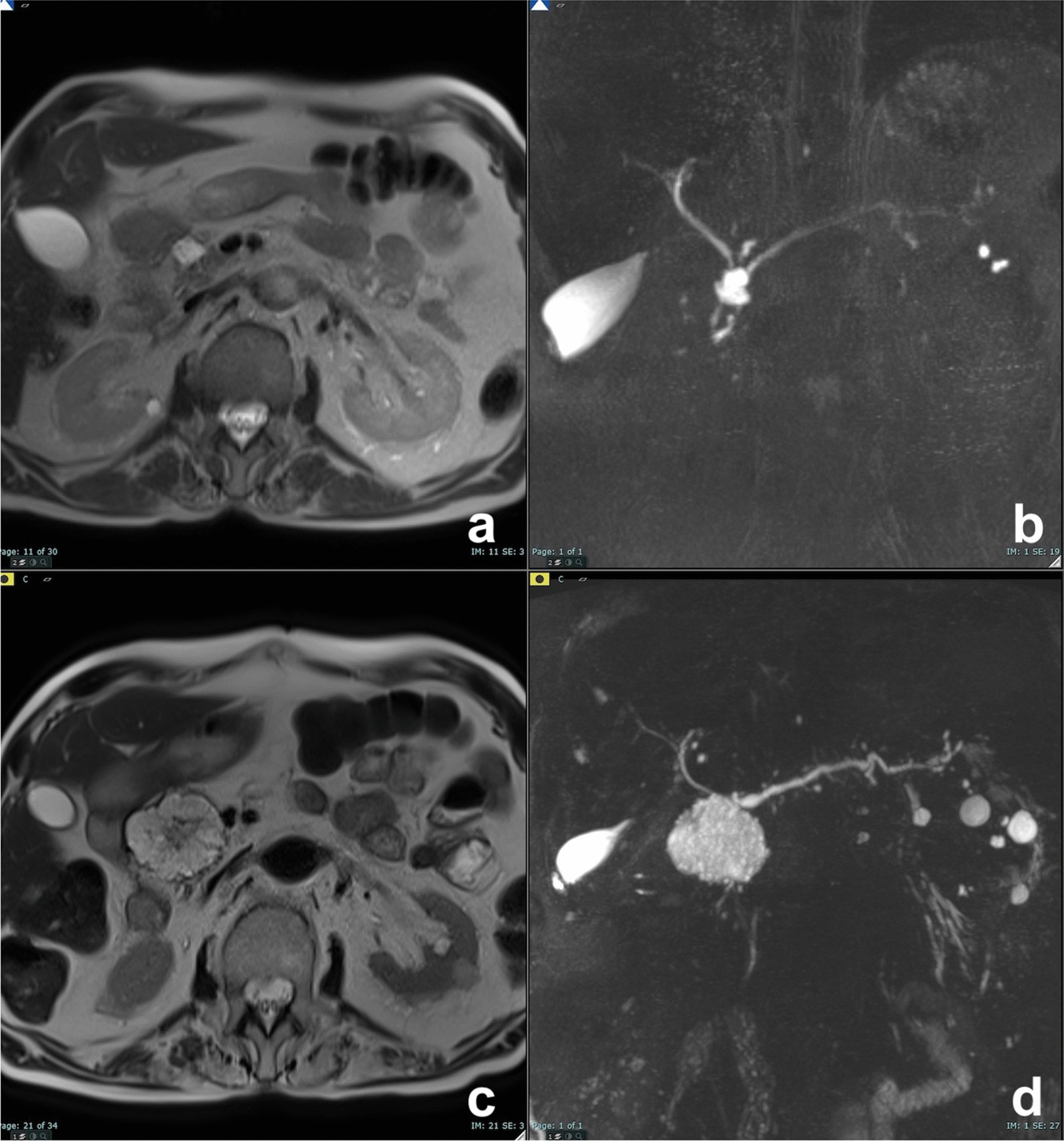
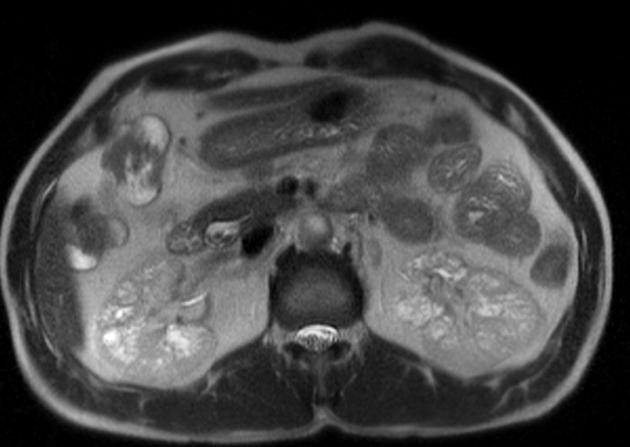
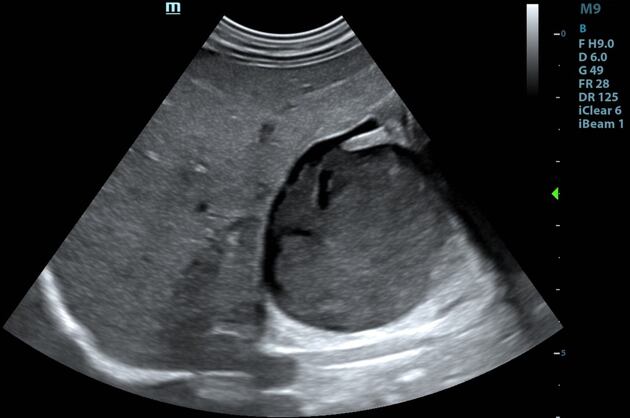
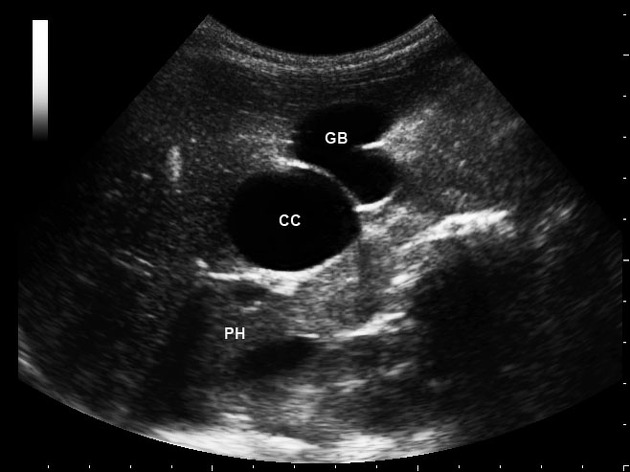
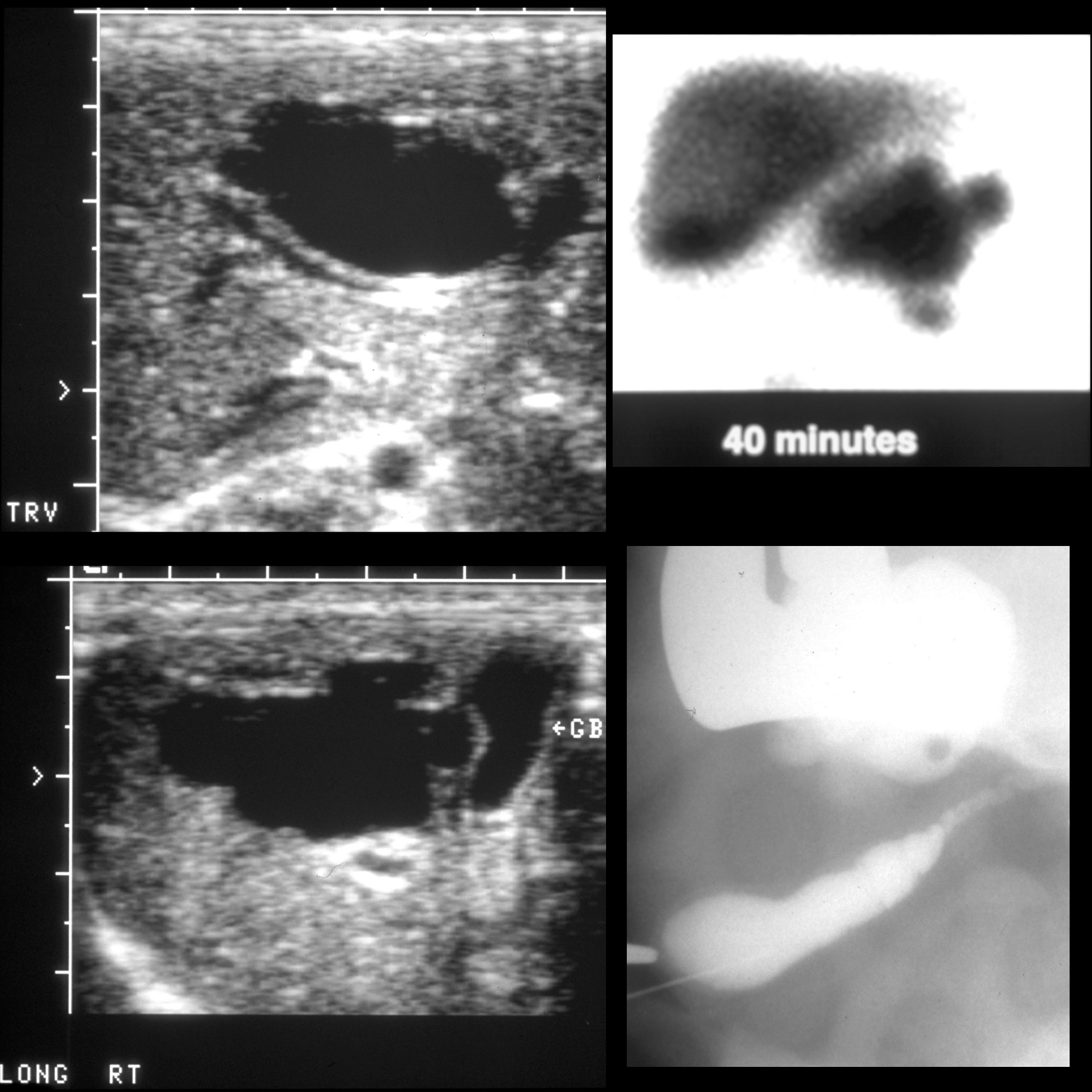
Ultrasound
The key to the diagnosis is a dilated cystic lesion which communicates with the bile duct and is separate from the gallbladder. A careful search for other causes needs to also be undertaken (see differential below), remaining cognizant that both stone formation and malignancy are associated with choledochal cysts.
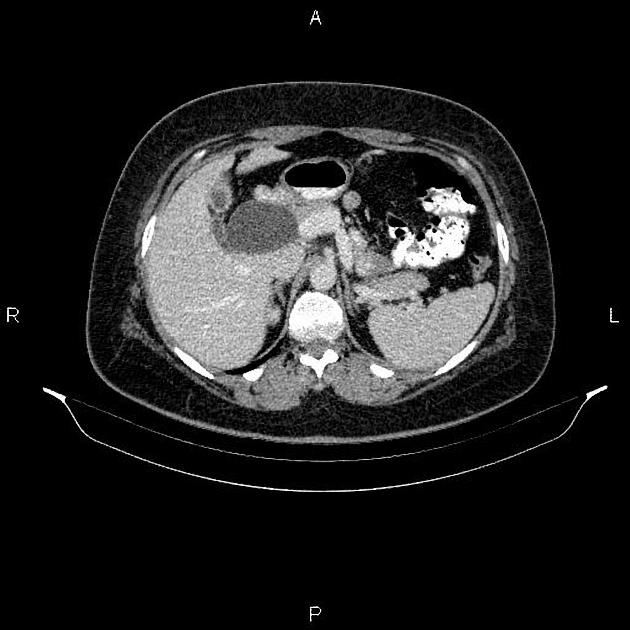
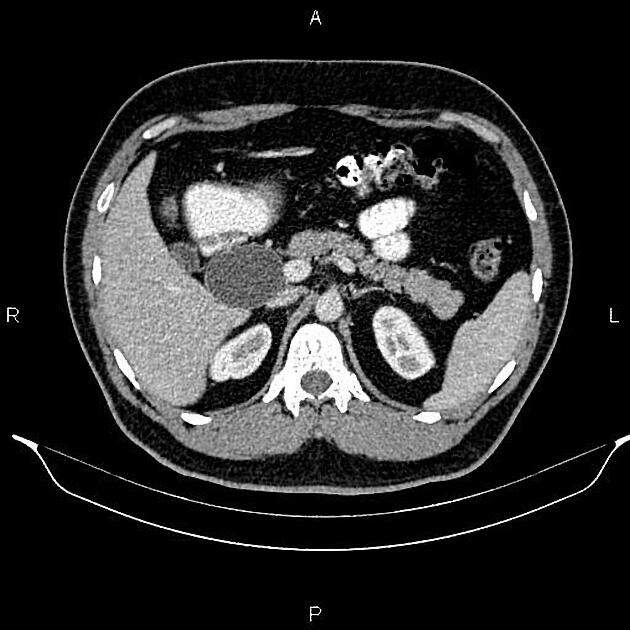
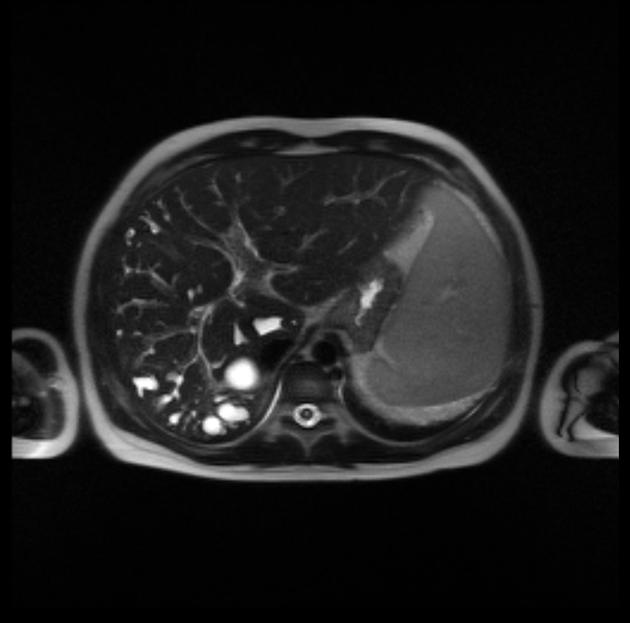
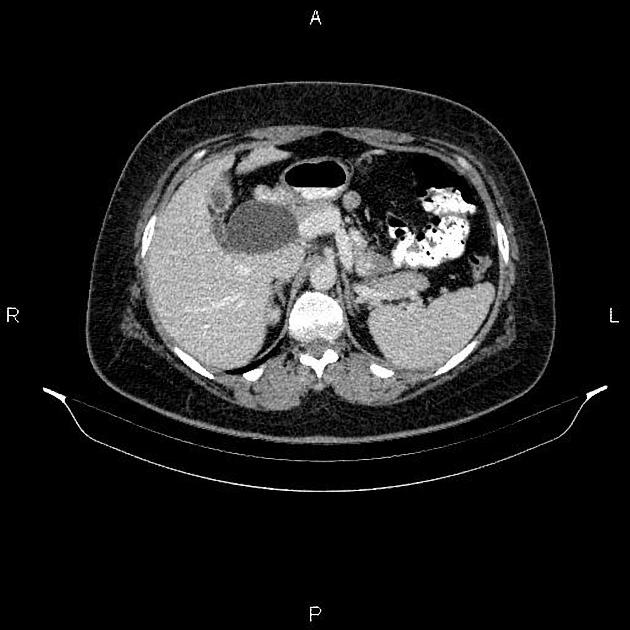
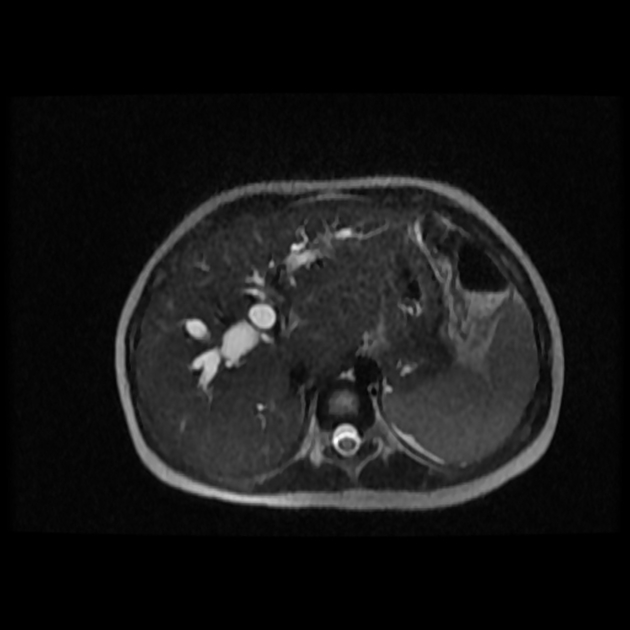
CT / MRI
Findings are similar to ultrasound, with a greater ability to demonstrate intrahepatic disease and complications.
Treatment and prognosis
Patients with type I, II, or IV cysts usually undergo surgical resection of the cyst due to the risk of malignancy. A number of possible approaches exist, depending on cyst location and other factors. Typically a Roux-en-Y hepaticojejunostomy is performed .
Complications
The two most frequent complications of choledochal cysts are stone formation and malignancy. Complications include:
- stone formation: most common
- malignancy
- cholangiocarcinoma
- lifetime incidence 10-15%
- the cyst may rupture leading to bile peritonitis
- most frequently seen in neonates
- pancreatitis
Differential diagnosis
General imaging differential considerations include:
- duodenal diverticulum
- pancreatic cystic lesions
- pseudocyst(s)
- cystic tumors
- other causes of biliary tree dilatation
- impacted gallstone
- cholangiocarcinoma
- biliary stricture
See also
Siehe auch:
- Duodenaldivertikel
- cholangiozelluläres Karzinom
- pseudocyst
- zystische Pankreasläsionen
- peribiliäre Zysten
- Normvarianten des Gallenwegssystems
und weiter:
- Ductus choledochus
- Todani-Klassifikation der Gallengangszysten
- Pankreaspseudozyste
- Caroli-Syndrom
- coarsened hepatic echotexture
- Double-Bubble-Zeichen
- Choledochozele
- anomalous pancreaticobiliary junction
- focal hypodense hepatic lesions on non-enhanced CT
- Dünndarmvolvulus
- biliäres Zystadenom
- simple Leberzyste
- Gallenblasenduplikatur
- Differenzialdiagnosen zystischer Leberläsionen
- bulleted and numbered lists
- numbered lists
- Tripelgallenblase
- choledochal cyst, type 1
- Todani Typ 2 Choledochuszyste
- Gallengangstumoren
- Komi Klassifikation Choledochuszyste
 Assoziationen und Differentialdiagnosen zu Choledochuszyste:
Assoziationen und Differentialdiagnosen zu Choledochuszyste: