pott disease






















Tuberculous spondylitis, also known as Pott disease, refers to vertebral body osteomyelitis and intervertebral diskitis from tuberculosis (TB). The spine is the most frequent location of musculoskeletal tuberculosis, and commonly related symptoms are back pain and lower limb weakness/paraplegia.
Epidemiology
Tuberculous spondylitis is one of the more common infections of spine in countries where TB is prevalent. Unfortunately, the incidence of tuberculous spondylitis, as with other forms of TB, is on the rise, due to new multiple drug resistant strains.
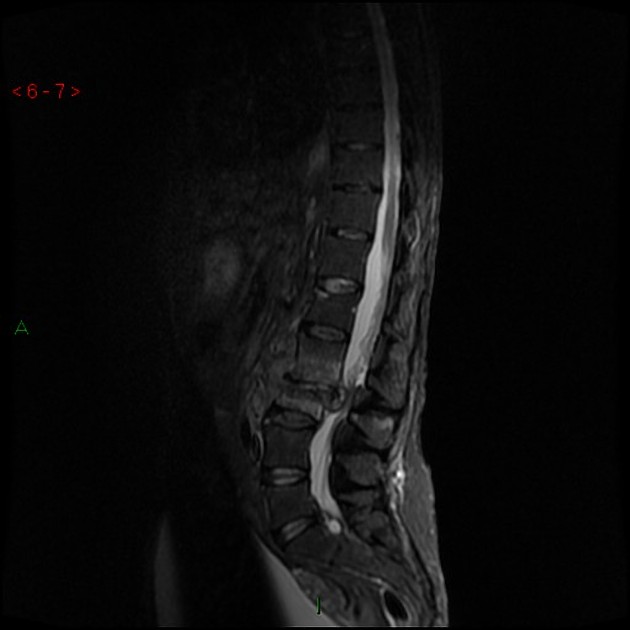
Diskitis and/or osteomyelitis comprise approximately 50% of all musculoskeletal tuberculosis, and usually affects the lower thoracic and upper lumbar levels of the spine .
Clinical presentation
Patients usually present with back pain, lower limb weakness/paraplegia, and kyphotic deformity. Constitutional symptoms (fever and weight loss) are also common but not as pronounced as with bacterial diskitis/osteomyelitis.
Pathology
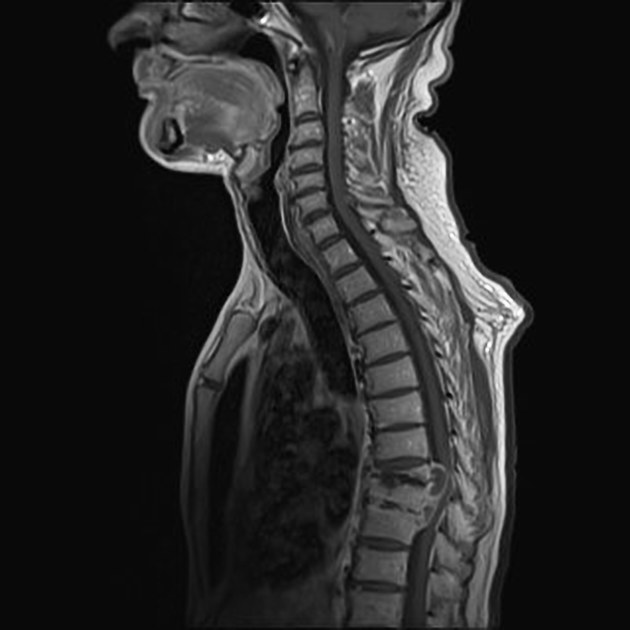
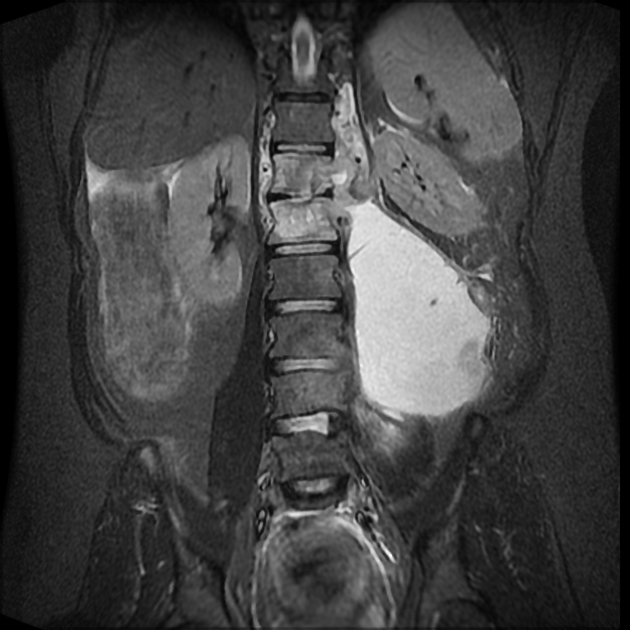
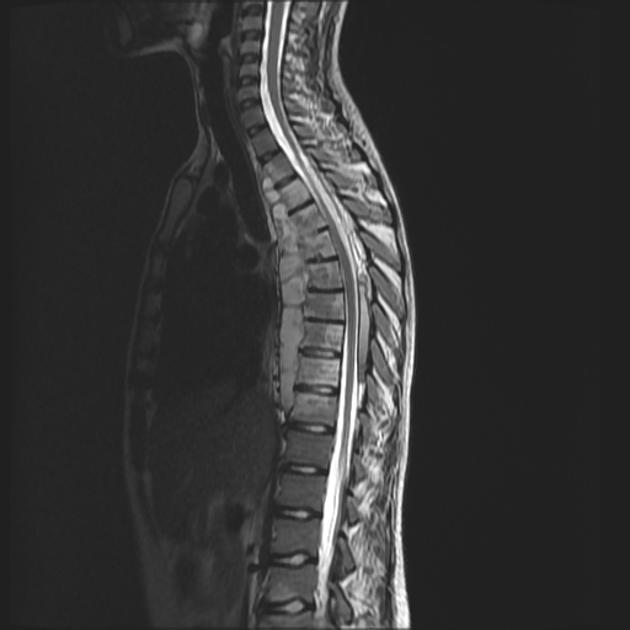
The spine is involved due to hematogenous spread via the venous plexus of Batson . There is usually a slow collapse of one or usually more vertebral bodies, which spreads underneath the longitudinal ligaments. This results in an acute kyphotic or "gibbus" deformity. This angulation, coupled with epidural granulation tissue and bony fragments, can lead to cord compression. Unlike pyogenic infections, the discs can be preserved and it more commonly involves the thoracic spine. In late-stage spinal TB, large paraspinal abscesses without severe pain or frank pus are common, leading to the expression "cold abscess".
Radiographic features
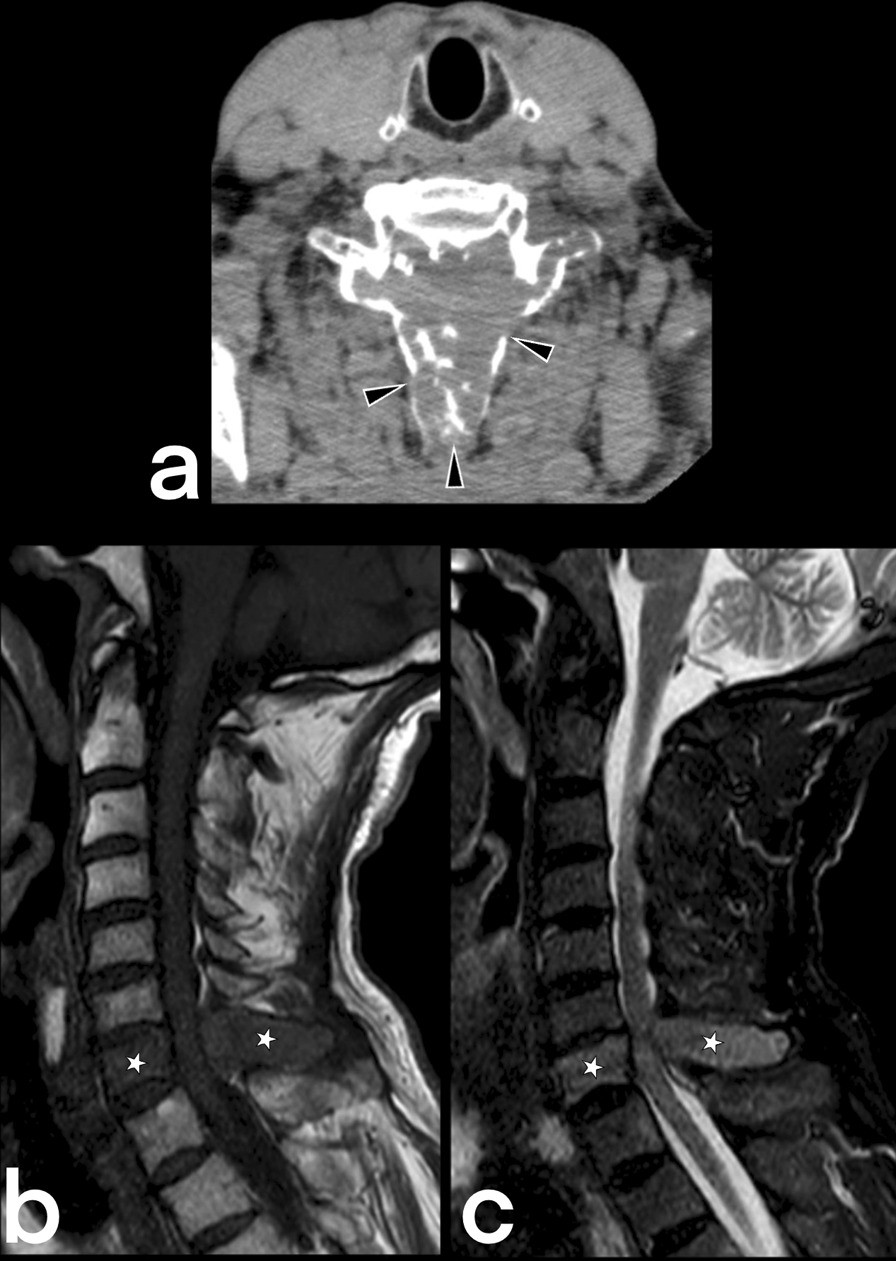
Plain radiograph
The spread of infection is typically described as 'sub-ligamentous': beneath the anterior longitudinal ligament, usually sparing the posterior elements and often involving multiple levels.
Tuberculous spondylitis can be difficult to detect in early stages because of relative preservation of the disc space.
A reduction in vertebral height is often seen with the irregularity of the anterosuperior endplate being relatively early and subtle sign. Due to the subligamentous extension, there may be some irregularity of the anterior vertebral margin. This is a classical appearance with TB spondylitis.
Later, paraspinal collections can develop which can be remarkably large.
Ivory vertebrae can result in re-ossification. Other associated features may include:
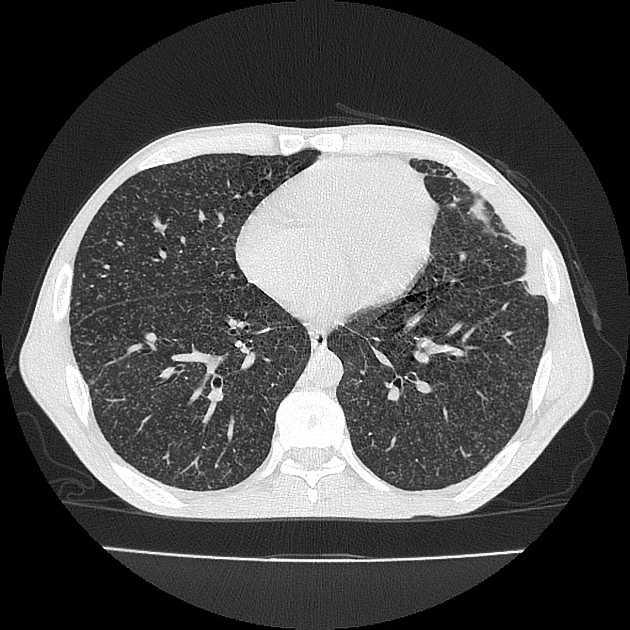
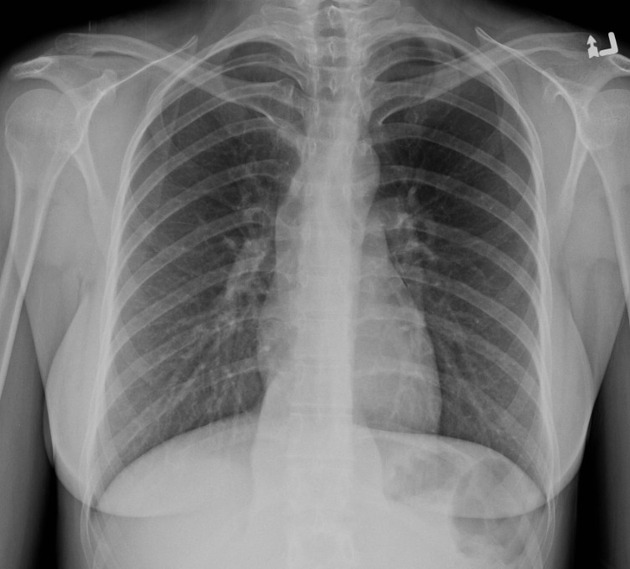
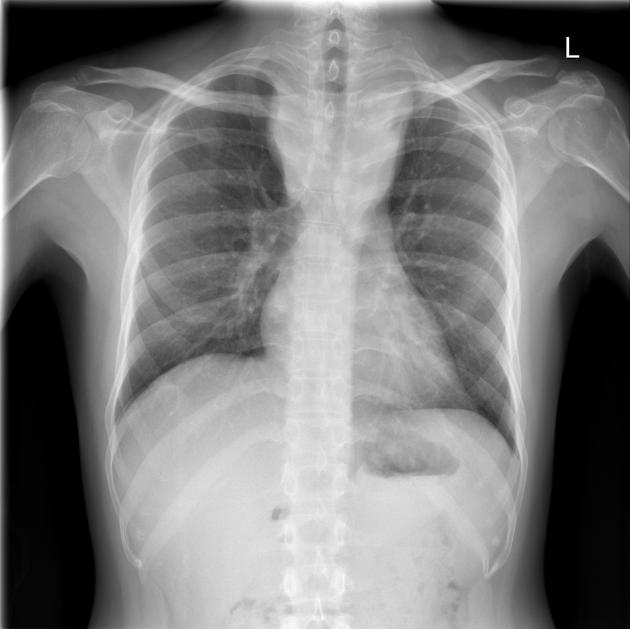
As with other extrapulmonary TB, the chest film may be unrevealing (no pulmonary lesions seen in up to 50% of cases), with the source being a primary lung lesion that is clinically silent.
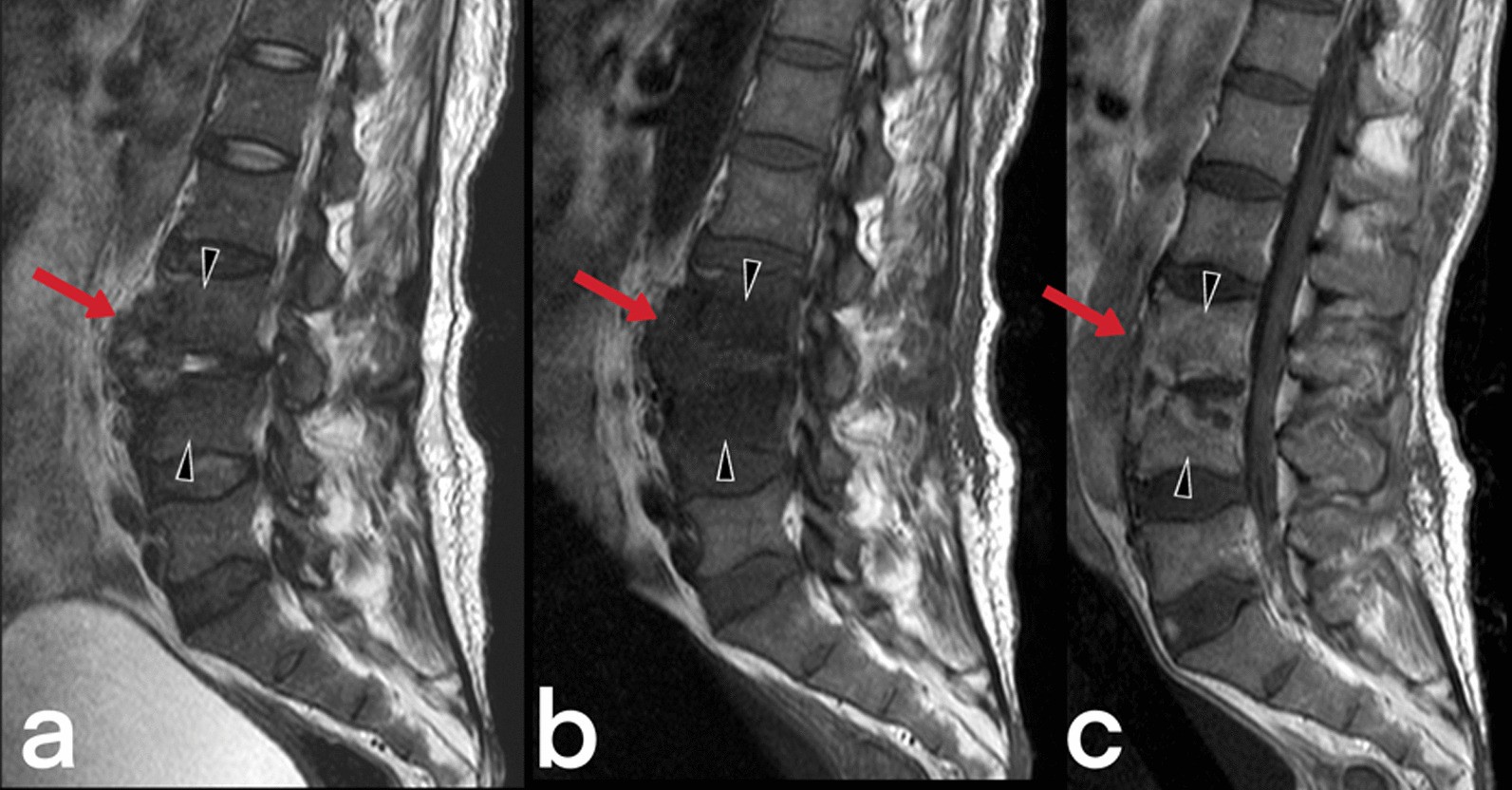
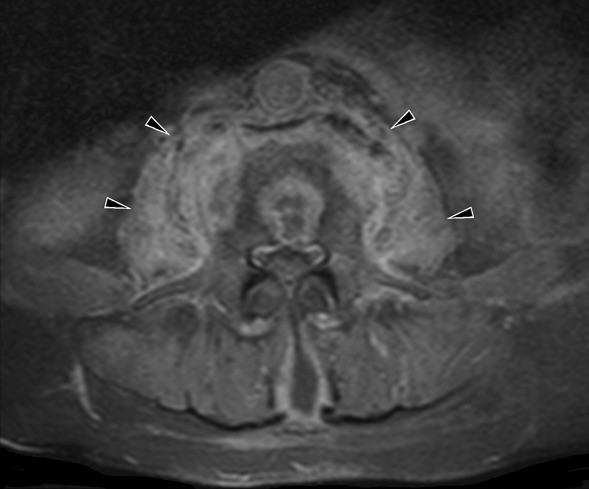
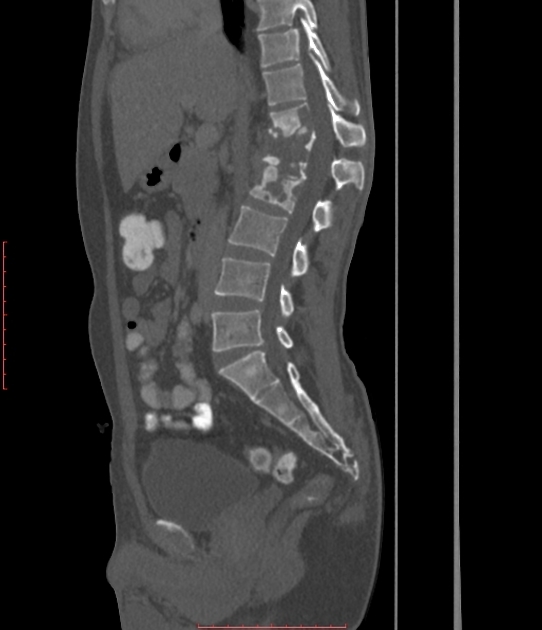
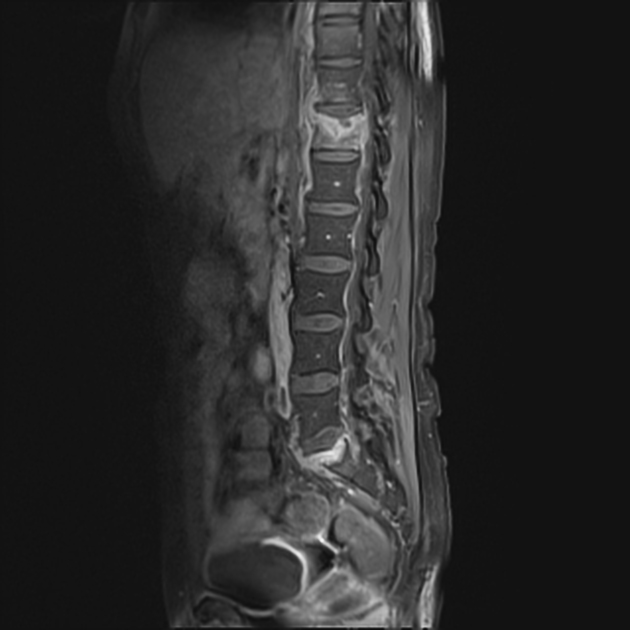
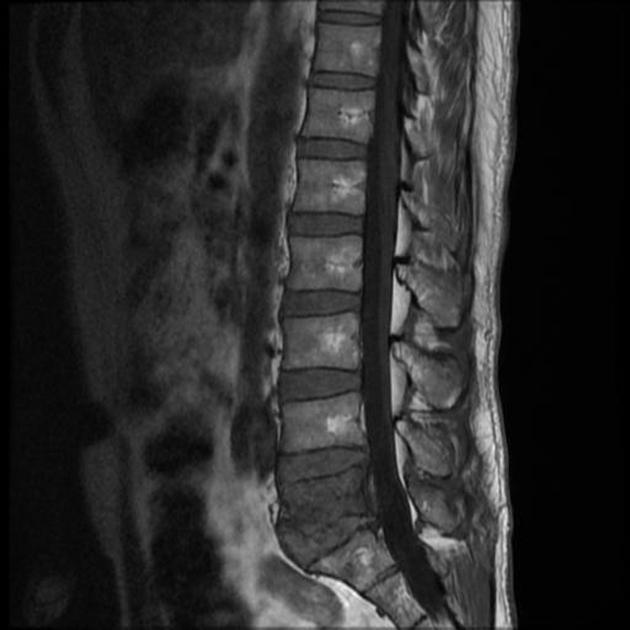
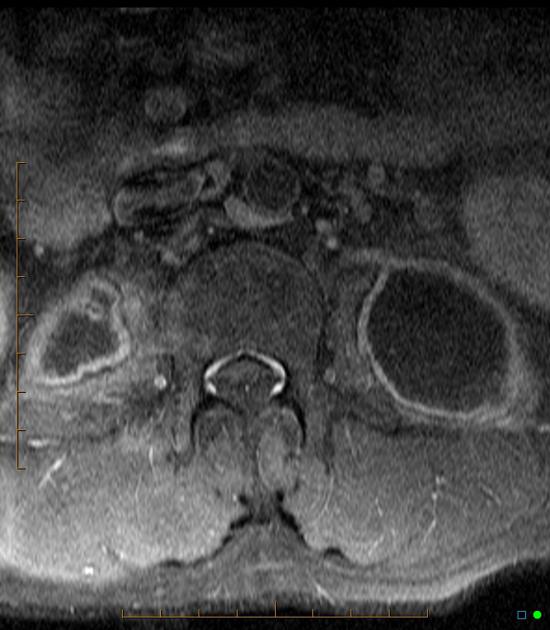
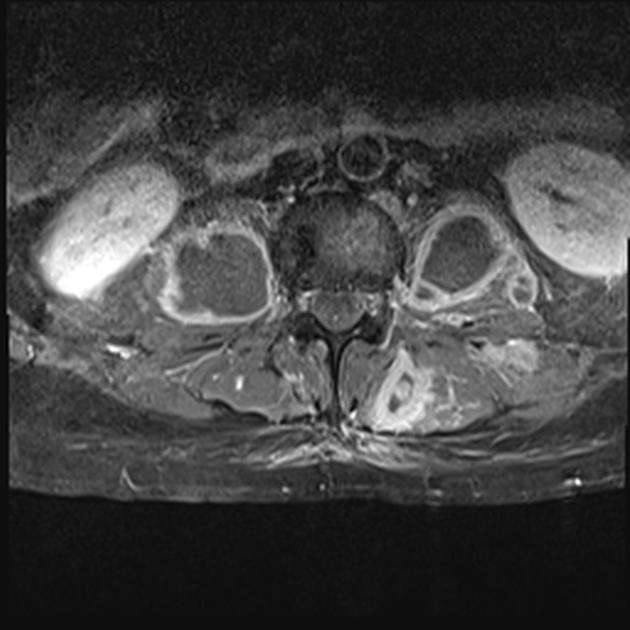
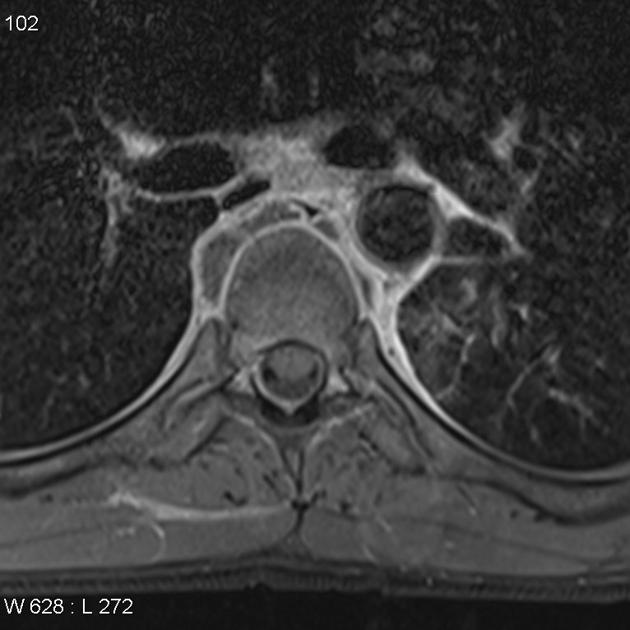
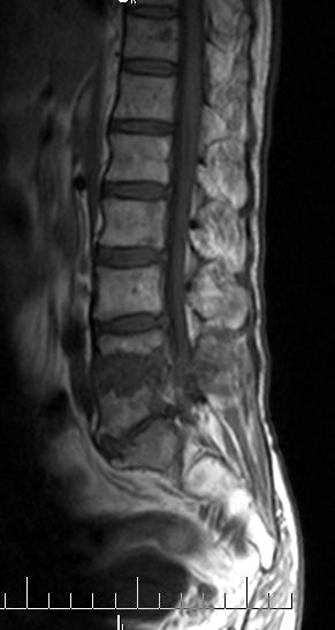
CT and MRI
Cross-sectional imaging is required to assess better the extent of involvement and particularly for the presence of an epidural component and cord compression. MRI is the modality of choice for this, with CT with contrast being a distant second.
Features include irregularity of both the endplate and anterior aspect of the vertebral bodies, with bone marrow edema and enhancement seen on MRI:
- T1: hypointense marrow in adjacent vertebrae
- T2: hyperintense marrow, disc, soft tissue infection
- T1 C+ (Gd): marrow, subligamentous, discal, dural enhancement
The paraspinal collections are typically well circumscribed, with fluid centers and well-defined enhancing margins .
Differential diagnosis
In many parts of the developing world, TB is the most common cause of vertebral body infection, with the majority of cases seen in patients under the age of 20. TB can also affect the meninges of the spine, causing an intense pachymeningitis that enhances dramatically.
- brucellosis: can present as granulomatous osteomyelitis of the spine that can be difficult to distinguish from TB. Both are acid-fast bacilli, which may cause caseating granuloma(s)
- fungal infection
- sarcoidosis
- pyogenic infection
- compared to pyogenic infection tuberculous spondylitis has relatively preserved disk-space height, forms large paraspinal abscesses with a smooth enhancing wall and there is usually systemic involvement of multiple organs
- see: tuberculous spondylitis versus pyogenic spondylitis
- metastasis
Siehe auch:
- Tuberkulose
- Spondylodiscitis
- Spondylitis
- skelettale Tuberkulose
- Tuberkulose der Wirbelsäule und des Spinalkanals
- tuberkulöse Spondylodiscitis
und weiter:

 Assoziationen und Differentialdiagnosen zu tuberkulöse Spondylitis:
Assoziationen und Differentialdiagnosen zu tuberkulöse Spondylitis: