stomach
The stomach is a muscular organ that lies between the esophagus and duodenum in the upper abdomen. It lies on the left side of the abdominal cavity caudal to the diaphragm at the level of T10.
Gross anatomy
The stomach ("normal" empty volume 45 mL) is divided into distinct regions:
- cardia: the area that receives the esophagus (gastro-esophageal junction)
- fundus: formed by the upper curvature; portion of stomach above GEJ level
- body (corpus): the main central region of the organ; central two-thirds portion from the cardia to the incisura angularis
- pylorus (antrum): the lower section of the stomach that facilitates emptying into the small intestine, located on the right of the midline at the level of L1.
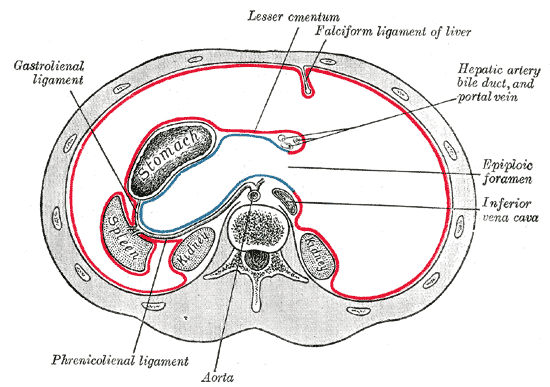
The lesser curvature forms the shorter concave border and the greater curvature forms the longer convex border of the stomach. The lesser omentum attaches the lesser curvature to the liver, while the greater omentum attaches to the greater curvature of the stomach .
There are two smooth muscle sphincters, esophageal and pyloric, that dictate entry into and exit from the stomach. These are under the control of several mechanisms including stimulant (parasympathetic) and inhibitory (orthosympathetic) control from the anterior gastric, posterior, superior and inferior celiac and myenteric nerve plexuses.
The inner mucosal surface has many rugal folds that act to increase the surface area of the stomach lining and increase its efficiency.
Specific sites
- incisura angularis: small anatomical notch on the stomach located on the lesser curvature of the stomach near the pyloric end, which marks the junction between the body and the antrum
- fornix gastricus: refers to the arch-shaped superior margin of the fundus of the stomach
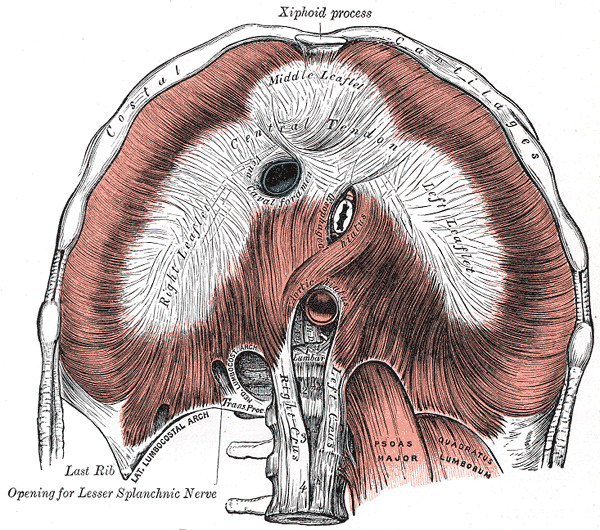
Relations
- anteriorly: left lobe of liver, anterior abdominal wall, left hemidiaphragm
- posteriorly: anterior wall of lesser sac, stomach bed
- medially: abdominal aorta, celiac trunk, celiac lymph nodes
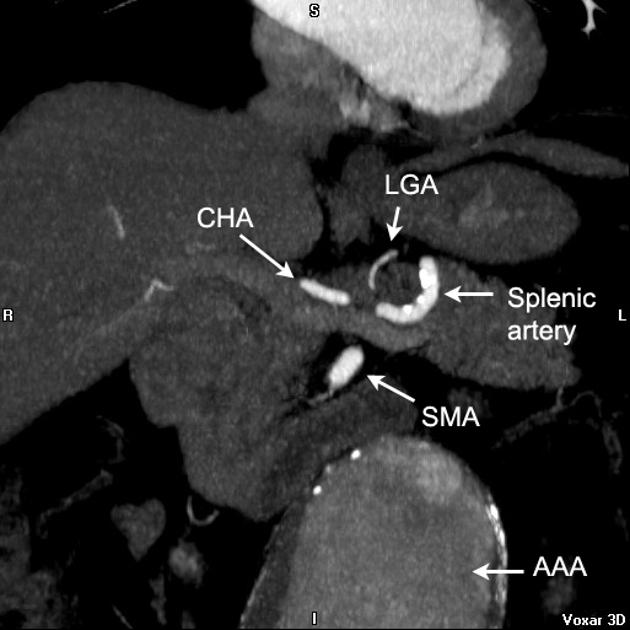
Arterial supply
- lesser curvature: right gastric artery (inferiorly) and left gastric artery (superiorly)
- cardia: left gastric artery
- greater curvature: right gastroepiploic artery (inferiorly) and left gastroepiploic artery and short gastric arteries (superiorly)
- fundus of the stomach: short gastric arteries
Venous drainage
- left and right gastric veins drain to portal vein
- short gastric vein and left gastroepiploic vein drain to splenic vein
- right gastroepiploic vein drains to superior mesenteric vein
Lymphatic drainage
Routes of flow of lymph from perigastric nodes to para-aortic lymph nodes include :
- directly to left paracardial lymph nodes
- along lymph nodes accompanying the splenic artery
- along lymph nodes accompanying the celiac artery
- along lymph nodes accompanying the superior mesenteric artery
- along lymph nodes on the posterior surface of the pancreatic head and nodes accompanying the common hepatic artery
Nomura et al suggested that the most likely route for para-aortic lymph node metastases was from the left gastric artery nodes passing by the celiac artery .
Histology
Akin to other areas of the gastrointestinal (GI) tract, the stomach walls are composed of the following layers:
- mucosa: internal layer of epithelium, the lamina propria (loose connective tissue and gastric glandular tissue) and the muscularis mucosae
- submucosa: a fibrous layer of connective tissue under the mucosa
- muscularis externa: this is the muscular layer of the stomach wall and is comprised of three layers (inner oblique, middle circular and outer longitudinal) unlike other GI organs which only have two layers
- serosa: the outermost layer of the stomach wall consisting of connective tissue which is continuous with the peritoneum
Cell types
The stomach wall contains several different types of glandular tissue. The cardia, fundus and pylorus all have different types of glands and are composed of a variety of different cells:
- mucous cells: secrete a mucus gel layer and are found throughout the stomach
- parietal (oxyntic) cells: secrete gastric acid and intrinsic factor throughout the stomach
- chief (zymogenic) cells: secrete pepsinogen and rennin in the fundus and body
- enteroendocrine (APUD) cells: secrete a variety of products and are found throughout the stomach
Physiology
Control of the stomach relates to the autonomic nervous system and various digestive system hormones:
- gastrin: causes an increase in the secretion of hydrochloric acid (HCl), pepsinogen and intrinsic factor from parietal cells in the stomach; it also causes increased motility in the stomach; released by G-cells in the stomach to distension of the antrum, and digestive products; inhibited by a pH normally <4 (acidic), as well as the hormone somatostatin
- cholecystokinin (CCK): greatest effect on the gall bladder, but it also decreases gastric emptying and increases release of pancreatic juice which is alkaline and neutralizes the chyme
- secretin: has most effects on the pancreas, but will also diminish acid secretion in the stomach
- gastric inhibitory peptide (GIP): decreases both gastric acid and motility
- enteroglucagon: decreases both gastric acid and motility
- glycogen: produced in the brain and stomach, affects the liver and level of glucose in the stomach
Radiographic features
Plain radiograph
The stomach is not usually well visualized on the plain film although a gastric bubble (gas outlining the fundus of the stomach) is often visible on an erect chest or abdominal x-ray.
CT
When well distended, the normal gastric wall will have a thickness of 5 to 7mm in the antrum and 2 to 3mm in the body .
Ultrasound
Analogous to the abovementioned histological architecture, the gastric walls will consist of five concentric layers of alternating echogenicity when viewed with an appropriately high frequency transducer, characteristic of the sonographic gut signature .
Sonographic localization of the stomach is typically performed with epigastric transducer placement with the patient in a supine or right lateral decubitus position. The gastric antrum is commonly visualized just to the right of anatomic midline using the following sonographic landmarks;
- left lobe of the liver
- lies cephalad and anterior to the gastric antrum
- pancreatic body
- lies posteriorly to the gastric antrum
- identified lying anteriorly to the abdominal aorta and superior mesenteric artery
- parallels the course of the splenic vein, which demarcates its posterior extent
- transverse colon
- inferior to the gastric antrum
Visualization of the gastric body is often possible by sweeping leftward of the gastric antrum. Visualization of the gastric fundus may require using the spleen as a sonographic window, using a left intercostal probe position. The sonographic appearance of the stomach, most notably the gastric antrum, may differ based on the patient's prandial status as follows;
- fasting patient
- gastric antrum may appear as a flattened ovoid with absent to minimally appreciable luminal contents
- targetoid or "bulls eye" appearance
- may also appear round, with homogenous anechoic fluid filling the lumen
- gastric antrum may appear as a flattened ovoid with absent to minimally appreciable luminal contents
- post-prandial patient
- viscous fluid ingestion results in luminal contents appearing uniformly hyperechoic
- recent solid food ingestion results in a heterogenous appearance of luminal contents, with posterior acoustic shadowing
- may be indicative of higher aspiration risk for patients under general anesthesia
Siehe auch:
und weiter:
 Assoziationen und Differentialdiagnosen zu Magen:
Assoziationen und Differentialdiagnosen zu Magen: