malignant fibrous histiocytoma (MFH)

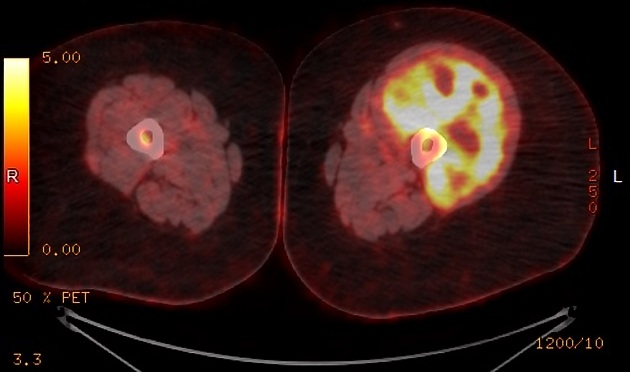





Undifferentiated pleomorphic sarcoma (UPS), previously known as malignant fibrous histiocytoma (MFH), is considered the most common type of soft tissue sarcoma. It has an aggressive biological behavior and a poor prognosis.
As in the majority of the cases, UPS affects the extremities, this article focuses on musculoskeletal involvement. For other rarer sites, please refer to specific articles:
Terminology
Malignant fibrous histiocytoma (MFH) was removed from the 2013 World Health Organization Classification of Tumors of Soft Tissue and Bone .
Epidemiology
Typically, UPS occurs in adults (range 32-80; mean 59 years) with a slight male predilection with an M: F ratio of 1.2:1) .
Clinical presentation
The presentation is usually with a painless, enlarging palpable mass.
Pathology
UPS are aggressive tumors which account for 25-40% of all adult soft tissue sarcomas, making them the most common type. However, the classification system is becoming more restrictive, with many tumors being re-classified as variants of myogenic sarcomas . Currently, it accounts for ~5% of adult sarcomas .
Risk factors
They are the most frequent soft tissue sarcoma to occur as a result of radiotherapy and are also seen on a background of Paget disease. Secondary transformation into the malignant sarcomas like UPS, have also been reported in fibrous dysplasia, giant cell tumor, enchondroma, chronic osteomyelitis, and osteonecrosis .
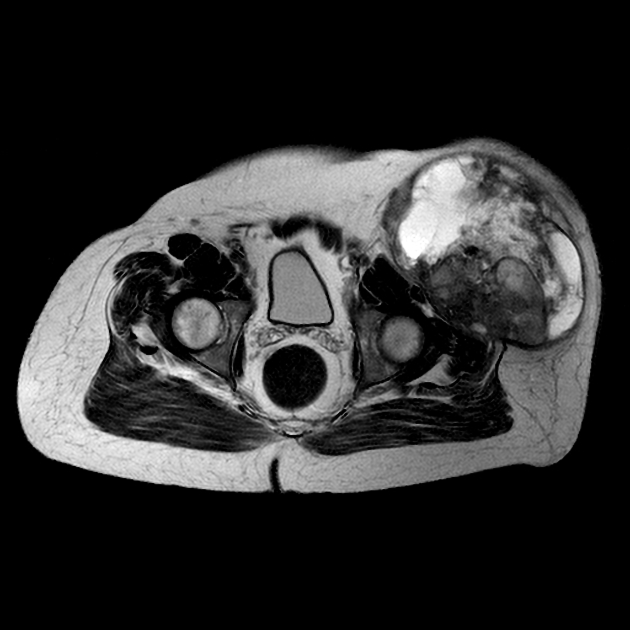
Location
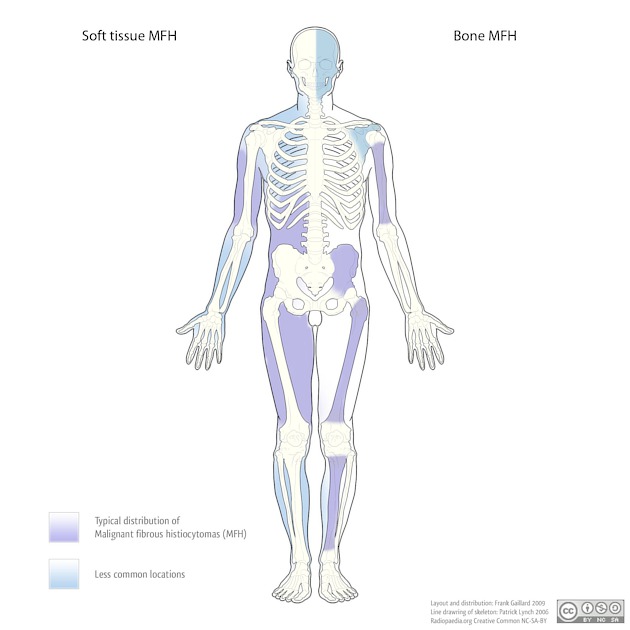
They are usually confined to the soft tissues but occasionally may arise in or from bone (1-5%) . Although UPS can occur almost anywhere in the body, they have a predilection for extremities: lower and upper extremities corresponding to ~50% and ~20% of the cases, respectively . Retroperitoneal UPS represent about 16% of the cases and, those involving the peritoneal cavity, about 5-10% . Involvement of the abdominal viscera is described as extremely rare.
Macroscopic appearance
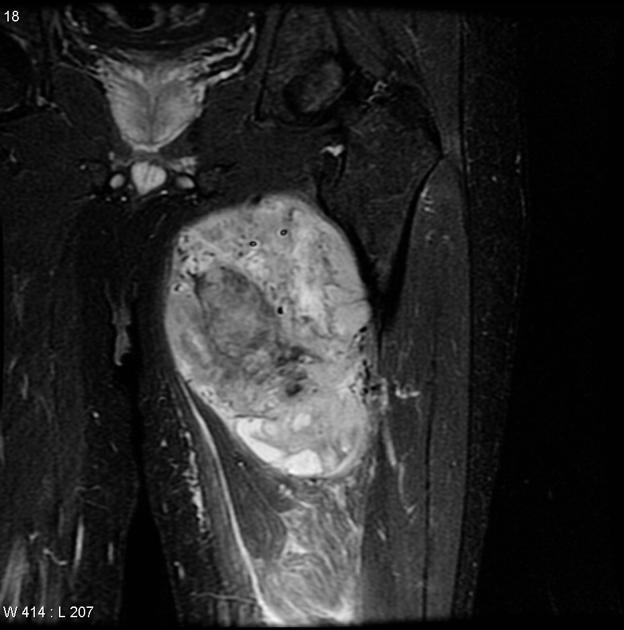
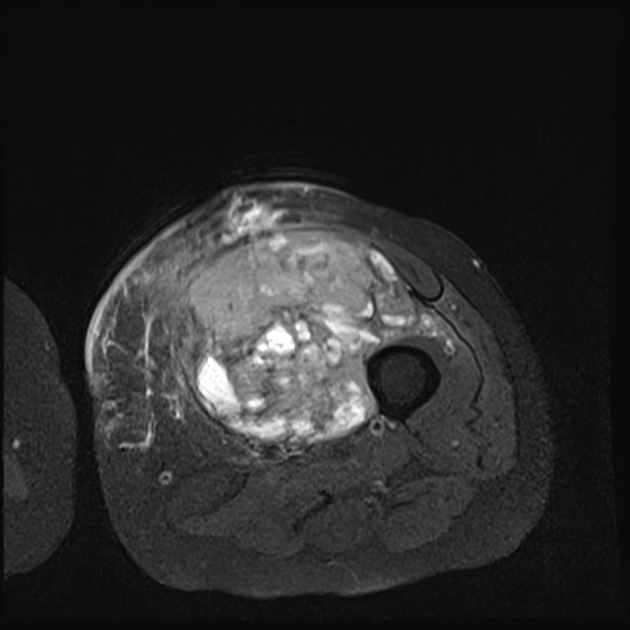
Macroscopically, these tumors are typically large (5-20 cm) well circumscribed but unencapsulated with a grey firm heterogeneous cut surface sometimes with areas of necrosis .
Histology
Microscopically they are heterogeneous fibroblastic tumors made up of poorly differentiated fibroblasts, myofibroblasts, histiocyte-like cells with significant cellular pleomorphism, storiform architecture and also demonstrate bizarre multi-nucleated giant cells. They are sometimes difficult to distinguish from other high-grade sarcomas. A number of histological subtypes have been described including :
- storiform-pleomorphic: most common 50-60%
- myxoid: 25%, myxofibrosarcoma
- inflammatory: 5-10%
- giant cell: 5-10%
- angiomatoid
- relatively non-aggressive
- metastases uncommon
- usually occurs in young adults/adolescents
Radiographic features
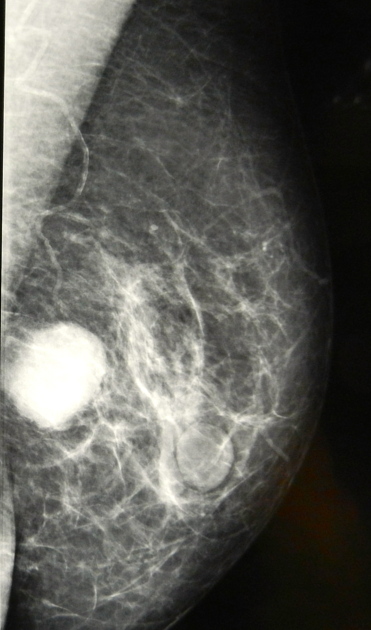
Plain radiograph
Plain radiographs will demonstrate a soft tissue mass and if arising from bone, then appear as an aggressive destructive bony lesion. In some cases, curvilinear or punctate regions of calcification may be demonstrated.
CT
The density of UPS is typically similar to adjacent muscle, with heterogeneous lower density areas if hemorrhage, necrosis or myxoid material is abundant. The soft tissue component enhances. In up to 15-20% of cases, some mineralization is present .
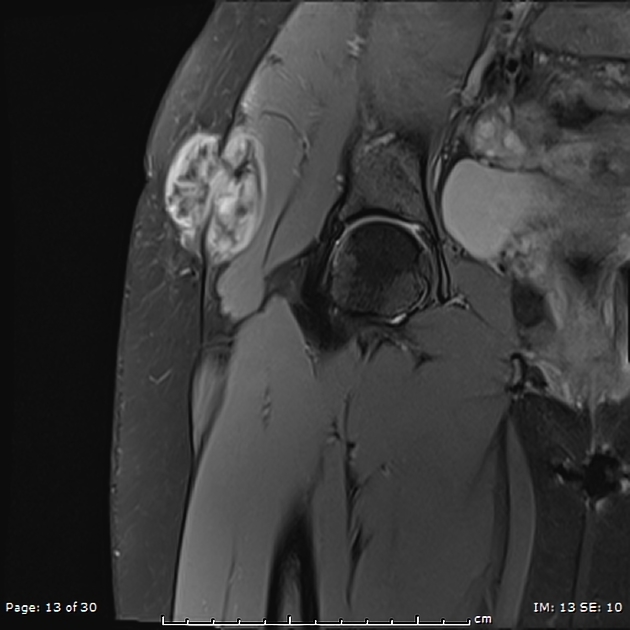
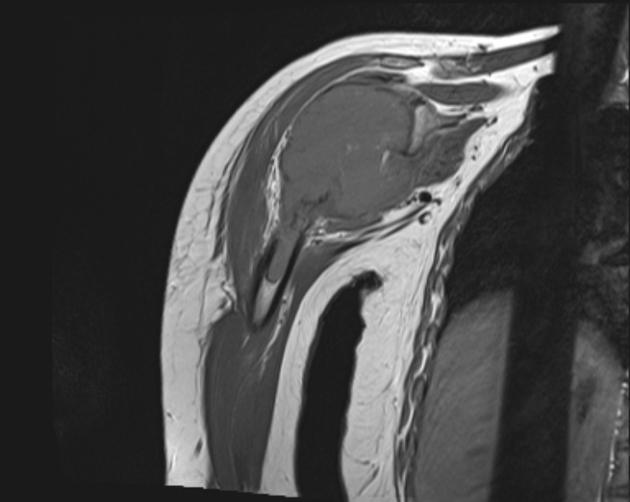
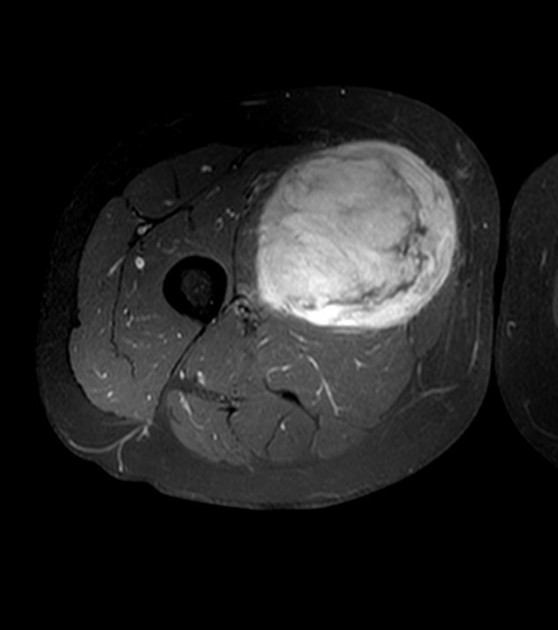
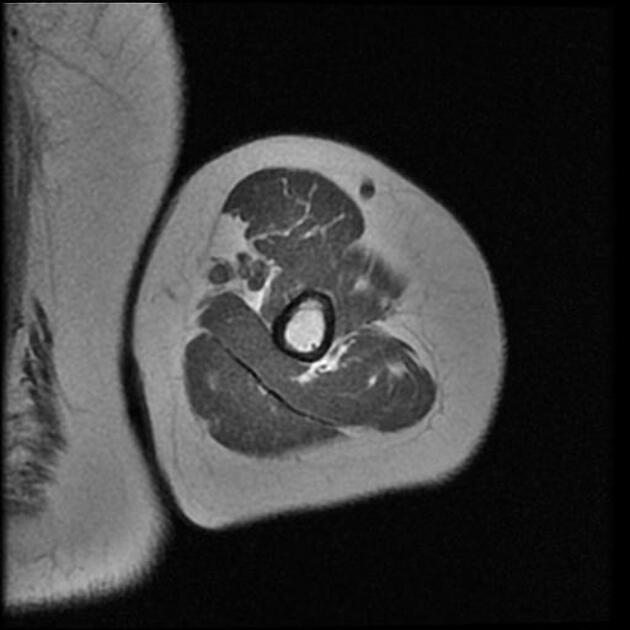
MRI
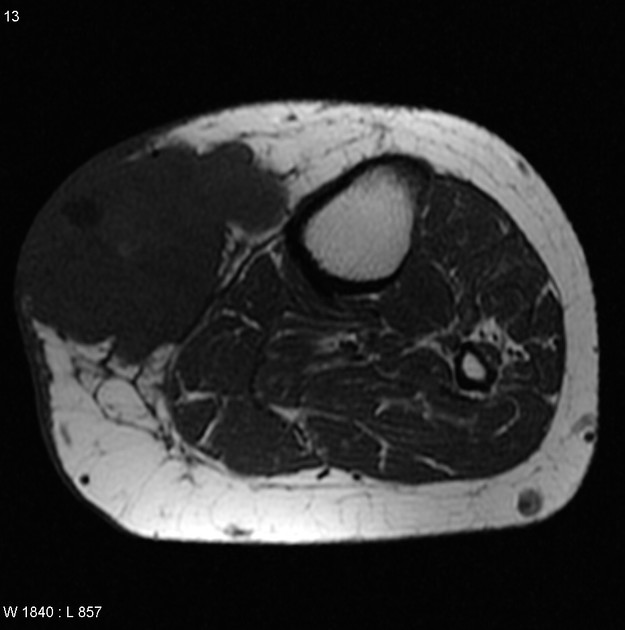
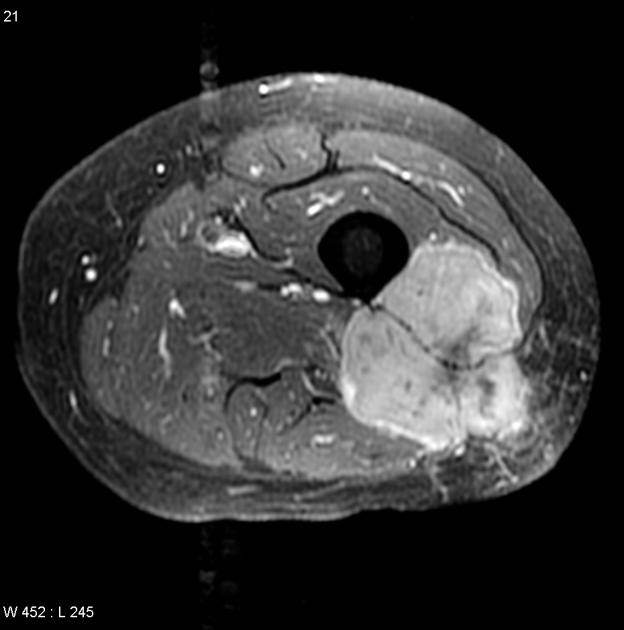
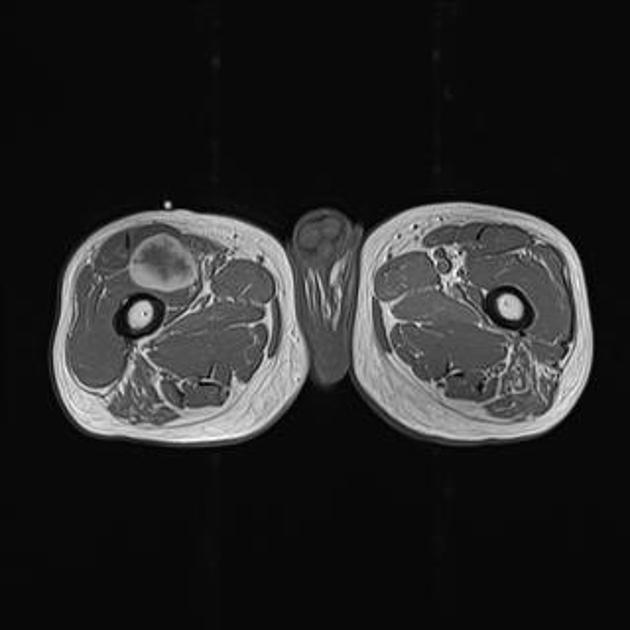
MRI is the modality of choice for assessing soft tissue sarcomas, as it is best able to locally stage a tumor.
These tumors are typically relatively well-circumscribed, located within or adjacent to muscle, exerting a positive mass effect on surrounding structures due to their (usual) large size at presentation.
- T1
- intermediate (to low) signal intensity, similar to adjacent muscle
- heterogeneity if hemorrhage, calcification, necrosis, myxoid material present
- T1 + C
- prominent enhancement of solid components
- T2
- intermediate to high signal intensity
- heterogeneity if hemorrhage, calcification, necrosis, myxoid material present
Treatment and prognosis
Most UPS are of high grade (3 and 4) and are aggressive in their biological behavior. They frequently metastasize (30-50% at diagnosis ) and locally recur despite aggressive treatment. The overall 5-year survival is between 25-70% .
Prognostic factors include:
- tumor size: smaller being better
- location
- superficial is better
- distal is better
- histological grade
- histological subtype: the myxoid subtype has a better prognosis as compared to the storiform-pleomorphic subtype .
Examples
A tumor located superficially in the subcutaneous tissues of the distal extremity, and measuring less than 5 cm, has a 5-year survival of 80%, whereas a proximal large (>5 cm) and deep tumor has a 5-year survival of 55% .
Treatment usually consists of aggressive en bloc resection with a wide margin. Supplementary neoadjuvant chemotherapy and radiotherapy is especially useful in reducing the local recurrence rate . Limb-sparing surgery is usually possible .
Differential diagnosis
General imaging differential considerations include:
- other sarcomas and soft tissue tumors
- synovial sarcoma
- aggressive fibromatosis
- benign fibrous tumors
- soft tissue metastases
- myositis ossificans
See also
Siehe auch:
- Myositis ossificans
- Synovialsarkom
- WHO Klassifikation der Weichteiltumoren
- Desmoid-Tumor - aggressive Fibromatose
- pleomorphes undifferenziertes Sarkom des Retroperitoneums
- Pleomorphes Undifferenziertes Sarkom bei Kindern
und weiter:
- Codman-Dreieck
- myxofibrosarcoma
- Liposarkom
- moth-eaten appearance in bone
- WHO-Klassifikation der Tumoren des zentralen Nervensystems
- Dermatofibrosarcoma protuberans
- Tumoren der Thoraxwand
- oberflächliche Weichteilläsionen der Extremitäten
- cardiac curriculum
- dedifferentiated chondrosarcoma
- Weichteilsarkom
- Weichteiltumoren der Extremitäten
- retroperitoneale Tumoren
- benignes fibröses Histiozytom des Knochens
- extraskeletal musculoskeletal tumors by compartment
- bone lesions with sequestrum
- bony sequestrum (mnemonic)
- clavicle abnormalities (paediatric)
- permeative process in bone (mnemonic)
- fibrous lesions
- extra skeletal musculoskeletal lesions by compartment
- primäre maligne Neoplasien des Herzens
- maligne Tumoren des Herzen
- disorganised periosteal reaction
- pleomorphic rhabdomyosarcoma
- extra skeletal chondrosarcoma
- paediatric clavicle abnormalities
- paratesticular tumours
- Knochentumoren
- radiologisches muskuloskelettales Curriculum
- Dermatofibrom
- Tumoren der Wirbelsäule
- distribution of MFH
- malignant fibrous histiocytoma in the gluteal zone
- recurrence of a malignant fibro-histiocytoma in the masticator space with perineural spread

 Assoziationen und Differentialdiagnosen zu Pleomorphes Undifferenziertes Sarkom:
Assoziationen und Differentialdiagnosen zu Pleomorphes Undifferenziertes Sarkom: