Leriche-Syndrom



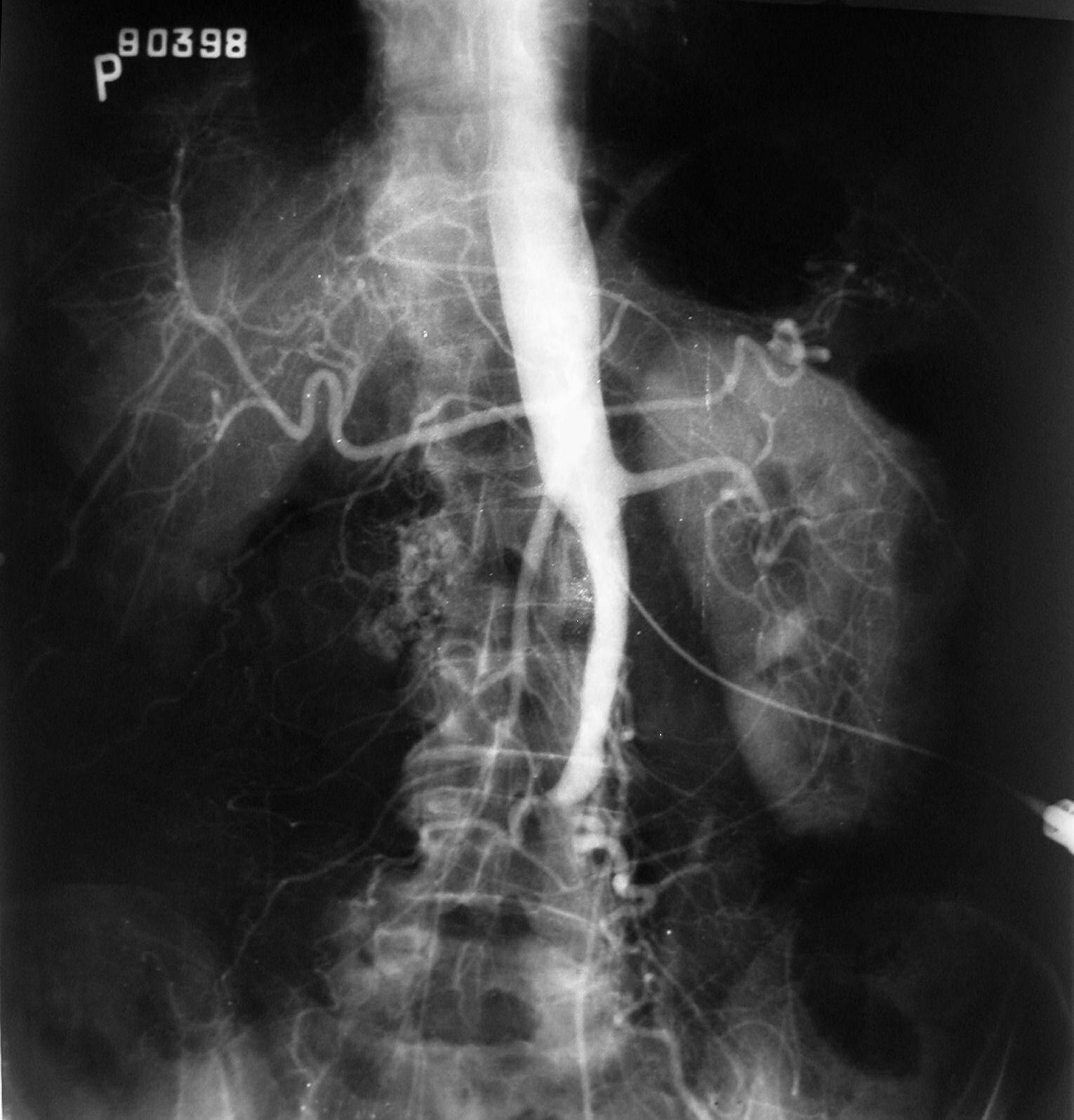
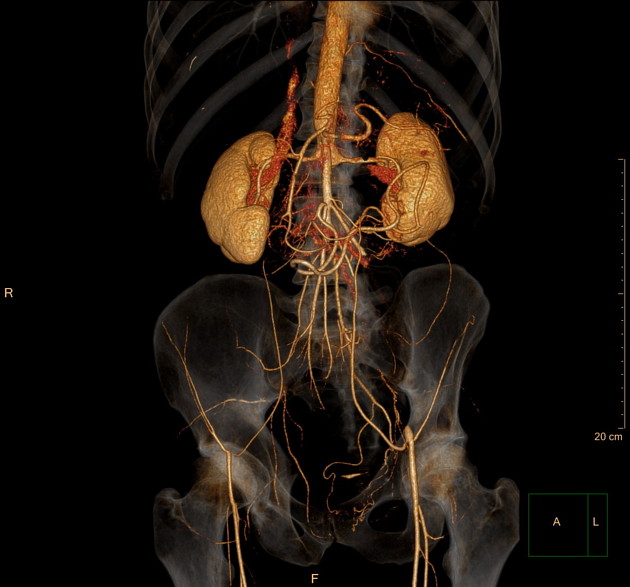


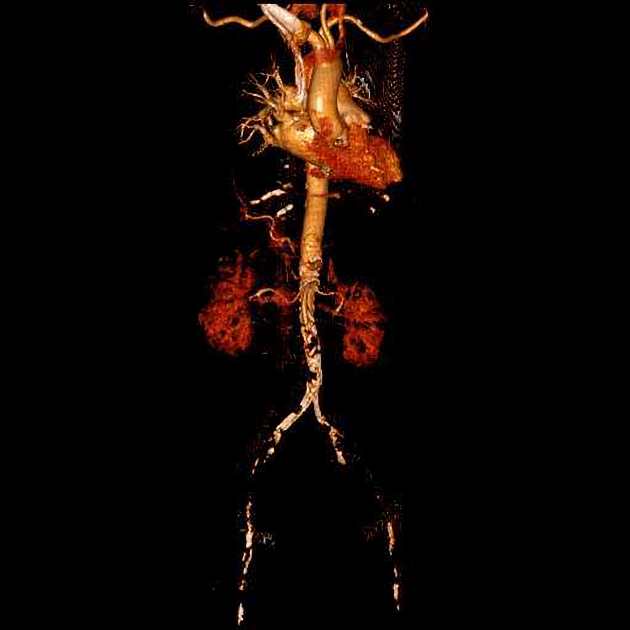
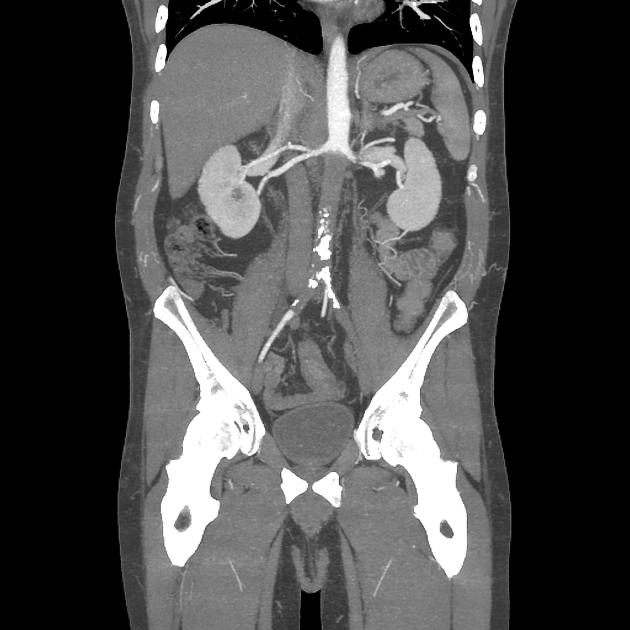
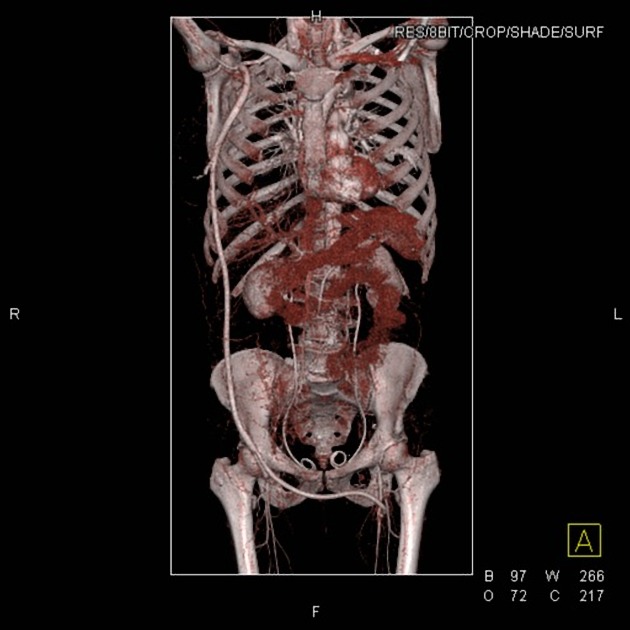




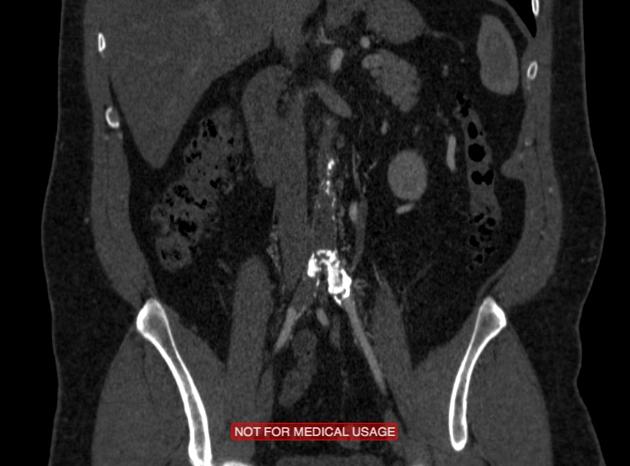


Aortoiliac occlusive disease, also commonly termed as Leriche syndrome refers to complete occlusion of the aorta distal to the renal arteries.
Terminology
Originally the triad of erectile dysfunction, pelvis and thigh claudication, with absence of the femoral pulses was described as Leriche syndrome, which usually affects younger (30-40 year old) males . However, in contemporary use all aortoiliac occlusions with absent femoral pulses are commonly summarized under this eponym, concomitant sexual dysfunction being often, but not necessarily present .
Clinical presentation
Aortoiliac occlusive disease is more common in the elderly with an advanced atherosclerotic disease. Acute onset is more common in female patients and is associated with poor outcome with approximately 50% mortality.
In acute cases, symptoms include the 6 Ps:
- pain
- pulselessness
- pallor
- paresthesia
- paralysis
- prostration
In chronic onset cases, mostly in arteriosclerosis, symptoms may include erectile dysfunction or impotence, claudication and absence of femoral pulses .
Classification
The anatomical location of atheromatous lesions influence the classification and treatment choice :
- type I: confined to distal abdominal aorta and common iliac arteries
- type II: as above with extension into the external iliac arteries
- type III: aortoiliac segment and femoropopliteal vessels
According to the Trans Atlantic Inter Society Consensus II (TASC II) Leriche syndrome is a type D lesion .
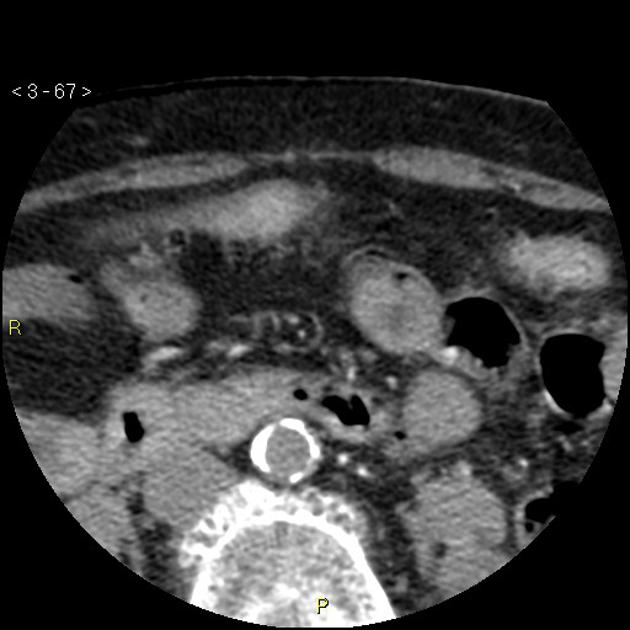
Pathology
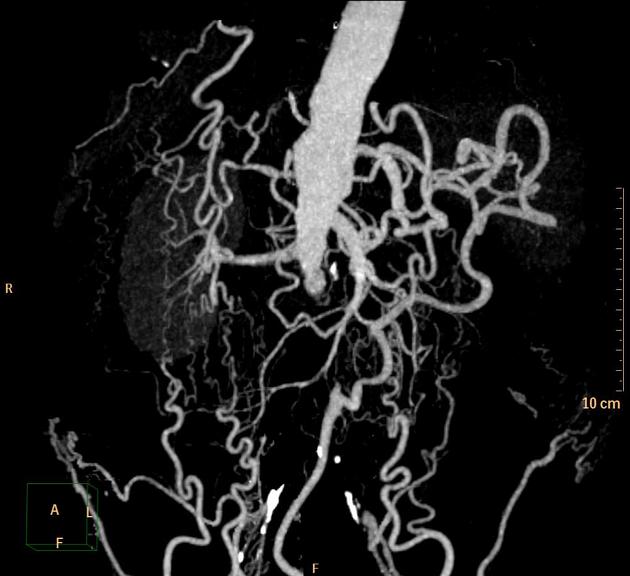
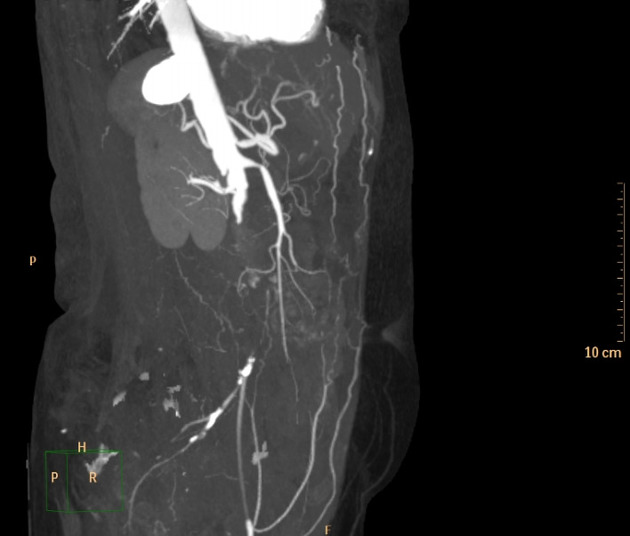
The condition can be acute or chronic. There is endothelial damage resulting in inflammation and lipid accumulation in the tunica media and macrophages eventually leading to plaque formation and occlusive disease . Complete infra-renal aortoiliac occlusion will display significant collateral circulation sustained by multiple anastomoses allowing reconstitution with the distal femoral arteries .
Location
Most often the occlusion occurs near the aortic bifurcation. It typically begins at the distal aorta or common iliac artery origins and slowly progresses proximally and distally over time.
Etiology
- arteriosclerosis: the main cause of this syndrome is an atherosclerotic obstruction of aortoiliac arteries
- vasculitis
- thrombosis
An extensive network of collateral parietal and visceral vessels may form to bypass any segment of the aortoiliac arterial system. In abdominal aortoiliac stenosis/occlusion, the commonest collateral pathways to the lower extremities are :
- superior mesenteric artery > inferior mesenteric artery > superior rectal artery >
- intercostal, subcostal, and lumbar arteries > superior gluteal and iliolumbar arteries > internal iliac arteries > external iliac arteries.
- intercostal, subcostal, and lumbar arteries > circumflex arteries > external iliac arteries
- subclavian arteries > internal thoracic (mammary) arteries > superior epigastric arteries > inferior epigastric arteries > external iliac arteries (the Winslow Pathway )
Radiographic features
CT angiography is usually the best modality for assessment. In patients where CT is not possible, contrast-enhanced MR angiography may be a good option .
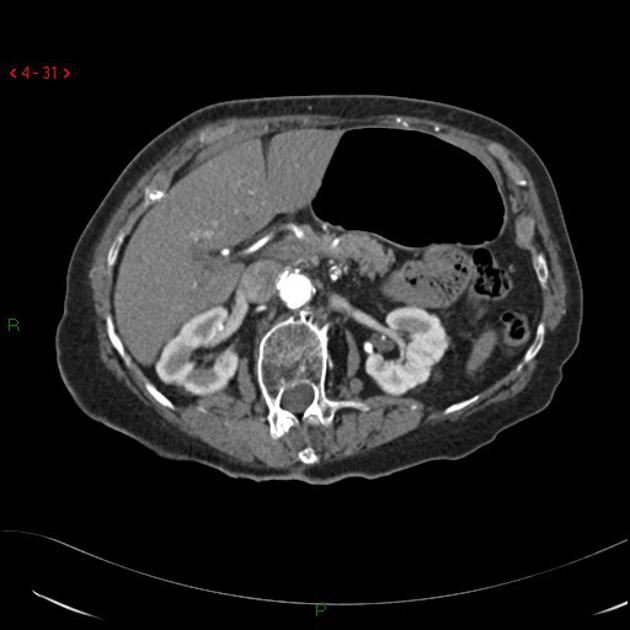
CT angiography
It allows direct anatomical visualization of the location of the stenosis and occlusion. It also permits the assessment for the presence of a concomitant occlusive disease affecting visceral arteries, the type and extent of collateralization, and the level of the most proximal and distal arterial segments amenable to stent-graft placement.
Treatment and prognosis
Traditional surgical procedures for aortoiliac occlusive disease are :
- aortoiliac endarterectomy (TEA)
- aortobifemoral bypass (AFB)
- patency rates of 90% at five years and 80% at ten years
- Tasc II type D lesions recommend surgery as the treatment of choice
- axillobifemoral bypass (extra-anatomic technique); used to avoid abdominal surgery
- percutaneous transluminal angioplasty (PTA) and stenting
Other more novel methods include
- covered endovascular reconstruction of aortic bifurcation (CERAB) technique
History and etymology
It is named after French vascular surgeon René Leriche (1879–1955) who initially described the findings in 1948 .
Differential diagnosis
Imaging differential considerations include:
- mid-aortic syndrome: occurs at or above renal artery level with the involvement of a longer segment and usually in much younger patients (usually 10-30 years old)
Siehe auch:
und weiter:

 Assoziationen und Differentialdiagnosen zu Leriche-Syndrom:
Assoziationen und Differentialdiagnosen zu Leriche-Syndrom:
