reversibles zerebrales Vasokonstriktionssyndrom


 nicht verwechseln mit: posteriores reversibles Enzephalopathiesyndrom
nicht verwechseln mit: posteriores reversibles EnzephalopathiesyndromReversible cerebral vasoconstriction syndrome (RCVS) is a group of conditions with a common clinical and radiologic presentation. It is characterized by thunderclap headache and reversible vasoconstriction of the cerebral arteries.
Terminology
Numerous and varied terms have been used to describe RCVS, sometimes entirely synonymously and at other times one or other subset. These terms include :
- acute benign cerebral angiopathy
- benign angiopathy of the CNS
- CNS pseudovasculitis
- Call-Fleming syndrome
- cerebral vasculopathy
- drug-induced cerebral arteritis
- isolated benign cerebral vasculitis
- migrainous vasospasm or migraine angiitis
- postpartum cerebral angiopathy
- primary thunderclap headache
- sexual headache
- thunderclap headache associated vasospasm
- vasospasm in fatal migrainous infarction
Importantly RCVS should not be confused with posterior reversible encephalopathy syndrome (PRES). Although there is overlap both in the presumed underlying mechanisms and predisposing factors they are considered separate syndromes. Confusingly, an association of PRES with RCVS has been described particularly in the setting of clinical settings that both conditions have in common (e.g. eclampsia and septic shock syndrome) .
Another important distinction is with vasospasm related to subarachnoid hemorrhage. In both instances subarachnoid blood and vasospasm may be seen, however, in RCVS subarachnoid hemorrhage is believed to be a secondary phenomenon rather than the inciting event .
Epidemiology
RCVS affects women more commonly than men (F:M 2.4:1) and usually presents between 20-50 years of age (mean 42), although it has also been described in children and adolescents . The mean age of presentation in men is a decade younger than the mean age of presentation for women.
Clinical presentation
Thunderclap headache is the usual primary symptom, often occipital but also potentially diffuse. They are usually fairly short in duration (a few hours) and usually, headaches will periodically recur over days or weeks.
Headaches may be associated with photophobia, nausea and vomiting. Focal neurological deficits can occur, secondary to ischemia or convexity subarachnoid hemorrhage. CSF studies are normal or near normal.
In 2016, a study proposed a set of criteria to diagnose RCVS and to distinguish it from primary angiitis of the central nervous system (PACNS) with a specificity of 98-100% and a similarly high PPV :
- recurrent thunderclap headaches or;
- single thunderclap headache with either normal neuroimaging study or watershed infarct/vasogenic edema or;
- no thunderclap headache but abnormal angiographic findings with a normal neuroimaging study
- this basically rules out PACNS as neuroimaging is always abnormal
Criteria have also been proposed by the International Headache Society.
Associated/predisposing conditions
- pregnancy and puerperium
- early puerperium / late pregnancy
- eclampsia / pre-eclampsia / delayed postpartum eclampsia
- exposure to drugs and blood products
- phenylpropanolamine
- pseudoephedrine
- ergotamine
- tartrate
- methysergide
- bromocriptine
- lisuride
- SSRI
- sumatriptan
- isometheptene
- 'recreational drugs'
- cocaine
- ecstasy
- marijuana
- amphetamines
- tacrolimus
- cyclophosphamide
- erythropoietin
- IV Ig
- red blood cell transfusion
- miscellaneous
- migraine (20-40%)
- at least in part explained by the known role of migraine medication as a trigger for the syndrome
- hypercalcemia
- porphyria
- pheochromocytoma
- bronchial carcinoid
- unruptured cerebral aneurysm
- head trauma/neurosurgical procedures
- spinal subdural hematoma
- post carotid endarterectomy
- migraine (20-40%)
- idiopathic
Radiographic features
Neuroimaging is often reported as normal at the onset of symptoms but this varies from study to study (21-55%) .
The findings on imaging consist of either direct visualization of the vascular narrowings and/or complication(s) related to vascular narrowings such as:
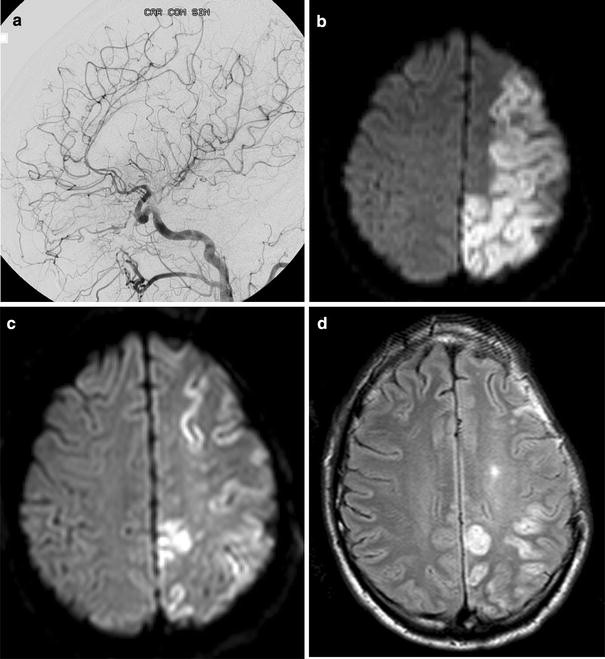
- convexity non-aneurysmal subarachnoid hemorrhage (22-34%)
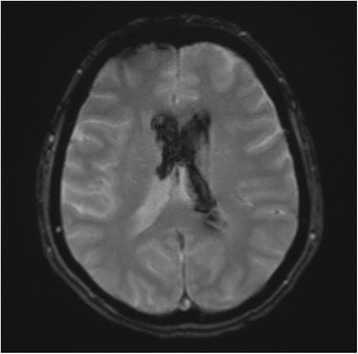
- lobar hemorrhage (6-20%)
- watershed infarct (29%)
- vasogenic edema (38%)
Ultrasound
Transcranial Doppler may show increased arterial velocities suggesting vasospasm and decreased luminal caliber of ICA, MCA and ACA . Bedside ultrasound has been used for the follow-up of vasospasm .
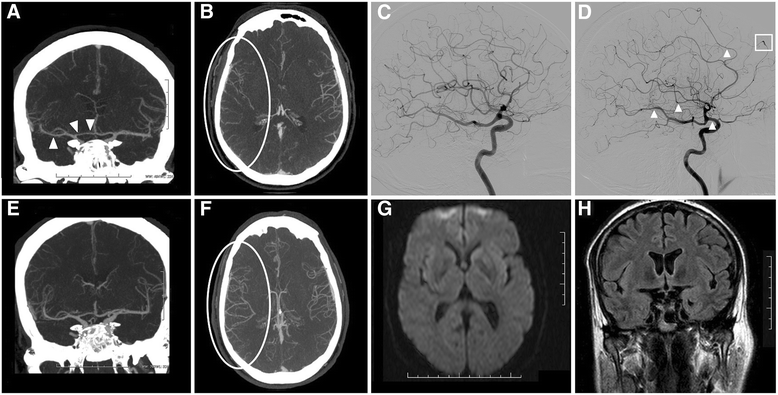
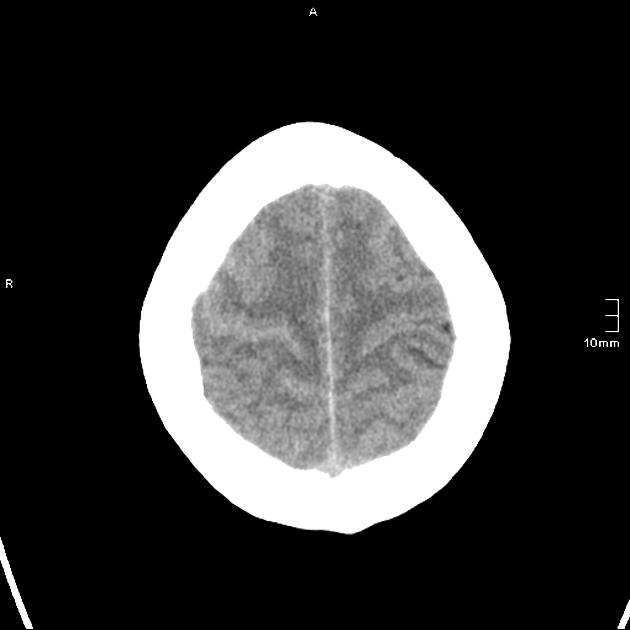
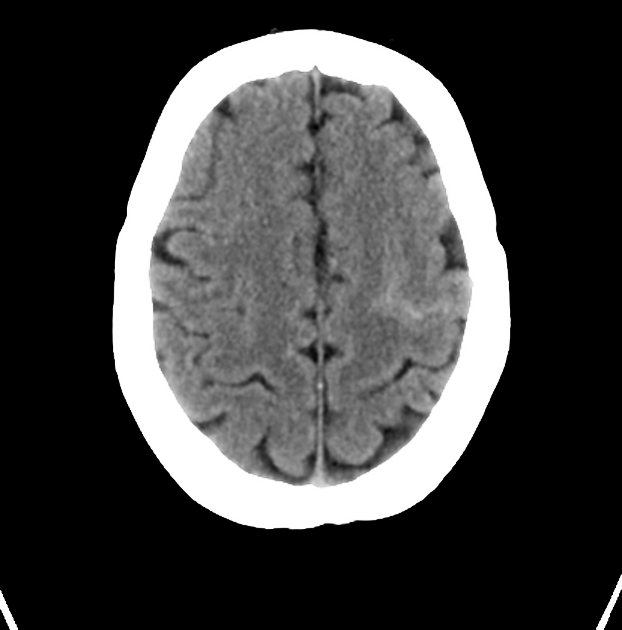
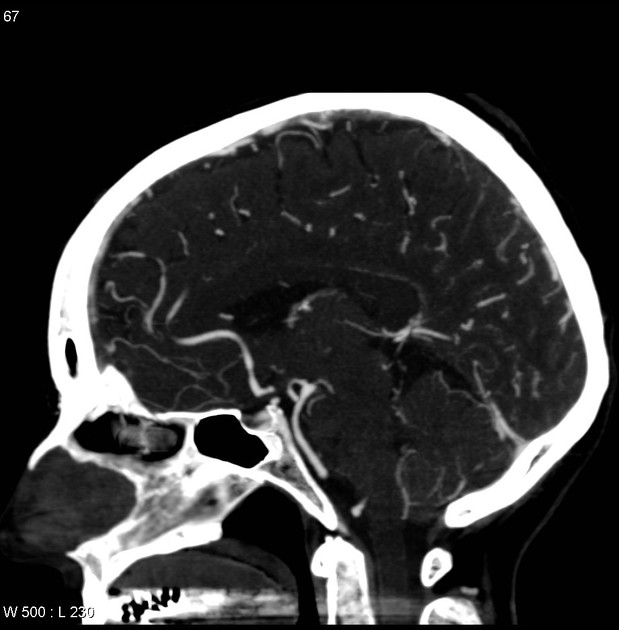
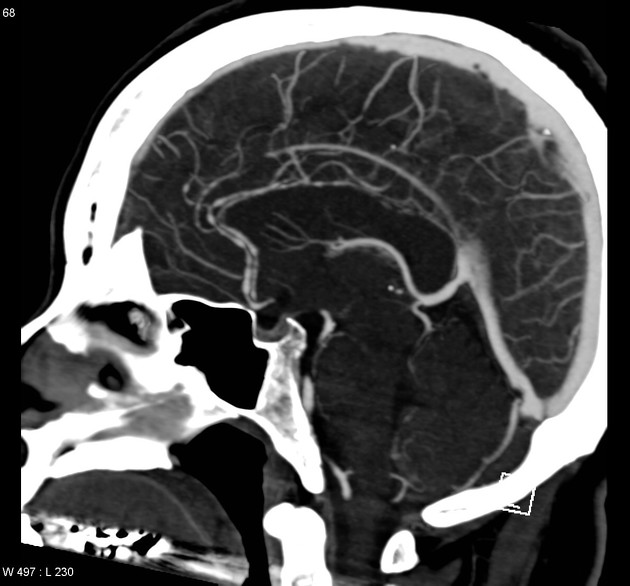
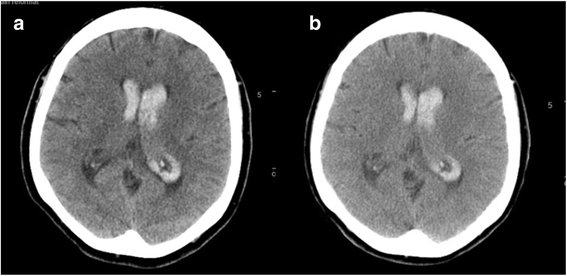
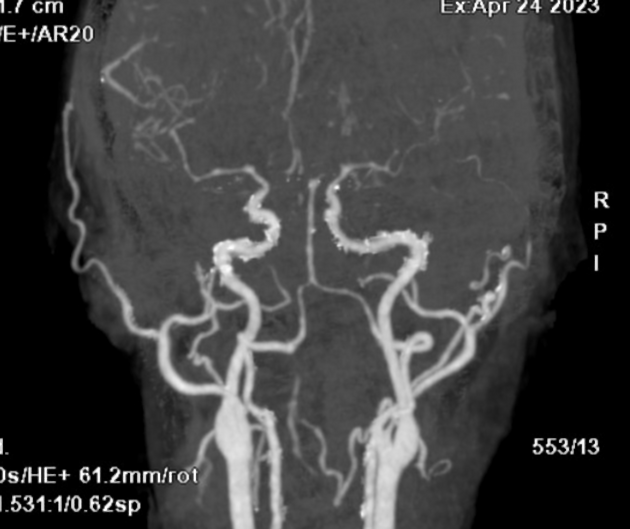
CT
CT-scan and CTA are useful to rule out aneurysmal subarachnoid hemorrhage. As previously noted, CT-scan can be entirely normal with RCVS. The following can be seen:
- convexity subarachnoid hemorrhage
- watershed infarct
- lobar hemorrhage
- vascular narrowings on CTA
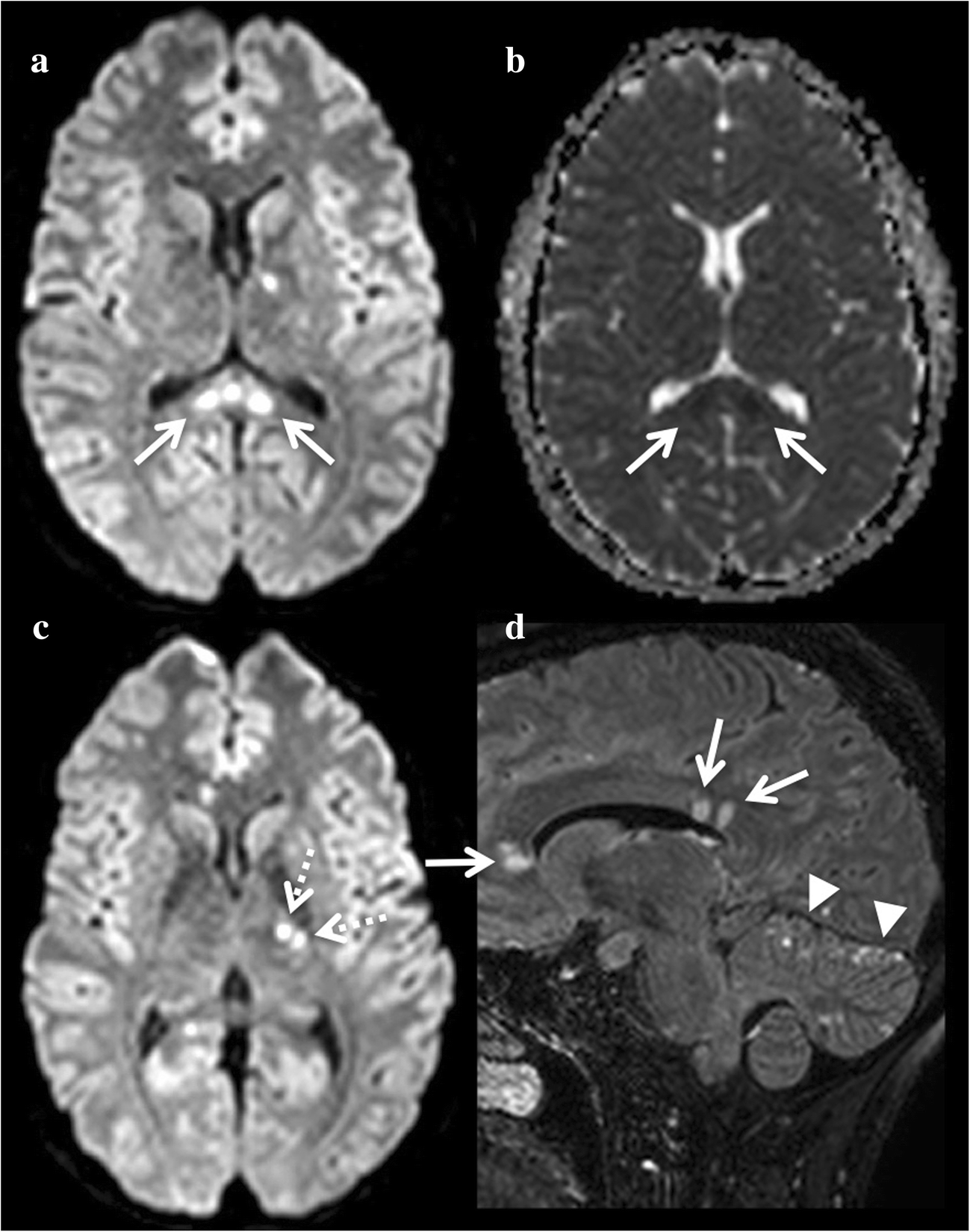
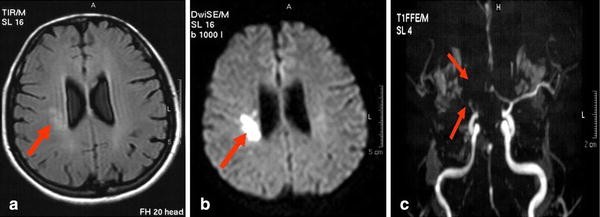
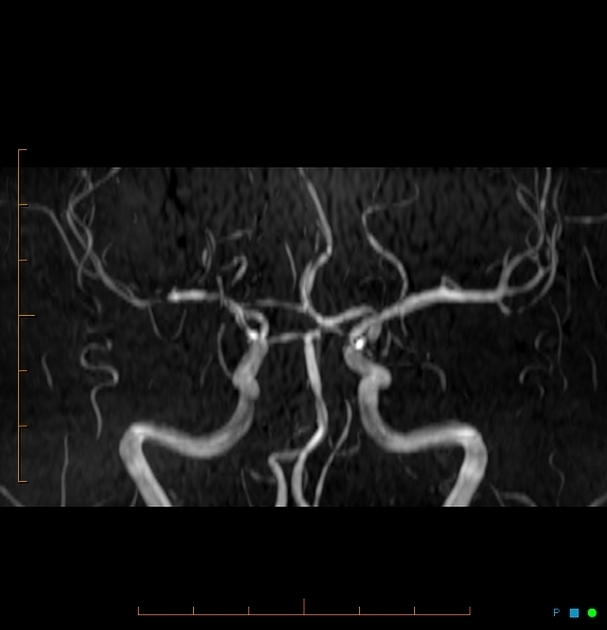
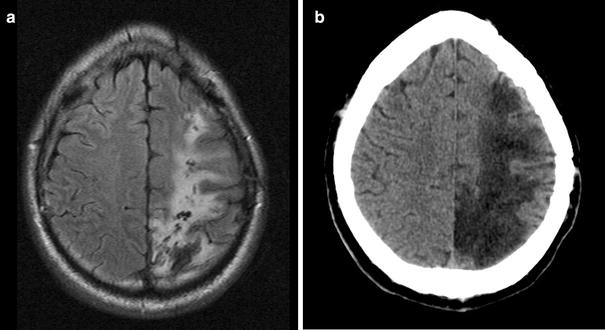
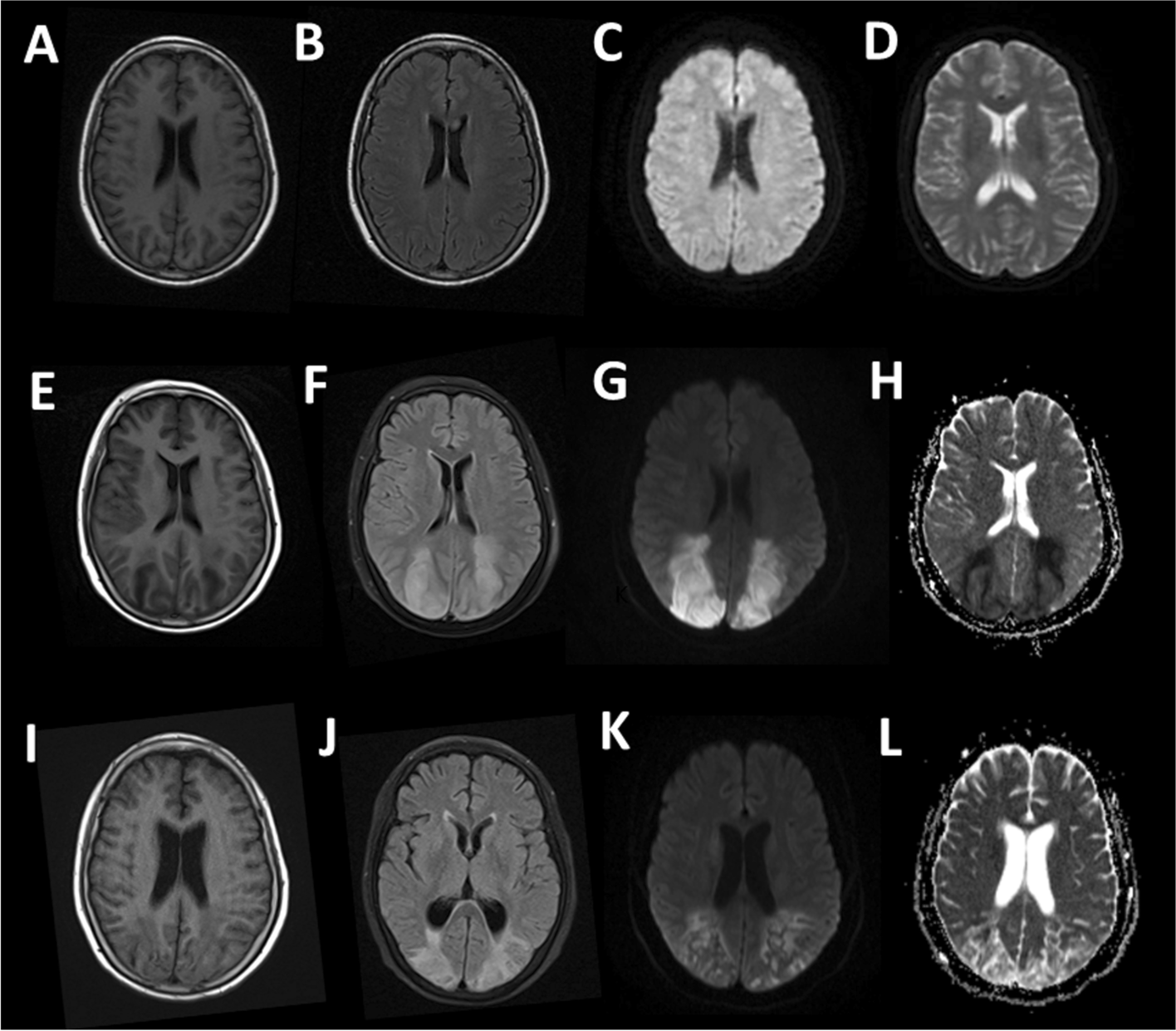
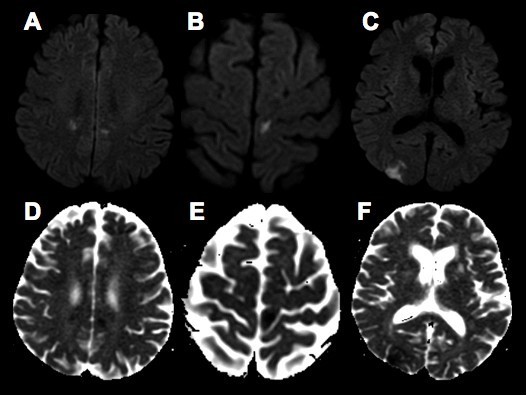
MRI
Cortical edema and/or vascular FLAIR hyperintensities may precede vasoconstriction on MRI.
- FLAIR:
- sulcal hyperintensities may reflect convexity subarachnoid hemorrhage or vascular hyperintensities (an early sign)
- cortical hyperintensities related to cortical edema (an early sign)
- vasogenic edema related to vasoconstriction or cytotoxic
- FLAIR C+:
- useful as it does not show normal cortical vessels and meninges (versus T1 C+), and may reflect blood-brain barrier breakdown
- variable patterns of sulcal enhancement have been described
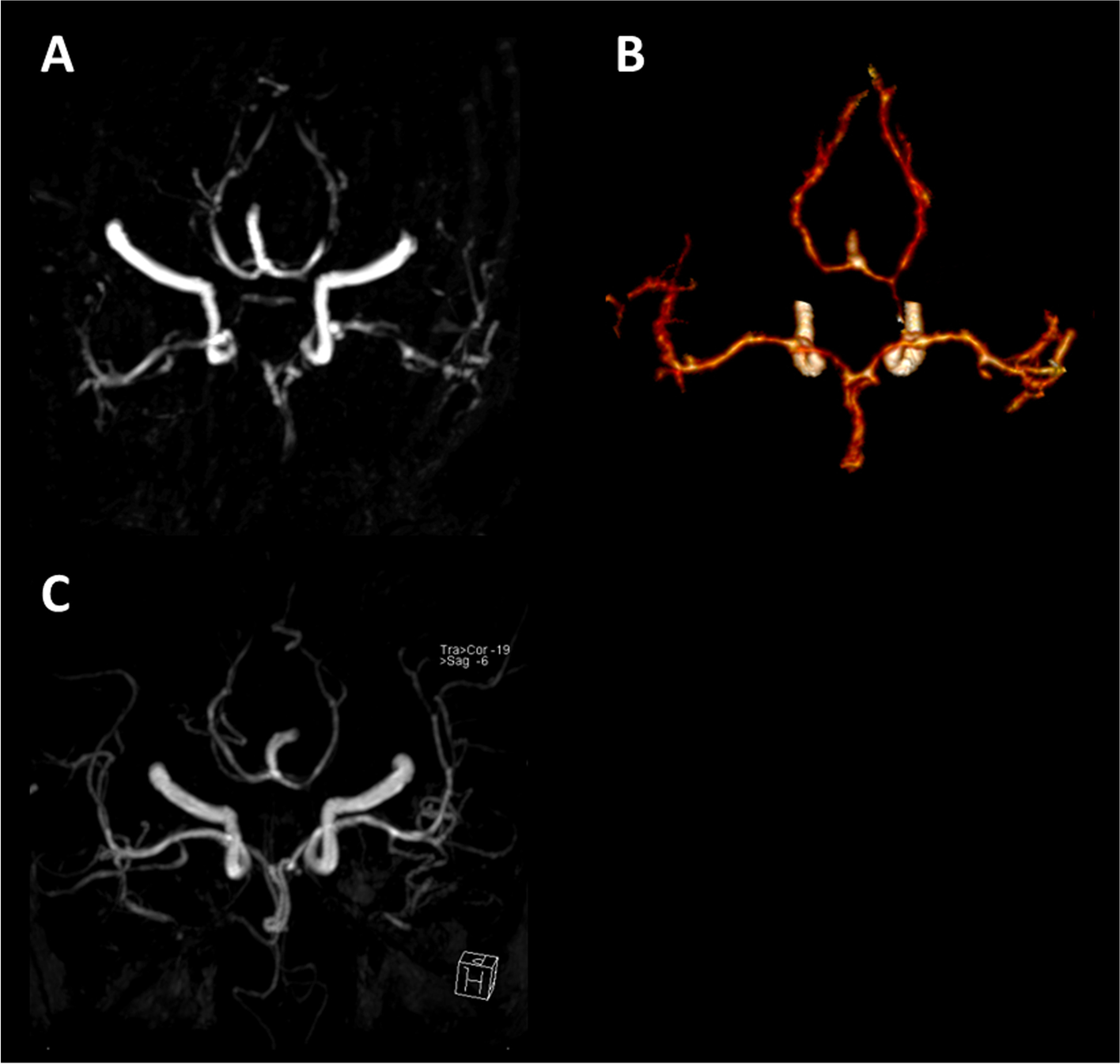
- MRA: vascular narrowings can be seen (see DSA)
- DWI: watershed infarcts can be seen
Vessel wall MRI (VW-MRI) may be a useful adjunct to conventional MRI, allowing differentiation between RCVS, where there is no or mild contrast enhancement of the affected arterial wall, and other causes of vascular narrowing such as vasculitis, where there is intense contrast enhancement of the affected arterial wall, or intracranial atherosclerotic plaques, which focally demonstrate contrast enhancement .
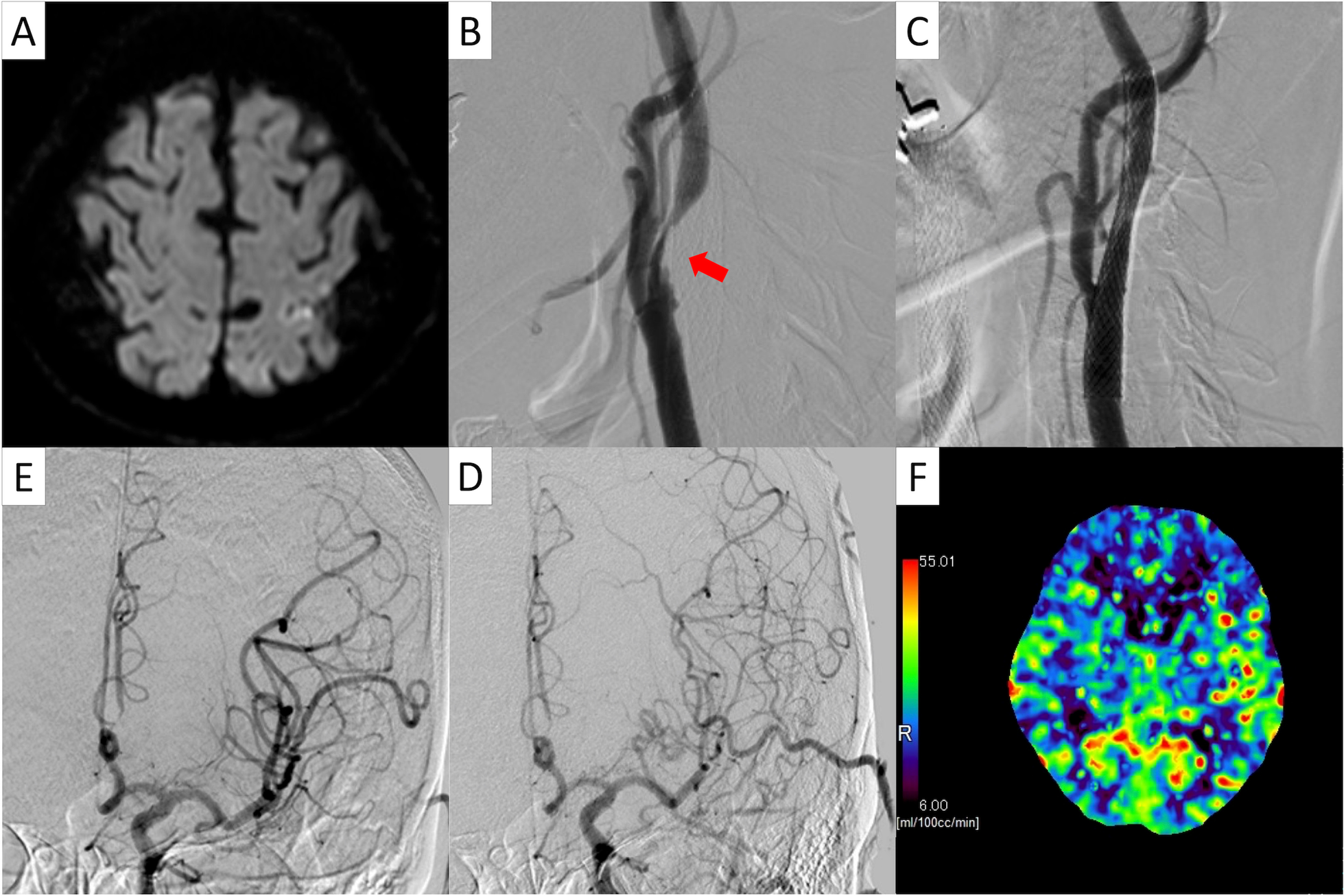
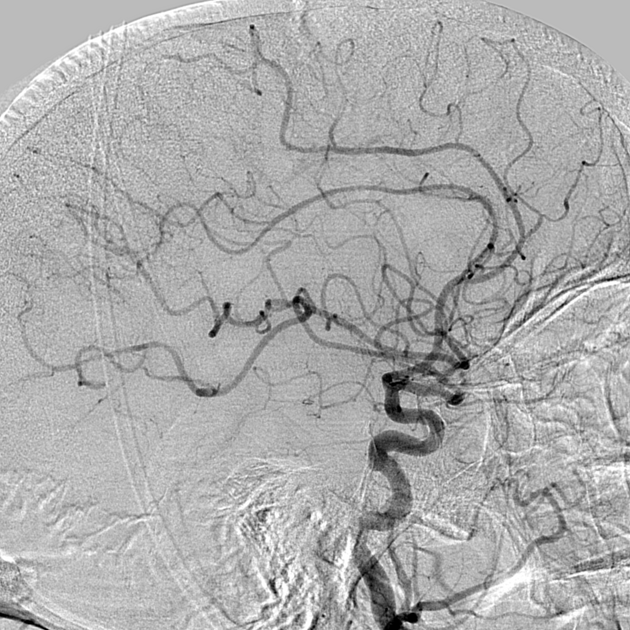
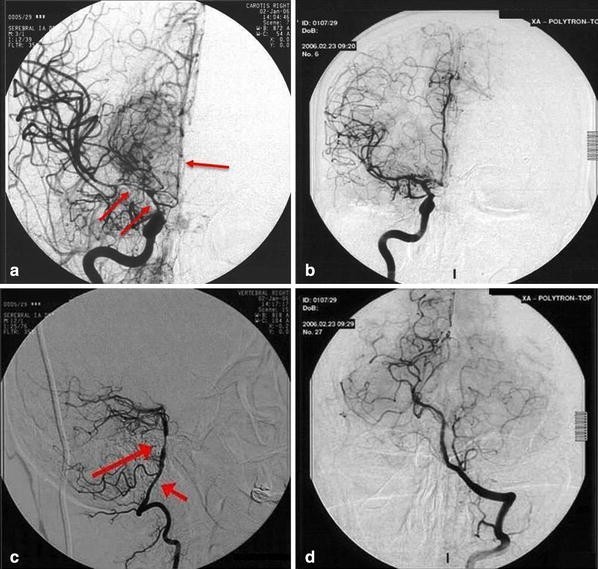
DSA - angiography
Smooth, tapered narrowings involving large to medium-sized arteries followed by abnormally dilated segments of second-order and third-order branches is the most characteristic finding . This dilatation gives the typical beaded or sausage-shaped appearance of cerebral arteries. Normalization of the angiographic findings is usually seen within 8-12 weeks .
Vasoconstriction following subarachnoid hemorrhage involves longer segments of more proximal branches without alternating areas of narrowing . It is worth noting that intracranial atherosclerosis causing vascular narrowings is seen in 7.5-30% of the asymptomatic population thus potentially complexifying evaluation on DSA .
Treatment and prognosis
Spontaneous resolution usually occurs, with improvement in angiographic findings within three months. The natural history of the condition has not however been well characterized. Complete long-term resolution of the symptoms with no neurological deficit is the most common outcome in up to 90% of patients .
Although no randomized controlled trials are available, treatment with calcium channel blockers seems to be efficacious and are thought to be a reasonable first-line therapy. Short course glucocorticoid therapy has also been advocated.
History and etymology
It was first described by Calabrese et al. in 1993 and named “benign angiopathy of the central nervous system”. Afterwards, in 1998, Call and Flemming described a series of patients with severe headaches and reversible cerebral segmental vasoconstriction (see Call-Flemming syndrome) . The term RCVS was coined later in 2007 by Calebrese .
Differential diagnosis
The differential on clinical presentation is essentially that of a thunderclap headache, with the main concern being aneurysmal subarachnoid hemorrhage.
When vascular imaging has been obtained, the differential narrows to conditions that can cause intracranial arterial beading, namely:
- subarachnoid hemorrhage with intracranial vasospasm
- PACNS
- arterial dissection
- partially or untreated treated fungal or bacterial meningitis
Practical points
No validated radiological criteria have been defined for diagnosis confirmation. However, the following guidelines are reasonable when applied to the clinical context:
- neurovascular imaging demonstrates multifocal narrowings in the circle of Willis and its branches
- there is a suggestion of centripetal propagation of the narrowings when comparing initial neurovascular imaging at the onset of thunderclap headache with postremission neurovascular imaging
- if subarachnoid hemorrhage is present, it is usually mild and only involves the cerebral convexity
- validation of the diagnosis rests on eventual resolution of neurovascular findings within 8-12 weeks
Siehe auch:
- Subarachnoidalblutung
- Dissektion
- Susac syndrome
- thunderclap headache
- posteriores reversibles Enzephalopathiesyndrom
- zerebraler Vasospasmus
und weiter:
 Assoziationen und Differentialdiagnosen zu reversibles zerebrales Vasokonstriktionssyndrom:
Assoziationen und Differentialdiagnosen zu reversibles zerebrales Vasokonstriktionssyndrom: