diastematomyelia












Diastematomyelia, also known as a split cord malformation, refers to a type of spinal dysraphism (spina bifida occulta) when there is a longitudinal split in the spinal cord.
Terminology
Although traditionally it has been distinguished from diplomyelia (in which the cord is duplicated rather than split) the term split cord malformation is advocated to encompass both conditions . For the purposes of this article, the terms diastematomyelia and split cord malformation are used interchangeably.
Epidemiology
Split cord malformations are a congenital abnormality and account for ~5% of all congenital spinal defects .
Clinical presentation
The majority of patients with diastematomyelia are symptomatic, presenting with signs and symptoms of tethered cord, although patients with mild type II (see below) may be minimally affected or entirely asymptomatic . Presenting symptoms include:
- leg weakness
- low back pain
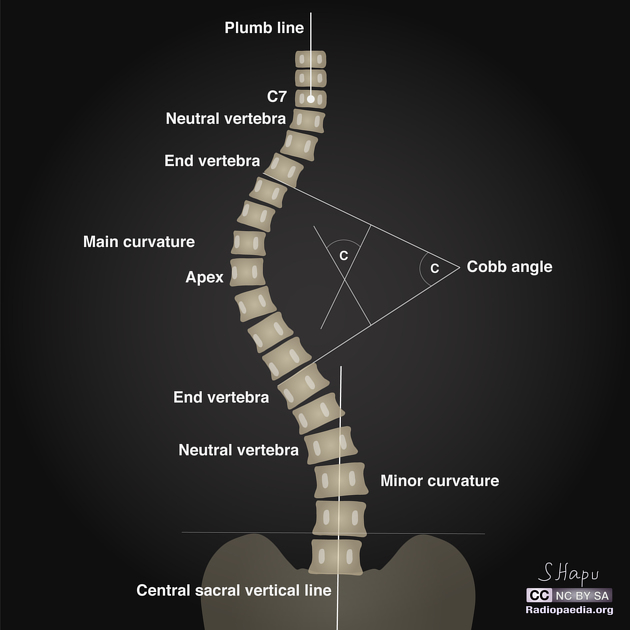
- scoliosis
- incontinence
Patients with diastematomyelia also frequently have other associated anomalies including:
- meningocele
- neurenteric cyst
- dermoid cyst
- clubfoot
- spinal cord lipoma
- hemangioma overlying spine
Pathology
Classification
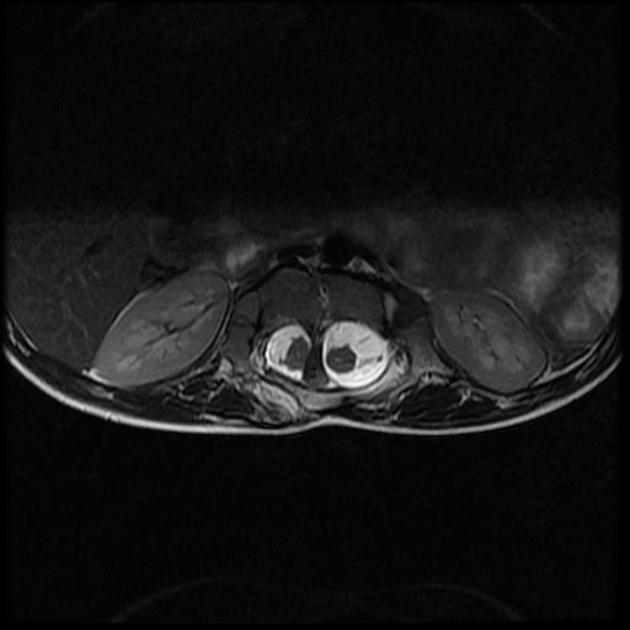
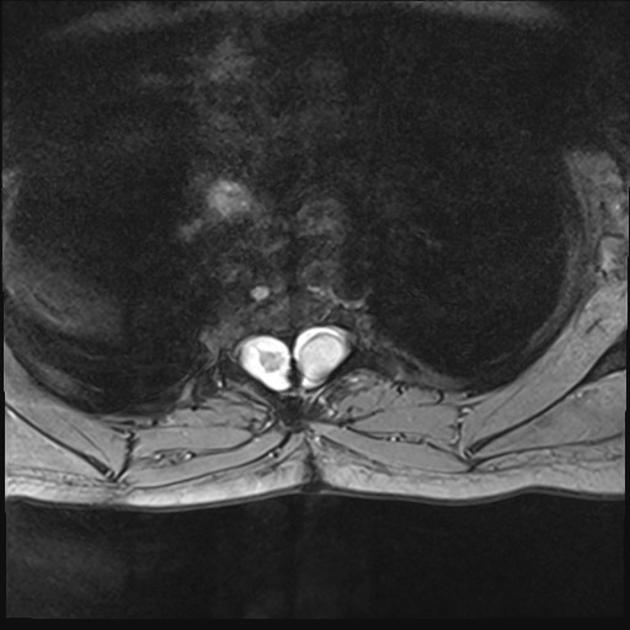
Split cord malformations are divided into two types according to the presence of a dividing septum and single vs dual dural sac:
- type I: duplicated dural sac, with common midline spur (osseous or fibrous) and usually symptomatic
- type II: single dural sac containing both hemicords; impairment less marked
Type I
Type I is the classic diastematomyelia, characterized by :
- duplicated dural sac
- hydromyelia common
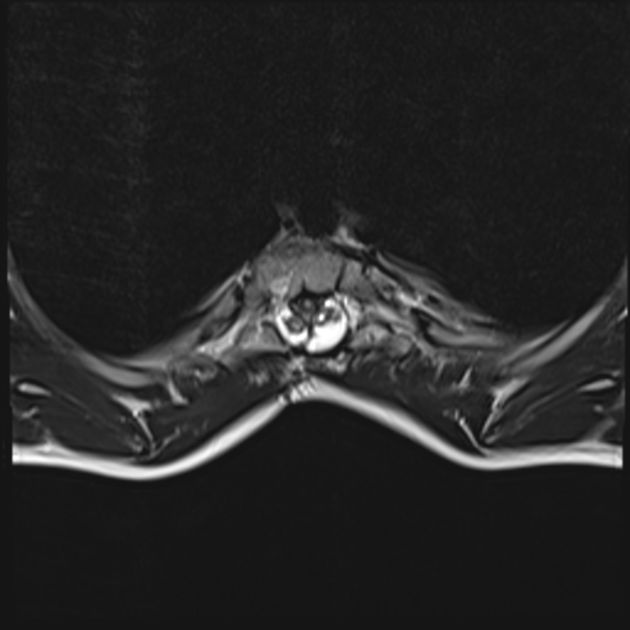
- midline spur often present (osseous or osteocartilaginous)
- vertebral abnormalities: hemivertebrae, butterfly vertebrae, spina bifida, fusion of laminae of adjacent levels
- skin pigmentation, hemangioma and hypertrichosis (hair patch) are common
- patients are usually symptomatic presenting with scoliosis and tethered cord syndrome
Type II
Type II is milder than type I, and lack many of the features of latter:
- single dural sac and no spur/septum
- cord divided, sometimes incompletely so
- hydromyelia may be present
- spina bifida may be present, but other vertebral anomalies are far less common
- patients a less symptomatic or may even be asymptomatic
Radiographic features
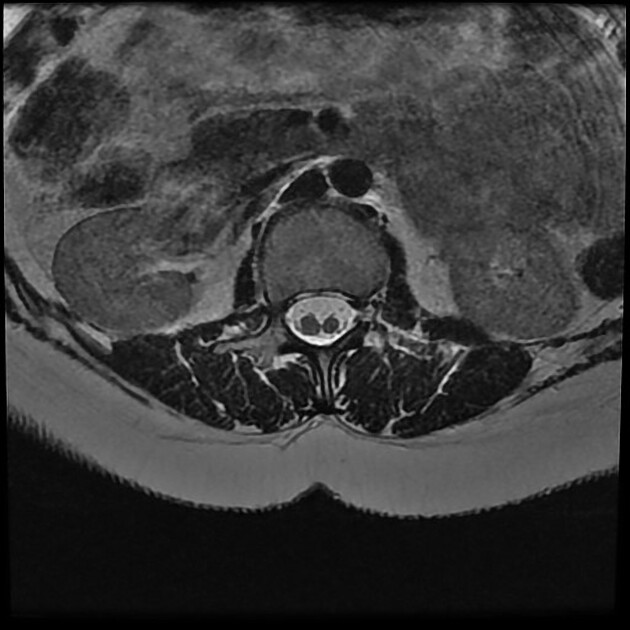
Split cord malformations are more common in the lower cord but can sometimes occur at multiple levels.
- 50% occur between L1 and L3
- 25% occur between T7 and T12
An associated bony, cartilaginous or fibrous spur projecting through the dura mater forwards from the neural arch is visible in 33% of cases .
Vertebral anomalies (spina bifida, butterfly or hemivertebrae) are common. Laminar fusion associated with a neural arch defect is a good predictor of diastematomyelia and occurs the level of the defect, or at an adjacent level.
Antenatal ultrasound
The presence of an extra echogenic focus in the midline between the fetal spinal posterior elements has been described as a reliable sign .
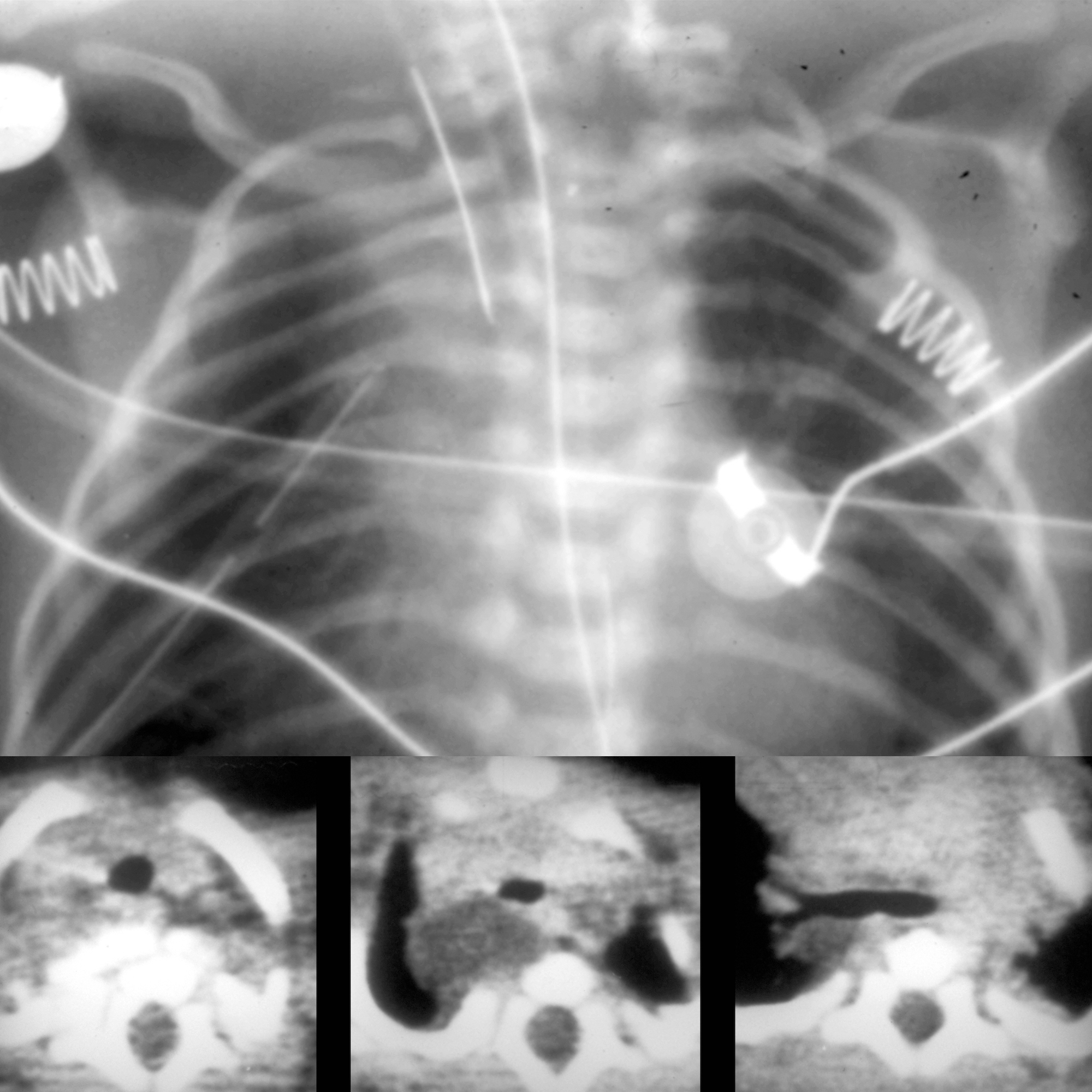
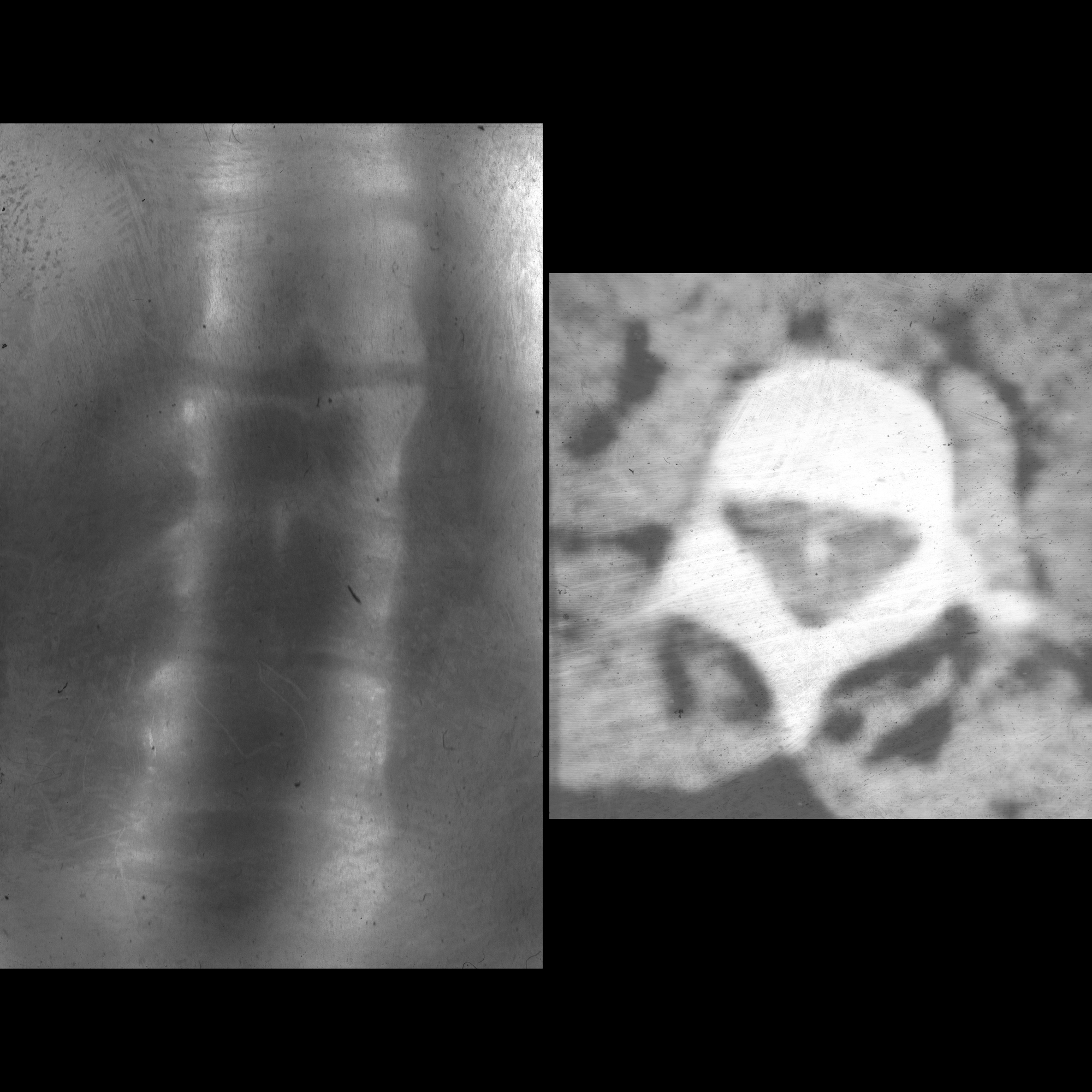
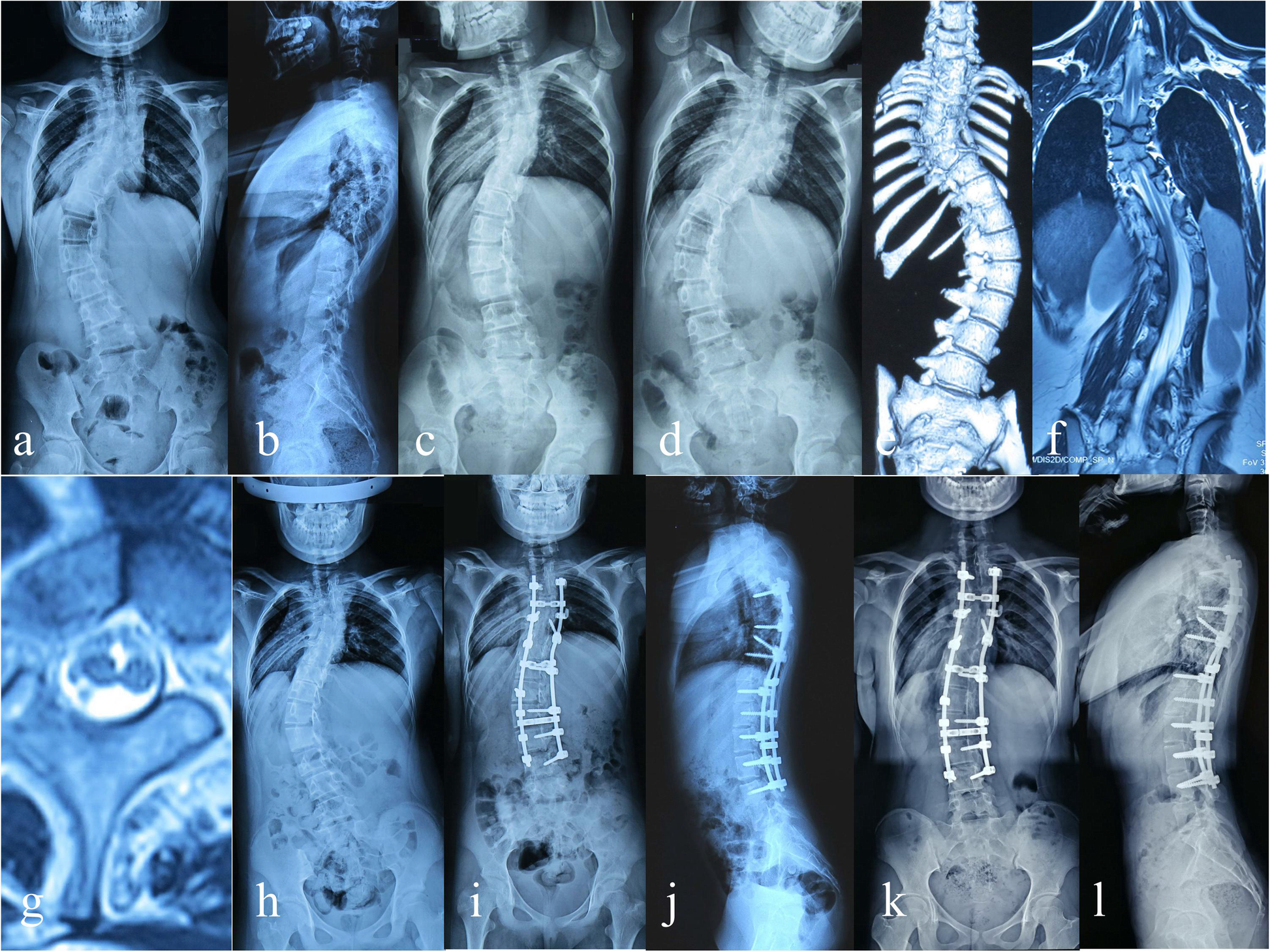
Plain radiograph
- multilevel spina bifida
- widening of interpedicular distance: but this may be remote from the site of the spur
- associated scoliosis
- anteroposterior vertebral body narrowing
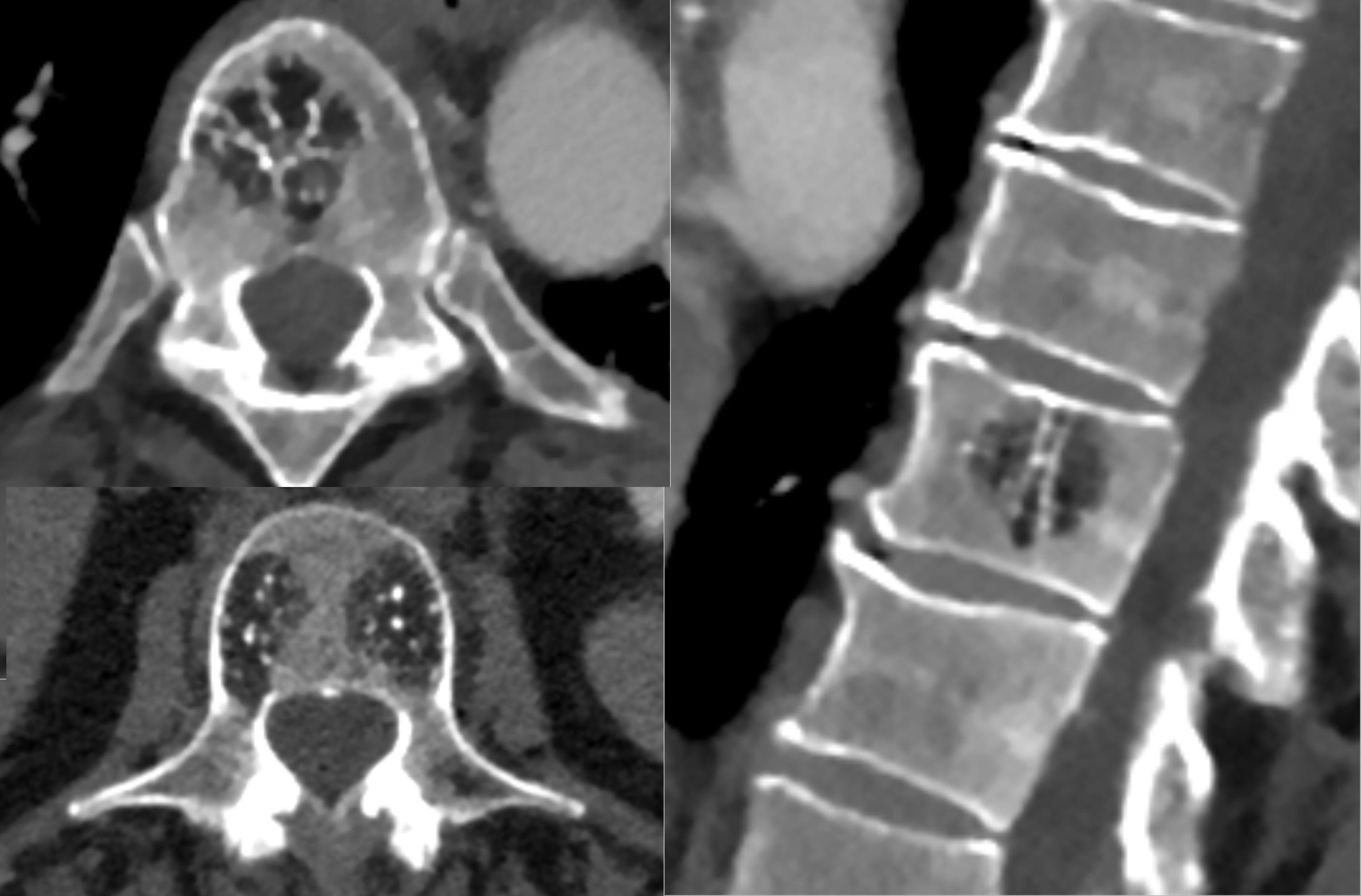
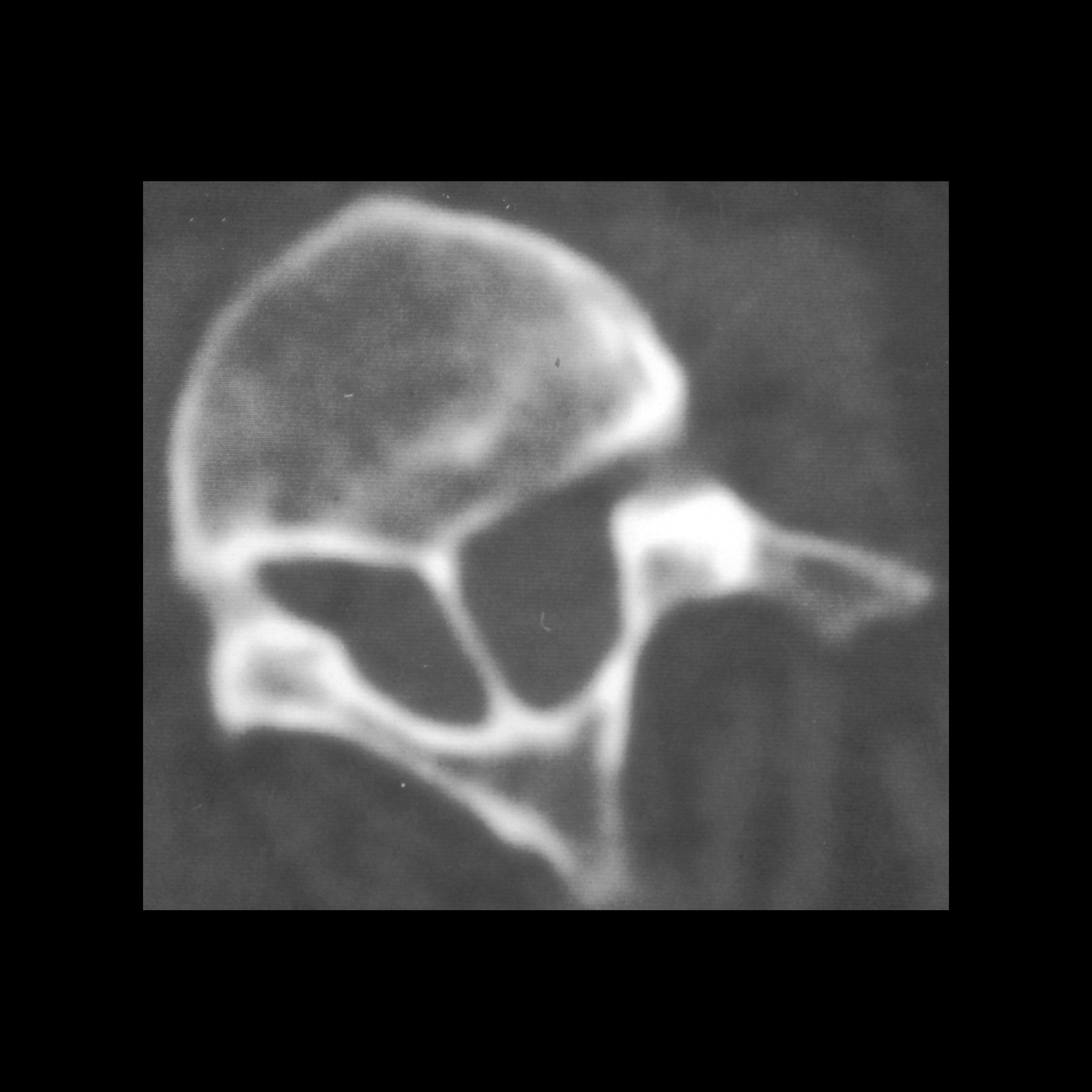
CT
CT is able to better image many of the features seen on plain films and in addition may demonstrate the bony septum.
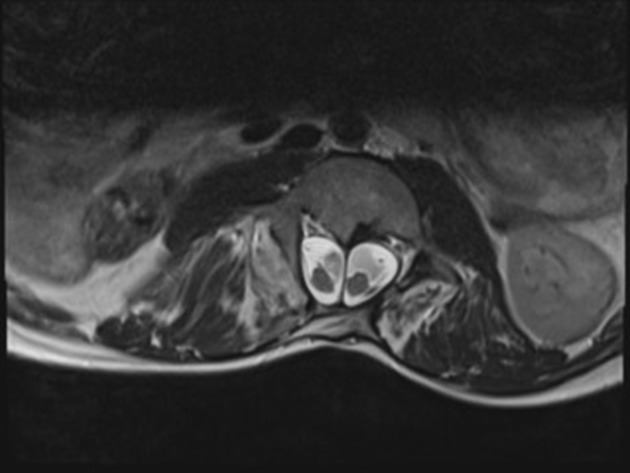
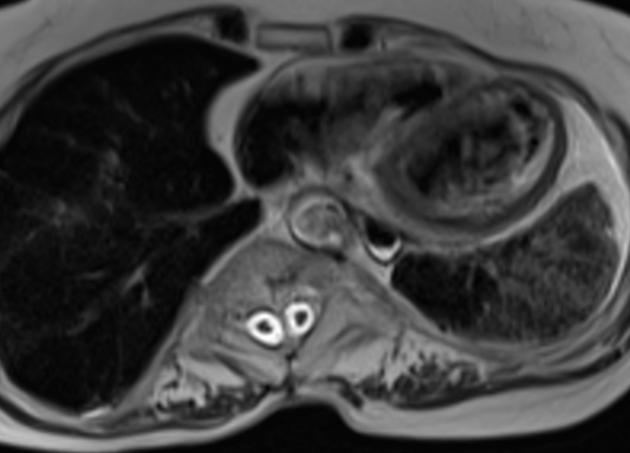
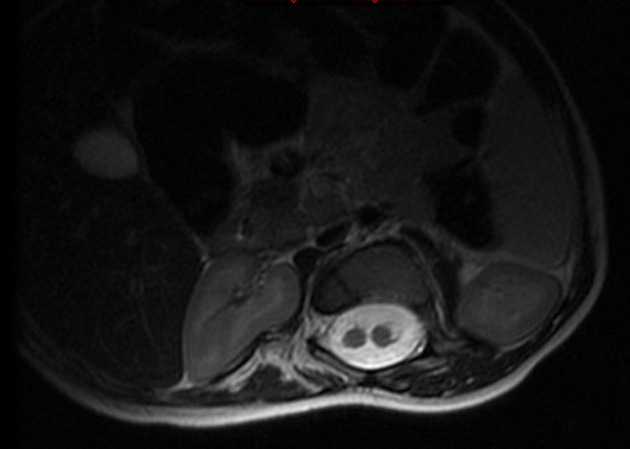
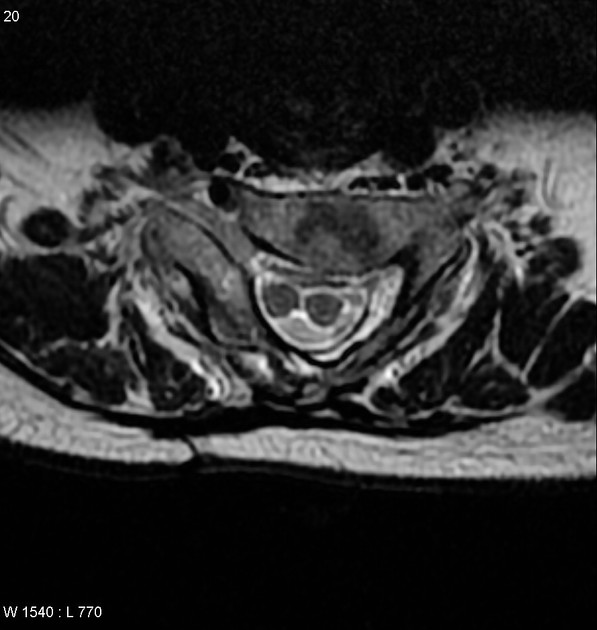
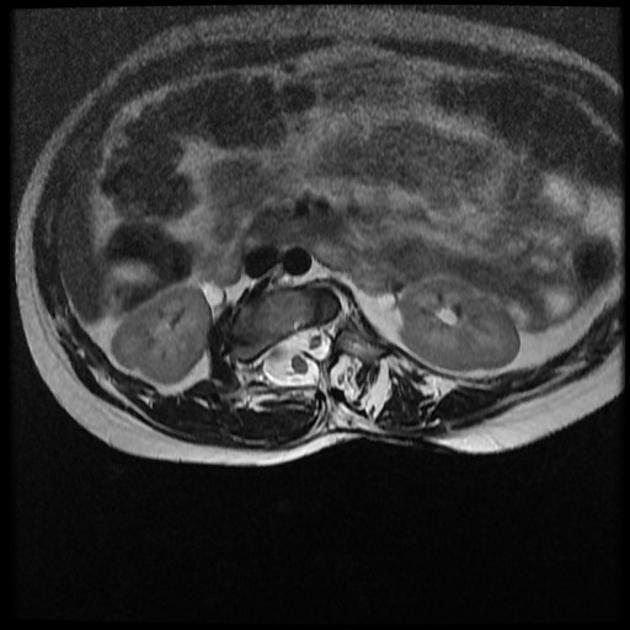
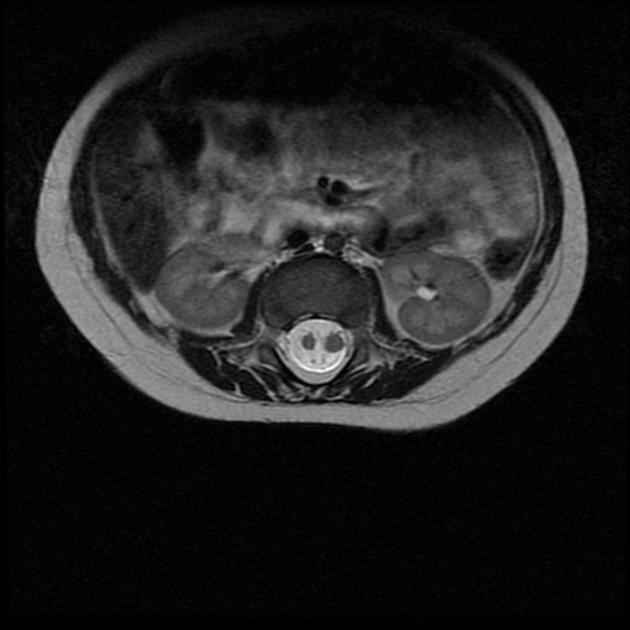
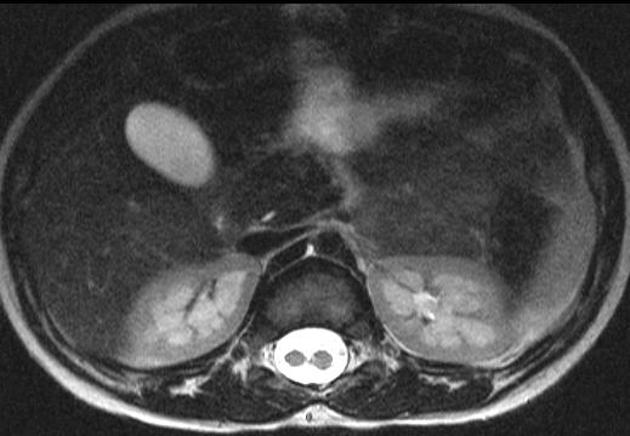
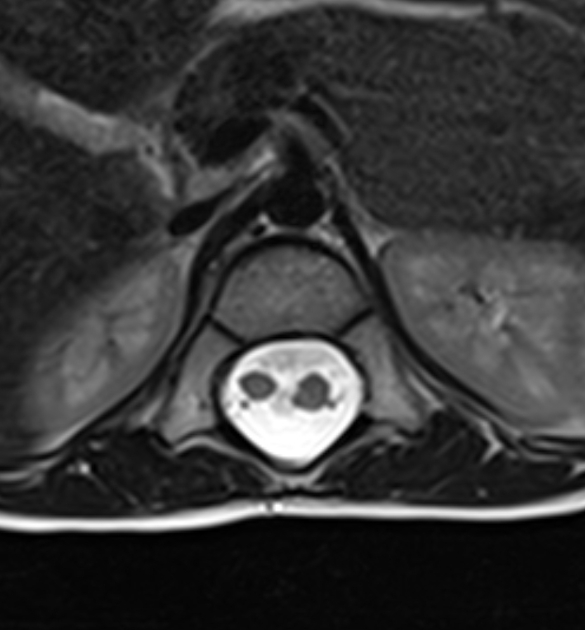
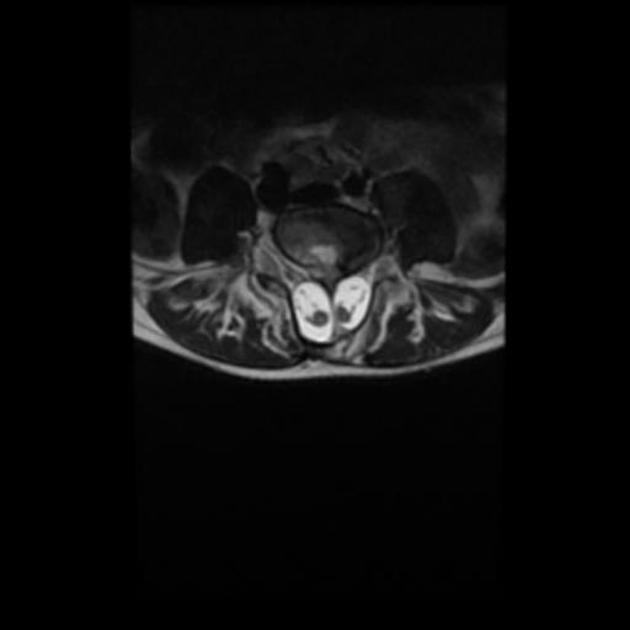
MRI
MRI is the modality of choice for assessing children with split cord malformations. As well as being able to elegantly demonstrate the cord and presence of hydromyelia (if present), it can also assess for the presence of the numerous associated anomalies (see above).
Differential diagnosis
Usually, there is little in the way of a differential diagnosis when the cord has been adequately imaged and features are typical (especially now that diplomyelia is considered part of the same spectrum by many authors ).
Siehe auch:
- Hämangiom der Wirbelsäule
- Schmetterlingswirbel
- Skoliose
- neuroenterische Zyste
- Meningozele
- Cauda equina Lipom
- Sinus pilonidalis
- spinale Dermoidzyste
- Dermalsinus
- Hämangiomatose
- Lipom der Medulla spinalis
- Diplomyelie
und weiter:
- obstetric curriculum
- Klumpfuß
- Myelomeningozele
- erweiterter Spinalkanal
- intraspinale zystische Läsionen
- Erweiterung des interpedunculären Abstands
- diastematomyelia and tethered cord
- diastematomyelia associated with spina bifida occulta and tethered cord
- Dysrhaphie
- double diastematomyelia
- diastematomyelia : cervical spine
 Assoziationen und Differentialdiagnosen zu Diastematomyelie:
Assoziationen und Differentialdiagnosen zu Diastematomyelie: