intradural extramedullary metastases
Intradural extramedullary metastases are rare and only account for approximately 5% of spinal metastases.
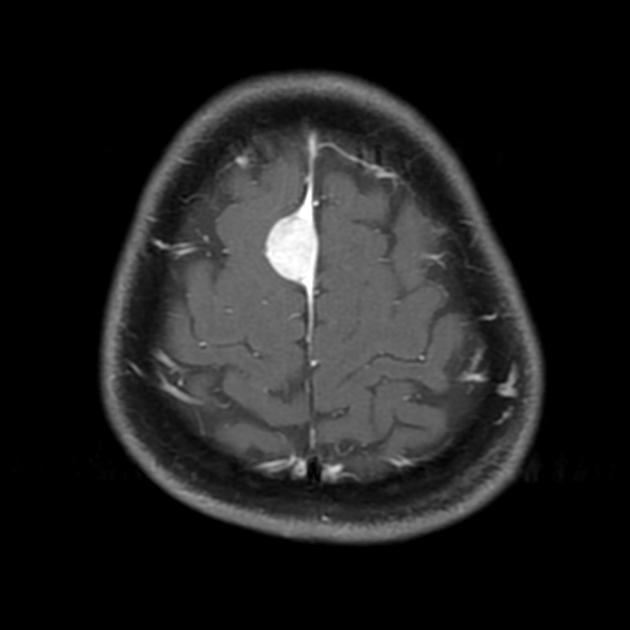
Please review leptomeningeal metastases (brain) for a general discussion focused on the brain's subarachnoid space involvement.
Epidemiology
The age at presentation depends on tumor type. Metastases from central nervous system malignancies generally occur at a younger age.
Clinical presentation
Presentation is highly variable. As the most commonly affected site is the lumbosacral spine, symptoms and signs include back or radicular pain, weakness, paresthesias, gait disturbance, cauda equina syndrome and symptoms/signs of meningeal irritation.
Pathology
In the pediatric population, the most common intradural extramedullary neoplasms are leptomeningeal metastases resulting from primary brain tumors whereas in adults non-CNS tumors are most commonly encountered. Multiple lesions are common.
Primary tumors include:
- CNS (drop metastases)
- cerebral glioblastoma
- anaplastic astrocytoma
- ependymoma and myxopapillary ependymoma
- posterior fossa medulloblastoma (PNET-MB)
- pineal tumors (e.g. germinoma, pineoblastoma)
- choroid plexus neoplasms
- non-CNS
- solid tumors
- melanoma
- haemopoietic neoplasms
- papillary carcinoma of thyroid
Radiographic features
Plain films and CT are inadequate for the assessment of possible leptomeningeal metastatic disease, and in these cases, MRI is required.
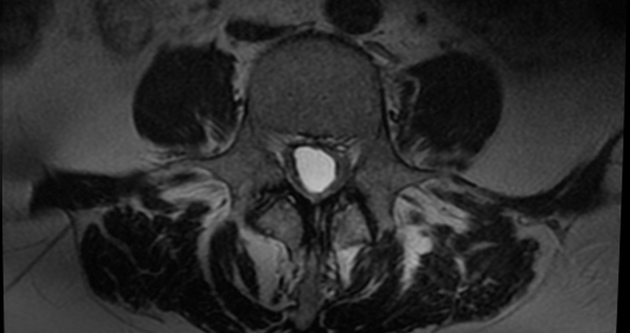
MRI
MRI without contrast may be normal, and thus when suspected contrast should be administered. Typical signal characteristics include:
- T1: thickened nerve roots or nodular lesions that are isointense with the spinal cord may be seen
- T2: cord edema may be seen with more extensive disease, especially if there is an intramedullary component
- T1 C+ (Gd)
- enhancing tumor nodules on the spinal cord, nerve roots or cauda equina.
- “sugar coating” of the spinal cord and nerve roots
Treatment and prognosis
Prognosis is poor, and depends on the primary tumor. No surgical cure is possible, and treatment revolves around systemic chemotherapy and radiotherapy to the neuraxis (again, this depends on the primary tumor).
Differential diagnosis
If diffuse (sugar coating) consider:
- meningoradiculitis
- homogeneously enhancing CSF
- CSF correlation useful
- arachnoiditis
- clumping of nerve roots
- "empty sac sign"
- often history of prior surgery
- Guillain-Barre syndrome
- smooth pial enhancement of cauda equina and conus medullaris
- history of recent viral illness is typical
If nodular (mostly at cauda equina) consider:
- spinal meningioma
- multiple meningiomas are most often associated with NF2
- dural tail sign
- spinal neurilemmoma/schwannoma
- multiple schwannomas are often associated with NF2
- frequently associated with hemorrhage, intrinsic vascular changes, cyst formation and fatty degeneration
- spinal neurofibroma
- multiple neurofibromes are often associated with NF1
- leptomeningeal (pial) lipoma
- follows fat signal intensity
- no enhancement
- post-arachnoiditic adhesions
See also
- intradural extramedullary spinal tumors
- neoplasms of the spinal canal
- intradural extramedullary spinal tumors (mnemonic)
Siehe auch:
- chronisch adhäsive Arachnopathie
- neoplasms of the spinal canal
- spinale Schwannome
- spinal neurofibroma
- intraspinales Meningeom
- sugar coating
- Guillain-Barré-Syndrom
- empty sac sign
- intradurale extramedulläre Tumoren
- Dural-Tail-Zeichen
und weiter:

 Assoziationen und Differentialdiagnosen zu intradural extramedullary metastases:
Assoziationen und Differentialdiagnosen zu intradural extramedullary metastases: