distal radial fracture











Distal radial fractures are a heterogeneous group of fractures that occur at the distal radius and are the dominant fracture type at the wrist. These common fractures usually occur when significant force is applied to the distal radial metaphysis.
Epidemiology
Distal radial fractures can be seen in any group of patients and there is a bimodal age and sex distribution: younger patients tend to be male and older patients tend to be female.
Clinical presentation
The majority of patients with a distal radial fracture present following a fall onto an outstretched hand. They are in pain and have a reduced range of motion. There may be an associated deformity and in severe cases, distal neurovascular compromise.
Pathology
Etiology
Trauma is almost always the cause of distal radial fractures and is often the result of a fall onto an outstretched hand (FOOSH).
In young adults, the long bones tend to be strong and the force required to break the bone is significant. Thus, distal radial fractures in younger patients require much greater force, e.g. falling from a significant height, severe road traffic accident.
In the elderly, the bones tend to have a much lower bone density and are consequently much weaker. Fracture of the distal radius can occur with injuries that exert much less force, e.g. falling from standing height.
Pathophysiology
Force applied longitudinally or obliquely to the hand and wrist is absorbed by the distal radius because it is the load-bearing bone in the forearm. If this force is greater than the strength of the bone, a fracture occurs.
When most people fall, they do not axially load the forearm but apply an oblique force longitudinally and dorsally. If a fracture does occur, there is usually associated with dorsal angulation.
Classification
They are best described in terms of their fracture type, location, displacement, and joint involvement. Traditionally, eponymous names were given to the common fracture types of the distal radius:
- Colles fracture: transverse extra-articular fracture with dorsal angulation
- Smith fracture: transverse fracture with palmar angulation
- Barton fracture
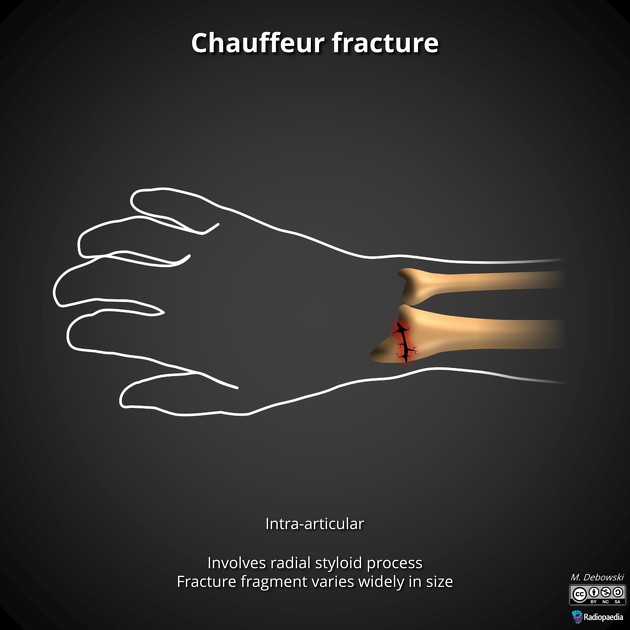
- chauffeur fracture
There are many radiological classification systems, e.g. Frykman classification. However, it is more important to recognize what makes the fracture more severe:
- oblique, spiral or comminuted configuration
- greater degree of angulation
- intra-articular involvement
- additional fractures
- associated dislocation
- distal radioulnar joint (Galeazzi fracture-dislocation)
- lunate / perilunate dislocation
- associated ligamentous injury
Radiographic features
Diagnosis usually only requires a standard wrist x-ray series. In some complex cases, additional cross-sectional imaging (usually CT) is required to accurately assess the fracture. This is especially true when there is a multi-part fracture with joint involvement.
Plain radiograph / CT
Most distal radial fractures in adult patients are transverse metaphyseal fractures. They are often extra-articular, but some may extend into the joint, and when they do, it is important to recognize. The degree of displacement (usually dorsal) is important because it will be a determining factor for treatment (whether to reduce or not before immobilization).
When describing the fracture, think about:
- what type of fracture is it?
- is there displacement?
- is there joint involvement?
- is there an accompanying ulnar styloid fracture?
Treatment and prognosis
Treatment is dependent on the type of fracture (as determined by the x-ray). The vast majority of distal radial fractures are relatively uncomplicated and can be conservatively managed as an outpatient with review in fracture clinic.
Fractures with significant displacement require manipulation (under sedation or anesthetic). A small number will require internal fixation (e.g. with a volar locking plate) following manipulation.
A small proportion of patients treated conservatively need to be followed up. If a fracture is stable and treated in cast it must be reviewed regularly because of the risk of displacement. This is particularly true if the cast becomes loose once the wrist swelling subsides. Late displacement warrants surgical consideration.
Siehe auch:
- Frakturen mit Eigennamen
- Chauffeur-Fraktur
- Galeazzi-Fraktur
- Fourchette-Stellung
- Colles-Fraktur
- Monteggia-Fraktur
- Barton Fraktur
- Bajonett-Stellung
- fracture-dislocations of the radius and ulna
- Smith-Fraktur
- Essex-Lopresti fracture
- reverse Barton fracture
- fall onto an outstretched hand (FOOSH)
und weiter:
- frykman classification of distal radial fractures
- navicular fracture
- proximale Humerusfrakturen
- Reverse Barton-Fraktur
- fall onto an outstretched hand
- Scaphoidfraktur
- Radius (Anatomie)
- Radiusfraktur
- Kapandji-Osteosynthese
- AO Klassifikation Radiusfrakturen
- Wulstfraktur des distalen Radius
- AO Klassifikation distale Radiusfraktur
- radiologisches muskuloskelettales Curriculum
- buckle fracture of distal radius
- ipsilateral fractures of distal radius, scaphoid and capitate
- dorsal tilt of the distal radius

 Assoziationen und Differentialdiagnosen zu distale Radiusfraktur:
Assoziationen und Differentialdiagnosen zu distale Radiusfraktur:









