Intramedullary spinal tumors



Intramedullary spinal tumors are rare, representing 4-10% of all CNS tumors and less than 10% of all pediatric CNS neoplasms . They account for 20% of all intraspinal tumors in adults and 35% of all intraspinal tumors in children .
A long duration of symptoms prior to diagnosis is typical.
Pathology
Classification
They can be classified according to many ways:
- intramedullary neoplastic lesion
- glial neoplasms: 90-95% of all intramedullary tumors
- spinal ependymoma: 60% of all glial spinal cord tumors
- spinal astrocytoma: 33% of all glial spinal cord tumors
- spinal ganglioglioma: 1% of all glial spinal cord tumors
- spinal glioblastoma multiforme (primary): 7.5% of all intramedullary gliomas and only 1.5% of all spinal cord tumors
- non-glial neoplasms
- highly vascular lesions
- other rare lesions
- glial neoplasms: 90-95% of all intramedullary tumors
- intramedullary benign masses
Associations
Intramedullary spinal neoplasms are more common in patients with neurofibromatosis:
- ependymomas occur more often in patients with NF2
- astrocytomas occur more often in patients with NF1
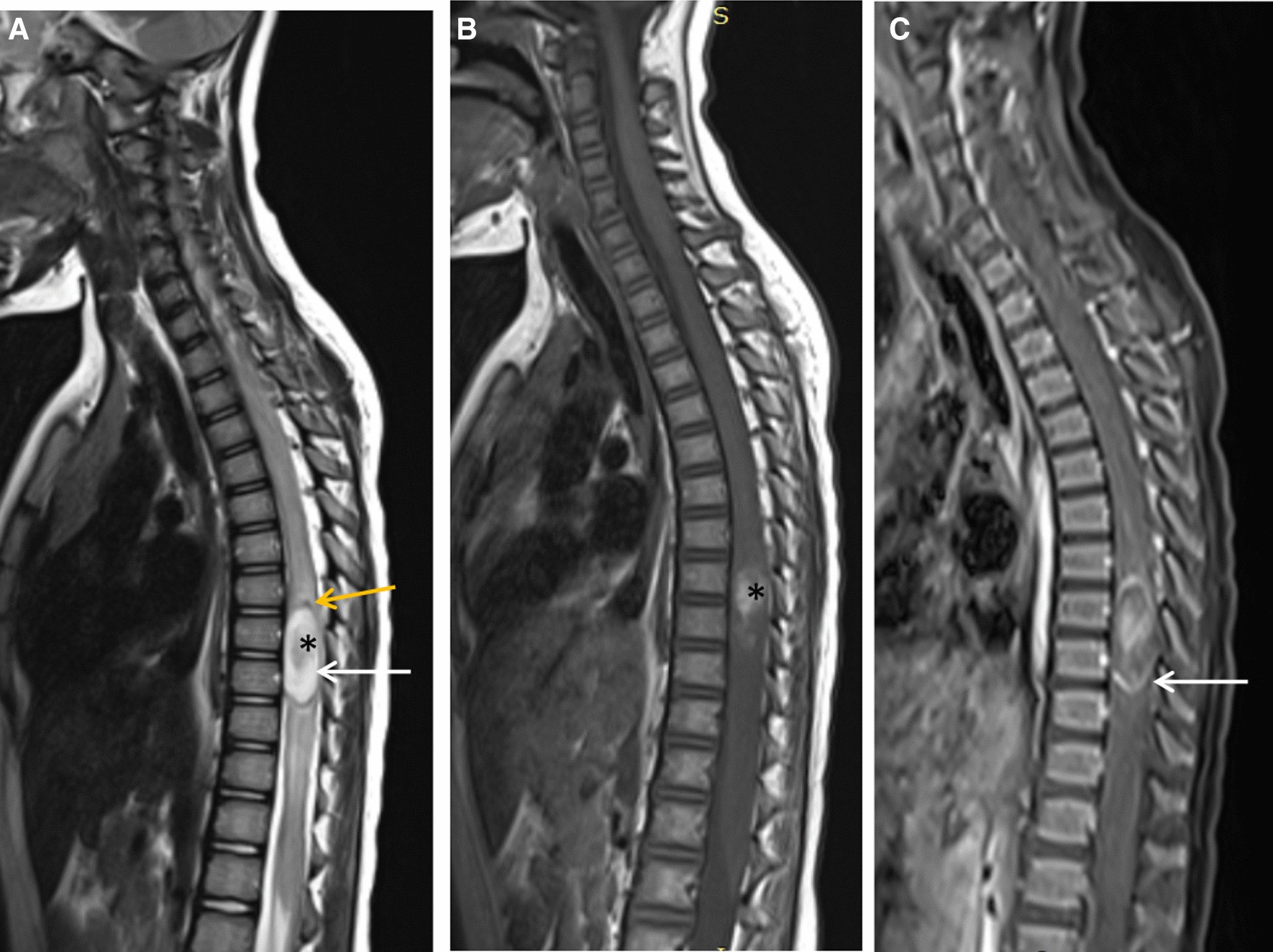
Approximately 70% of intramedullary tumors are associated with cysts . Two types of cysts are recognized:
- tumoral (or intratumoral) cysts
- contained within the tumor itself
- typically demonstrate peripheral enhancement
- may result from necrosis, fluid secretion, or degeneration of the neoplasm
- need to be resected along with the solid portion of the tumor because there is a high likelihood of neoplastic cells within the cyst wall
- occurs in association with the following proportion of tumors
- spinal ganglioglioma: in 46%
- spinal ependymoma: in 22%
- spinal astrocytoma: in 21%
- spinal hemangioblastoma: in 2-4%
- non-tumoral (or reactive) cysts
- occur rostral or caudal to the solid portion of the tumor
- occur due to dilatation of the central canal
- do not enhance
- present in 60% of all intramedullary spinal tumors
- may resolve once the neoplasm is resected
Syringomyelia occurs in approximately 50% of all intramedullary tumors but is most frequently associated with hemangioblastomas .
Clinical presentation
The presentation of intramedullary tumors depends on their size and location. The most common presenting symptoms include back/neck pain, radicular pain, weakness, paresthesia, gait disturbance and bowel and bladder dysfunction. Brown-Sequard syndrome may occur. An uncommon presentation is acute headache due to subarachnoid hemorrhage .
In children, progressive scoliosis may be seen. Motor regression and frequent falls may be the presenting features in young children .
Symptoms are usually slowly progressive. Due to their non-specific nature, the diagnosis is often delayed. An exception is intramedullary metastastases, which are diagnosed within one month of symptom onset in up to 75% of cases .
Radiographic features
Plain film
Widening of the interpedicular distance may be seen in less than 10% of cases
CT
Generally not useful because bony changes are relatively rare.
Myelography
- the spinal cord can be enlarged
- gradual subarachnoid space effacement
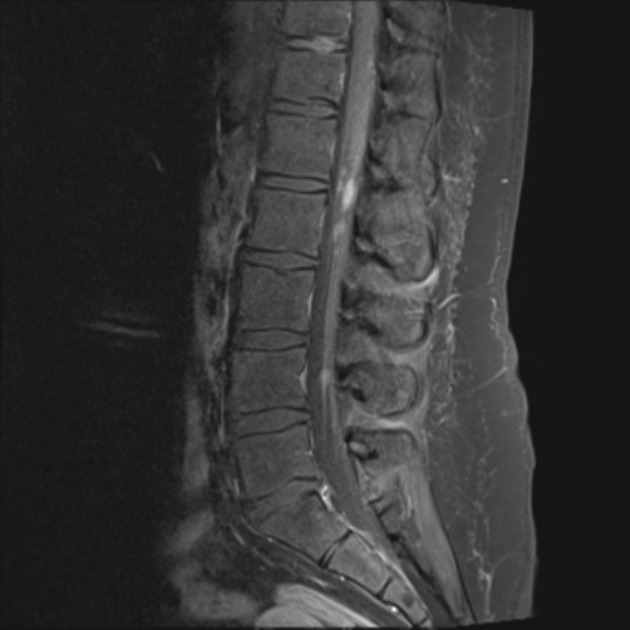
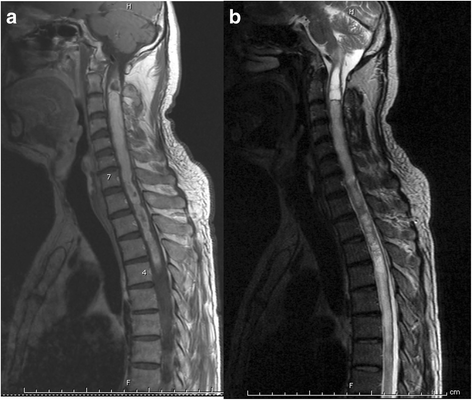
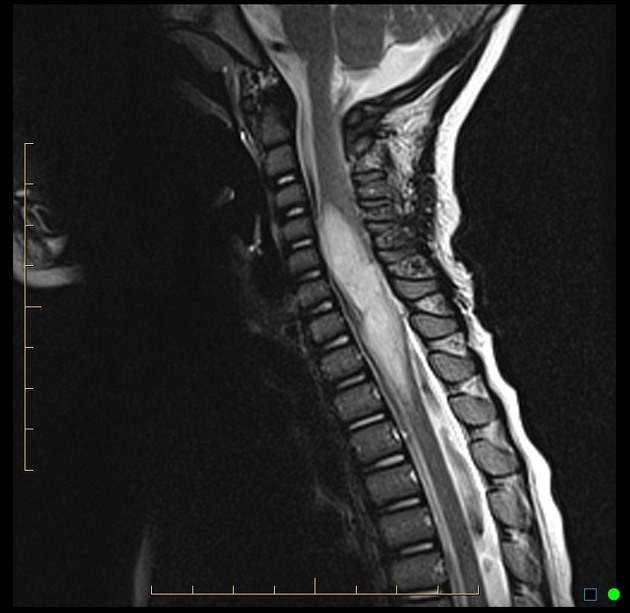
MRI
3 general characteristics of intramedullary neoplasms are recognized on MRI:
Differential diagnosis
Various lesions may mimic intramedullary tumors. The differential diagnosis of intramedullary tumors includes:
- vascular lesions
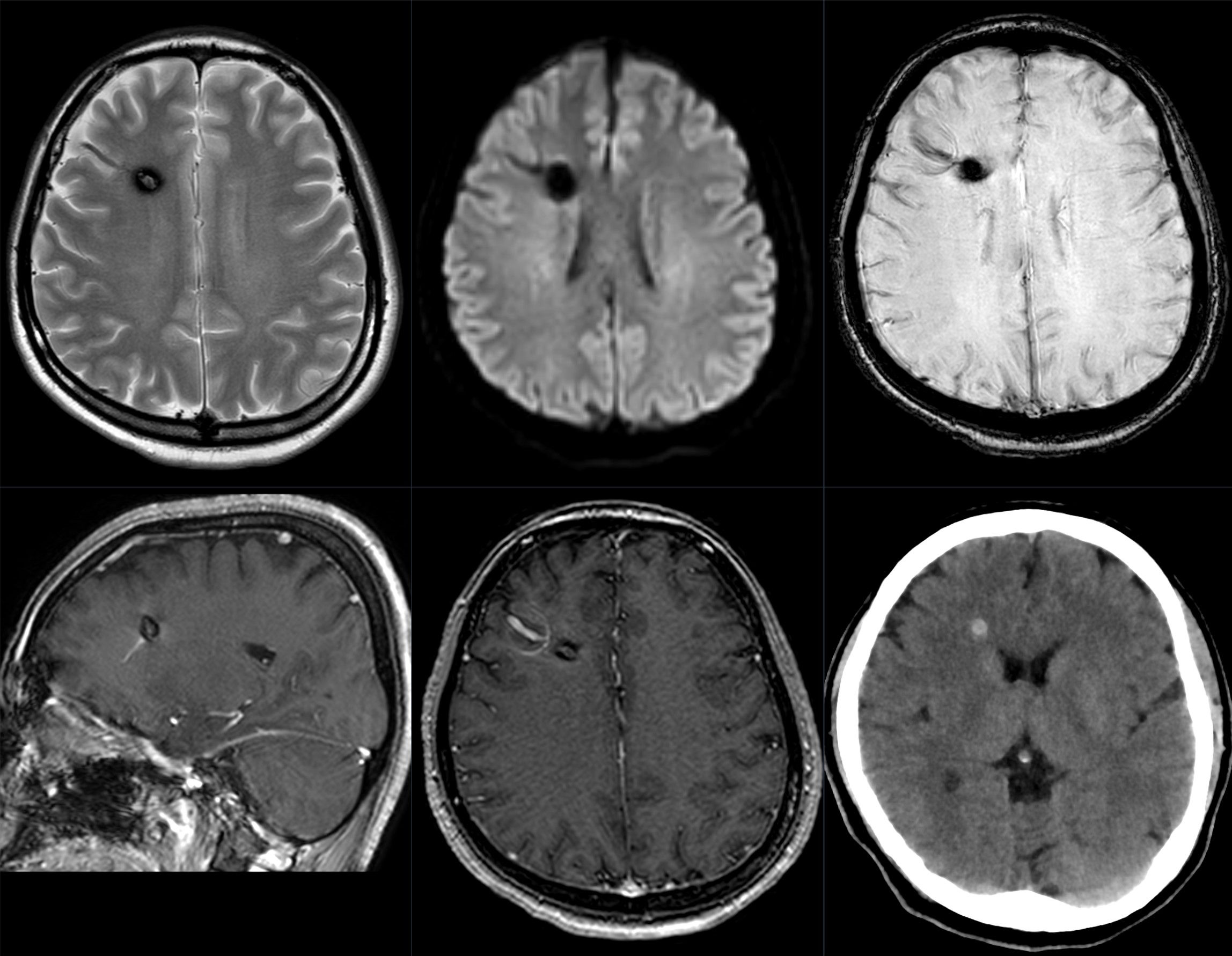
- cavernous malformation (cavernoma)
- rounded regions of heterogeneous signal intensity on T1 and T2 weighted images due to blood
- products of varying ages (“popcorn appearance”)
- low signal intensity rim on T2 weighted images (hemosiderin)
- hypointense “blooming” on gradient echo sequences (hemosiderin)
- may demonstrate minimal enhancement on post-contrast images
- minimal cord expansion or edema unless there has been recent hemorrhage
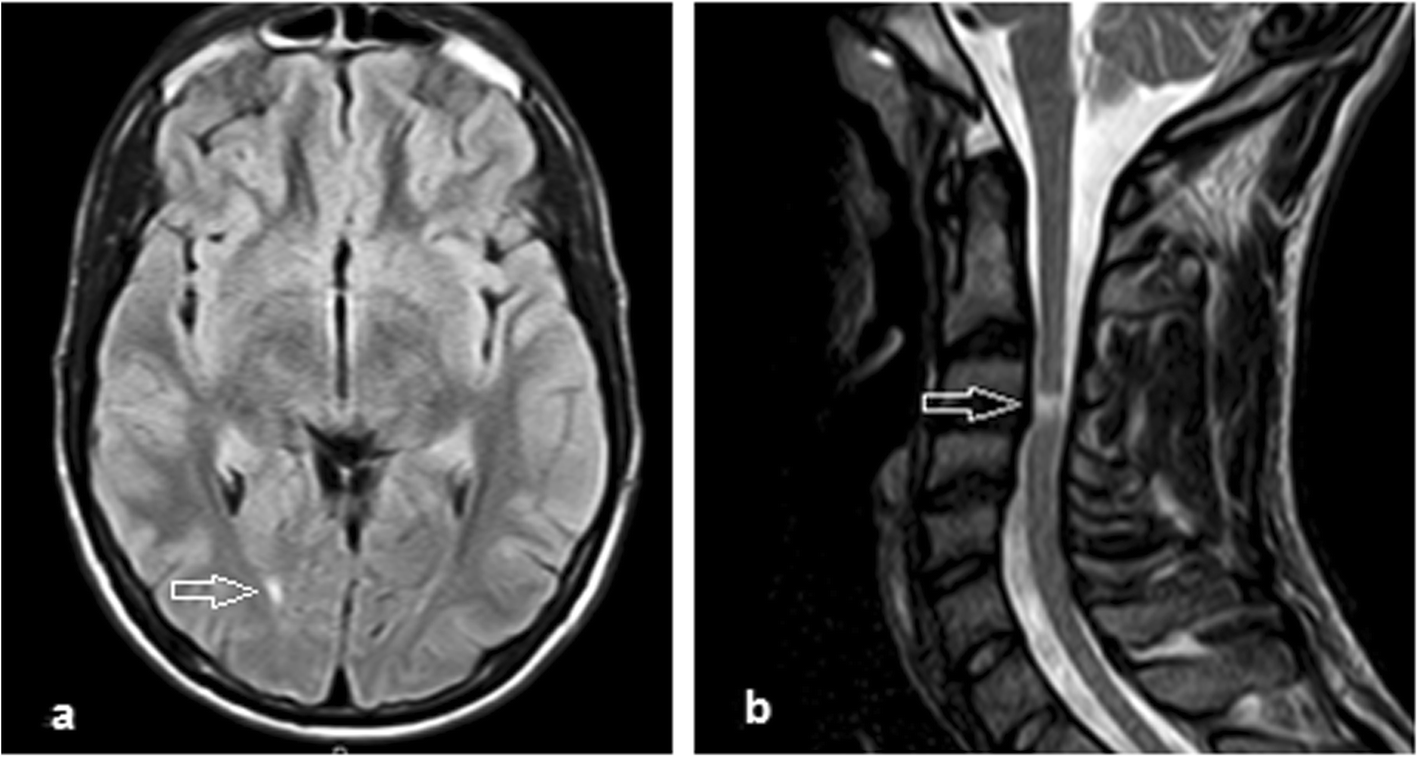
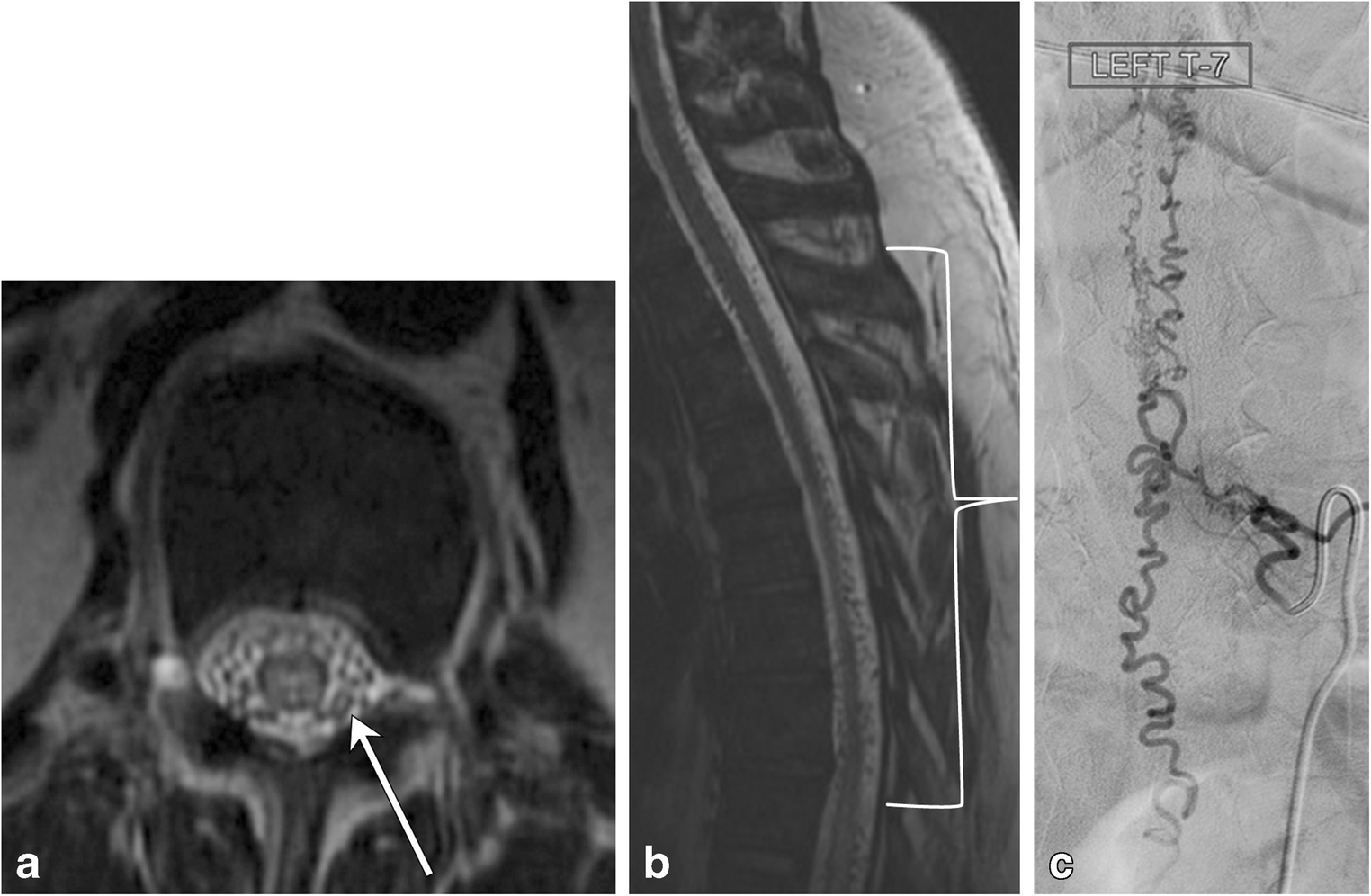
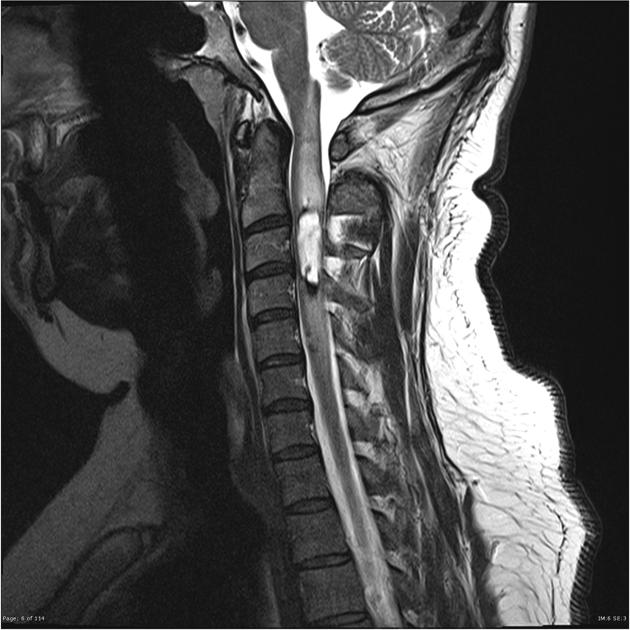
- dural arteriovenous fistula (DAVF)-(type I AVM)
- spinal cord may be normal size or enlarged
- hyperintense on T2 weighted images (due to edema)
- prominent vessels (flow voids) are usually present on the posterior aspect of the cord
- variable enhancement on post-contrast images
- typically located in the dorsal aspect of the lower thoracic cord and conus medullaris
- spinal cord infarction
- spinal cord is usually enlarged
- hyperintense on T2 weighted images and DWI
- post-contrast enhancement may or may not be present (enhancement is usually present in the subacute stage)
- signal intensity abnormality may be limited to the central grey matter or may involve most of the cross sectional area of the cord
- signal abnormality typically extends over multiple vertebral body segments
- can occur at any location in the cord but has a propensity for the upper thoracic or thoracolumbar regions
- vertebral body T2 hyperintensity may occasionally be seen (due to concomitant infarction)
- cavernous malformation (cavernoma)
- inflammatory lesions
- demyelination (e.g. multiple sclerosis)
- usually no spinal cord enlargement (enlargement is seen in 6-14% cases)
- plaques are generally shorter than two vertebral body segments in length and involve less than half the cross-sectional area of the cord
- characteristically peripherally located in the dorsal and lateral columns
- isointense to hypointense on T1 weighted images (unlike brain plaques, cord plaques may not be visible as areas of hypointensity on T1 weighted imaegs)
- hyperintense on T2 weighted images
- signal abnormality is typically poorly marginated
- plaque enhancement correlates with acute lesion activity (usually lasts less than two months)
- in most patients additional lesions of variable enhancement are present in the brain and spinal cord (MS is solely confined to the spinal cord in 5-24% of patients )
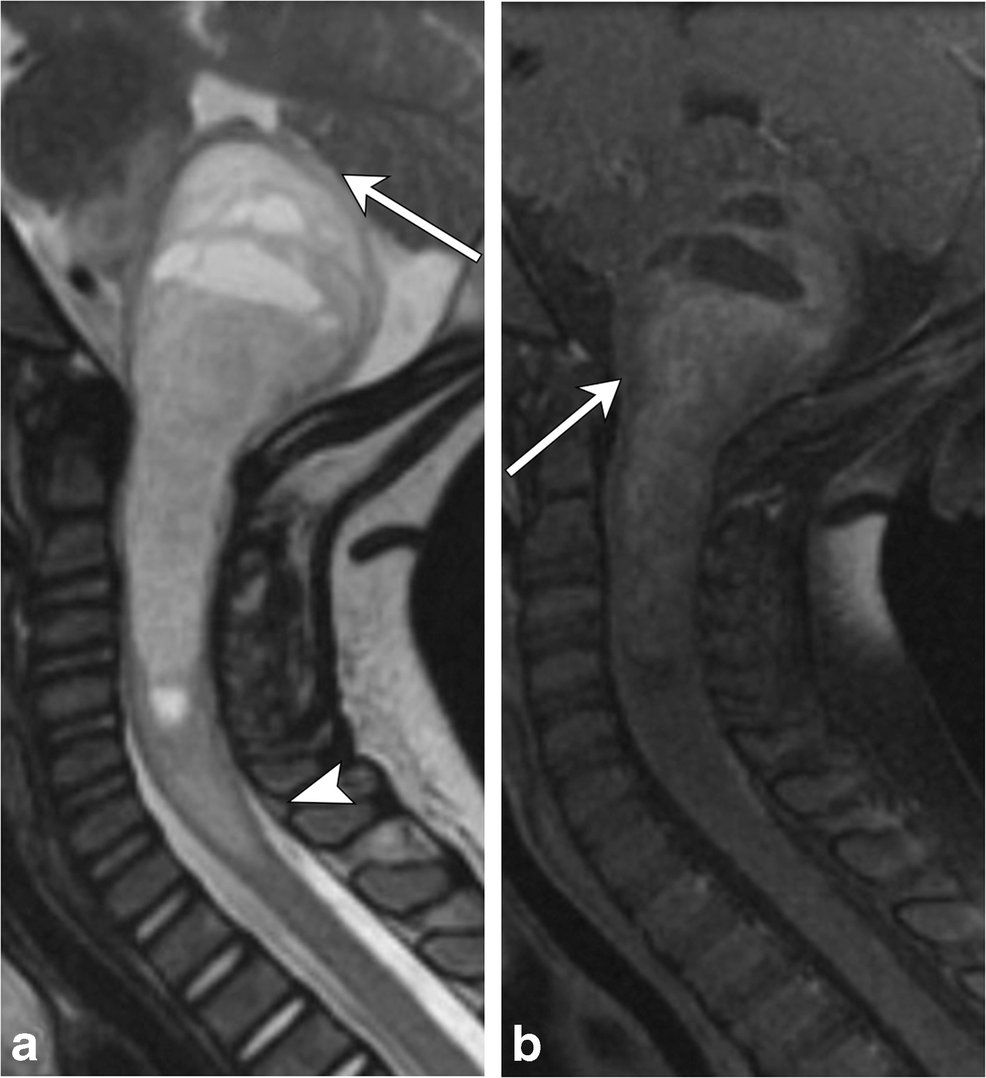
- transverse myelitis
- variable enlargement of the spinal cord
- hyperintense on T2 weighted images and iso- or hypointense on T1 weighted images
- variable enhancement patterns (none, diffuse, patchy, peripheral)
- lesions commonly extend for 3-4 spinal segments
- lesions typically occupy greater than two thirds of the cross-sectional area of the cord
- acute clinical course
- spinal cord abscess
- core is hypointense on T1 weighted images and hyperintense on T2 weighted images
- rim enhancement
- cord expansion
- may show restricted diffusion on DWI
- may have adjacent vertebral or disc abnormalities
- demyelination (e.g. multiple sclerosis)
- spinal cord contusion (acute)
- isointense to hypointense on T1 weighted images, hyperintense on T2 weighted images
- cord swelling
- usually associated with other spinal injuries (osseous, disc, vascular)
See also
Siehe auch:
- Transverse Myelitis
- Encephalomyelitis disseminata
- neoplasms of the spinal canal
- durale AV-Fistel
- Kavernom
- intramedulläres Astrozytom
- spinales Astrozytom
- intradurale extramedulläre Tumoren
- intramedulläres Ependymom
- intramedullary metastases (spinal)
und weiter:
- intramedullary spinal metastasis
- spinale Epidermoidzyste
- spinales Hämangioblastom
- Rückenmarksinfarkt
- intradural spinal mass lesions - an approach
- holocord presentation
- spinale Dermoidzyste
- spinale durale arteriovenöse Fistel
- spinal T2 hyperintense lesions
- intraspinale Tumoren
- Sarkoidose Rückenmark
- intramedulläre spinale Tuberkulose
- Gangliogliom des zervikalen Rückenmarks
- spinales Oligodendrogliom

 Assoziationen und Differentialdiagnosen zu Intramedullary spinal cord tumor:
Assoziationen und Differentialdiagnosen zu Intramedullary spinal cord tumor: