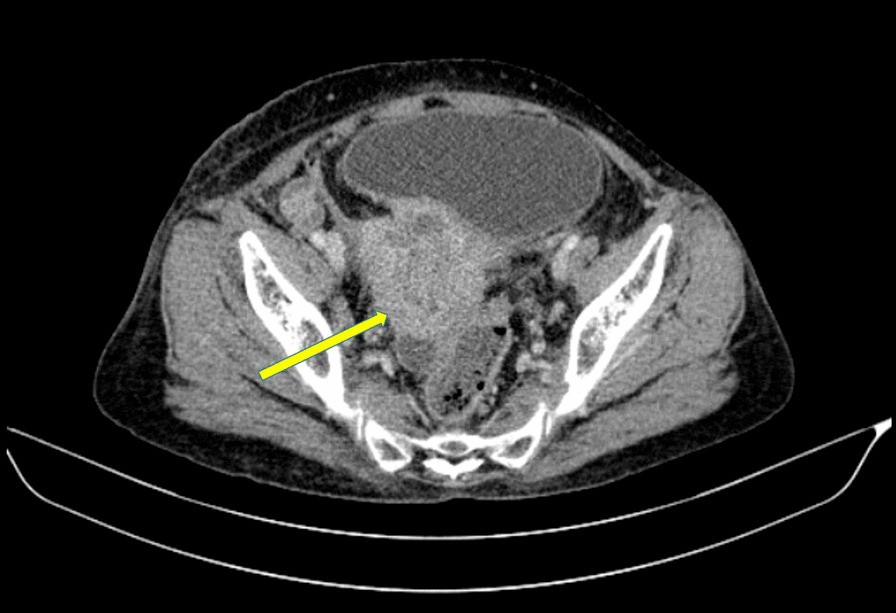
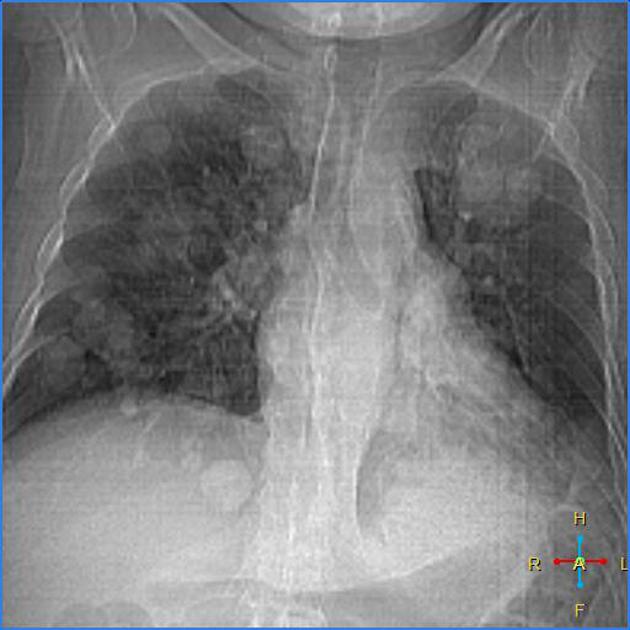
Lungenmetastasen bei Zervixkarzinom



Lungenmetastasen bei Zervixkarzinom
Lungenmetastasen Radiopaedia • CC-by-nc-sa 3.0 • de
Pulmonary metastases are common and the result of metastatic spread from a variety of primary tumors via blood or lymphatics.
This article describes haematogenous pulmonary metastases with lymphangitis carcinomatosis discussed separately.
Epidemiology
The epidemiology will match that of the underlying malignancy (see below), but as malignancies increase in incidence with increasing age, so does the presence of pulmonary metastases.
Clinical presentation
Pulmonary metastases are usually asymptomatic, with constitutional symptoms relating to disseminated metastatic disease and those attributable to the primary tumor dominating . Hemoptysis and pneumothorax are sometimes the presenting symptoms.
Pathology
Tumor cells reach the lungs via the pulmonary circulation, where they lodge in small distal vessels.
The most common primaries to result in pulmonary metastases in adults include :
- breast carcinoma
- colorectal carcinoma
- renal cell carcinoma
- uterine leiomyosarcoma
- head and neck squamous cell carcinoma
In the pediatric population, the most common primaries for pulmonary metastases are:
Alternatively, primaries which most frequently metastasize to lungs (although are much less common) include :
- choriocarcinoma
- Ewing sarcoma
- malignant melanoma
- osteosarcoma
- testicular tumors
- thyroid carcinoma
- pancreatic cancer
Primaries that metastasize as endobronchial deposits can include:
Radiographic features
Pulmonary metastases typically appear as peripheral, rounded nodules of variable size, scattered throughout both lungs . Atypical features include consolidation, cavitation, calcification, hemorrhage, and secondary pneumothorax.
Plain radiograph
Plain films are insensitive, although frequently able to make the diagnosis, as often pulmonary metastases are large and numerous.
CT
CT is excellent at visualizing pulmonary nodules. Typically, metastases appear of soft tissue attenuation, well circumscribed, rounded lesions, more often in the periphery of the lung. They are usually of variable size, a feature which is of some use in distinguishing them from a granuloma .
A prominent pulmonary vessel has frequently been noted heading into a metastasis. This has been termed the feeding vessel sign . It is unclear whether this is a true finding or the result of older scanners with thicker slices resulting in volume averaging . However, a number of atypical features are commonly encountered.
Some tumors have a predilection for innumerable small metastases (miliary pattern):
Conversely, a pulmonary metastasis may be single. This is most frequently seen in colorectal carcinoma. Other primaries which often present with solitary metastases include :
- malignant melanoma
- skeletal sarcoma
- testicular carcinoma
- adenocarcinomas in general
Adenocarcinoma metastases, rather than displace or destroy adjacent lung parenchyma, may grow in a lepidic fashion (spread along alveolar walls) resulting in pneumonia-like consolidation. Air bronchograms may also be visible .
Cavitation is present in ~4% of cases . The most common primary is squamous cell carcinoma, most often from the head and neck or from the lung. Other primaries include adenocarcinomas, and sarcomas .
Calcification, although uncommon and more frequently a feature of benign etiology (e.g. granuloma or hamartoma) is also seen with metastases, particularly those from papillary thyroid carcinoma and adenocarcinomas. Treated metastases, osteosarcomas and chondrosarcomas may also contain calcified densities .
A halo of ground-glass opacity representing hemorrhage can be seen, particularly surrounding hemorrhagic pulmonary metastases, such as choriocarcinoma and angiosarcoma.
MRI
Although not used routinely, MRI may be as sensitive in the detection of pulmonary metastases as CT.
Treatment and prognosis
In general presence of pulmonary metastases is an ominous finding, indicating poor prognosis. The specific prognosis will, however, depend on the primary tumor.
Complications
Tumors with prominent necrosis located near a pleural surface may result in a pneumothorax. Osteosarcoma is classically described as the pulmonary metastasis that results in pneumothorax. Another cause of pneumothoraces includes cystic or cavitary pulmonary metastases.
Differential diagnosis
The differential depends on the number of nodules/masses and their imaging characteristics.
- differential of multiple pulmonary nodules
- differential of a single pulmonary nodule
- differential of miliary pulmonary nodules
- differential of a cavitating lung mass
- differential of a pulmonary mass with calcification
- differential of a pulmonary mass with surrounding ground-glass halo
Zervixkarzinom Radiopaedia • CC-by-nc-sa 3.0 • de
Carcinoma of the cervix is a malignancy arising from the cervix. It is the third most common gynecologic malignancy (after endometrial and ovarian).
Epidemiology
It typically presents in younger women with an average age of onset at around 45 years.
Risk factors
- human papillomavirus (HPV) 16 and 18 infections: for most types except for clear cell carcinoma of the cervix and mesonephric carcinoma of the cervix
- multiple sexual partners or a male partner with multiple previous or current sexual partners
- young age at first intercourse
- high parity
- immunosuppression
- certain HLA subtypes
- oral contraceptives
- nicotine/smoking (except for cervical adenocarcinoma )
Clinical presentation
Presenting symptoms include:
- vaginal bleeding
- vaginal discharge
- subclinical: an abnormal cervical cancer screening test
Pathology
Invasive cervical carcinoma is thought to arise from the transformation of cervical intraepithelial neoplasia (CIN).
Histological types
The main histological types are:
- squamous cell carcinoma of the cervix: accounts for the vast majority (80-90%) of cases and is associated with exposure to human papillomavirus (HPV)
- adenocarcinoma of the cervix: rarer (5-20%) and can have several subtypes which include
- clear cell carcinoma of the cervix
- endometroid carcinoma of the cervix: ~7% of adenocarcinomas
- mucinous carcinoma of the cervix
- adenoma malignum: ~3% of adenocarcinomas
- serous carcinoma of the cervix
- mesonephric carcinoma of the cervix: ~3% of adenocarcinomas
- neuroendocrine tumors of the cervix
- small cell carcinoma of the cervix: rare (0.5-6%)
- adenosquamous cell carcinoma of the cervix: rare
For a detailed overview, refer to:
Location
Cervical squamous cell carcinoma arises from the squamocolumnar junction while adenocarcinomas arise from the endocervix. The squamocolumnar junction is situated on the ectocervix in younger patients though regresses into the endocervical canal with age. Hence cervical tumors tend to be exophytic in younger patients and endophytic with advancing age.
Radiographic features
General features
In order to be radiographically visible, tumors must be at least stage Ib or above (see staging). MRI is the imaging modality of choice to depict the primary tumor and assess the local extent. Distant metastatic disease is best assessed with CT or PET, where available.
Although the FIGO staging system is clinically based, the revised 2009 FIGO staging encourages imaging as an adjunct to clinical staging. MRI can stratify patients to the optimum treatment group of primary surgery or combined chemotherapy and radiotherapy. Tumors stage IIa and below are treated with surgery.
Ultrasound
- hypoechoic, heterogeneous mass involving the cervix
- may show increased vascularity on color Doppler
- although cervical cancer is staged clinically, ultrasound can be a useful adjunct by showing
- size (<4 cm or >4 cm)
- parametrial invasion
- tumor invasion into the vagina
- tumor invasion into adjacent organs
- hydronephrosis: implies stage IIIB tumor.
CT
CT, in general, is not very useful in the assessment of the primary tumor, but it can be useful in assessing the advanced disease. It is performed primarily to assess adenopathy, but also has roles in defining advanced disease, monitoring distant metastasis, planning the placement of radiation ports, and guiding percutaneous biopsy.
On CT, the primary tumor can be hypoenhancing or isoenhancing to normal cervical stroma (~50% ).
PET-CT
PET-CT in conjunction with pelvic MRI is often used as an imaging strategy in helping stage cervical carcinoma.
MRI
A dedicated MRI protocol is often useful for optimal imaging assessment.
The normal low signal cervical stroma provides intrinsic contrast for the high signal cervical tumor.
- T1: usually isointense compared with pelvic muscles
- T2
- hyperintense relative to the low signal of the cervical stroma
- hyperintensity is thought to be present regardless of histological subtype
- T1 C+ (Gd)
- contrast is not routinely used, though it may be helpful to demonstrate small tumors considered for trachelectomy
- on contrast-enhanced T1-weighted images, tumor presents as a high signal relative to the low signal of the cervical stroma
For further information, see the article: MRI reporting guidelines for cervical cancer.
Staging
The FIGO staging system is the most commonly adopted. See: cervical cancer staging
Treatment and prognosis
Prognosis is affected by many factors which include:
- tumor stage
- the volume of the primary mass
- histologic grade
Five-year survival rates vary between 92% for stage I disease and 17% for stage IV disease .
One of the keys roles of the radiologist is to help determine staging, as this may lead to appropriate management pathway either with surgery or chemo-radiotherapy. At the time of writing stage IIa vs. IIb is considered as an important separator in deciding whether a case is operable or not.
Differential diagnosis
For a mass involving the cervix consider:
- cervical polyp
- cervical leiomyoma
- invasion of the cervix from
- cervical lymphoma
- adenoma malignum: often considered a subtype of mucinous carcinoma of the cervix
- metastases to the cervix
- cervical ectopic pregnancy: consider with women of childbearing age with a high βHCG
Practical points
- MRI T2WI to assess parametrial invasion (stage 2b) is crucial to determine if the patient is candidate for surgery or not

 Assoziationen und Differentialdiagnosen zu Lungenmetastasen bei Zervixkarzinom:
Assoziationen und Differentialdiagnosen zu Lungenmetastasen bei Zervixkarzinom: