Chronisch obstruktive Lungenerkrankung

Chronic obstructive pulmonary disease (COPD) represents a spectrum of obstructive airway diseases. It includes two key components which are chronic bronchitis-small airways disease and emphysema.
Epidemiology
The most common cause has historically been, and unfortunately continues to be, smoking. It takes many years of smoking to develop COPD and as such typically patients are older adults. There are however a number of other less common risk factors/etiologies, each with their own demographics. They include:
- cigarette smoking
- industrial exposure (e.g. mining)
- cystic fibrosis
- alpha-1 antitrypsin deficiency
- intravenous drug use
- immune deficiency syndromes
- vasculitides and connective tissue disorders
Clinical presentation
Symptoms of COPD include dyspnea on exertion, wheezing, productive cough, pursed-lip breathing, and use of accessory muscles. Patients with chronic bronchitis are classically "blue bloaters," while those with emphysema are known as "pink puffers". In advanced cases, muscle wasting, asterixis, and peripheral edema may be seen.
ECG
- poor R wave progression
- requires an R wave in V3 <3 mm
- clockwise rotation of the heart secondary to hyperinflation results in a delayed precordial transition zone
- the lead in which the R/S ratio becomes >1, usually occurring in V3 or V4, shifts laterally (to V5 or V6)
- deep S waves in the lateral leads (I, aVL, V5, V6)
- low QRS voltage
- amplitude of QRS complexes <5 mm in the limb leads or <10 mm in the precordial leads
- right ventricular hypertrophy
- right axis deviation
- dominant R wave in V1 with an amplitude >7 mm
- often associated with "P pulmonale" (right atrial enlargement)
- multifocal atrial tachycardia
Pathology
In contrast to asthma, the histologic changes of COPD are irreversible and gradually progress over time. In chronic bronchitis, there is diffuse hyperplasia of mucous glands with associated hypersecretion and bronchial wall inflammation.
Emphysema involves the destruction of alveolar septa and pulmonary capillaries, leading to decreased elastic recoil and resultant air trapping. The morphological subtypes of emphysema include:
- centrilobular (centriacinar): associated with smoking and spreads peripherally from bronchioles
- panacinar: homozygous AAT1 deficiency and uniformly destroys alveoli
- paraseptal (distal acinar): involves the distal airways
Pulmonary function testing (PFT) reveals airflow obstruction, as evidenced by a decreased forced expiratory volume in 1 second to forced vital capacity (FEV1/FVC) ratio. Administration of bronchodilators has no effect, unlike the reversible obstruction seen in asthma.
Severity classification
The global initiative for chronic obstructive lung disease (GOLD) staging system is a commonly used severity staging system based on airflow limitation. According to this, there are 4 key stages with latest revision at time of writing being in 2019 :
- stage I: mild, FEV1 > 80% of normal
- stage II: moderate, FEV1 = 50-79% of normal
- stage III: severe, FEV1 = 30-49% of normal
- stage IV: very severe, FEV1 <30% of normal or <50% of normal with presence of chronic respiratory failure present
The FEV1:FVC ratio should be <0.70 for all stages.
The GOLD staging system may be insensitive in early stages .
Quantitative analysis of low attenuation areas can aid in classifying the severity of the disease .
Clinical phenotypes
Several distinct clinical phenotypes have been described :
- emphysema predominant
- airways predominant
- small airways predominant
- large airways predominant
- mixed
Radiographic features
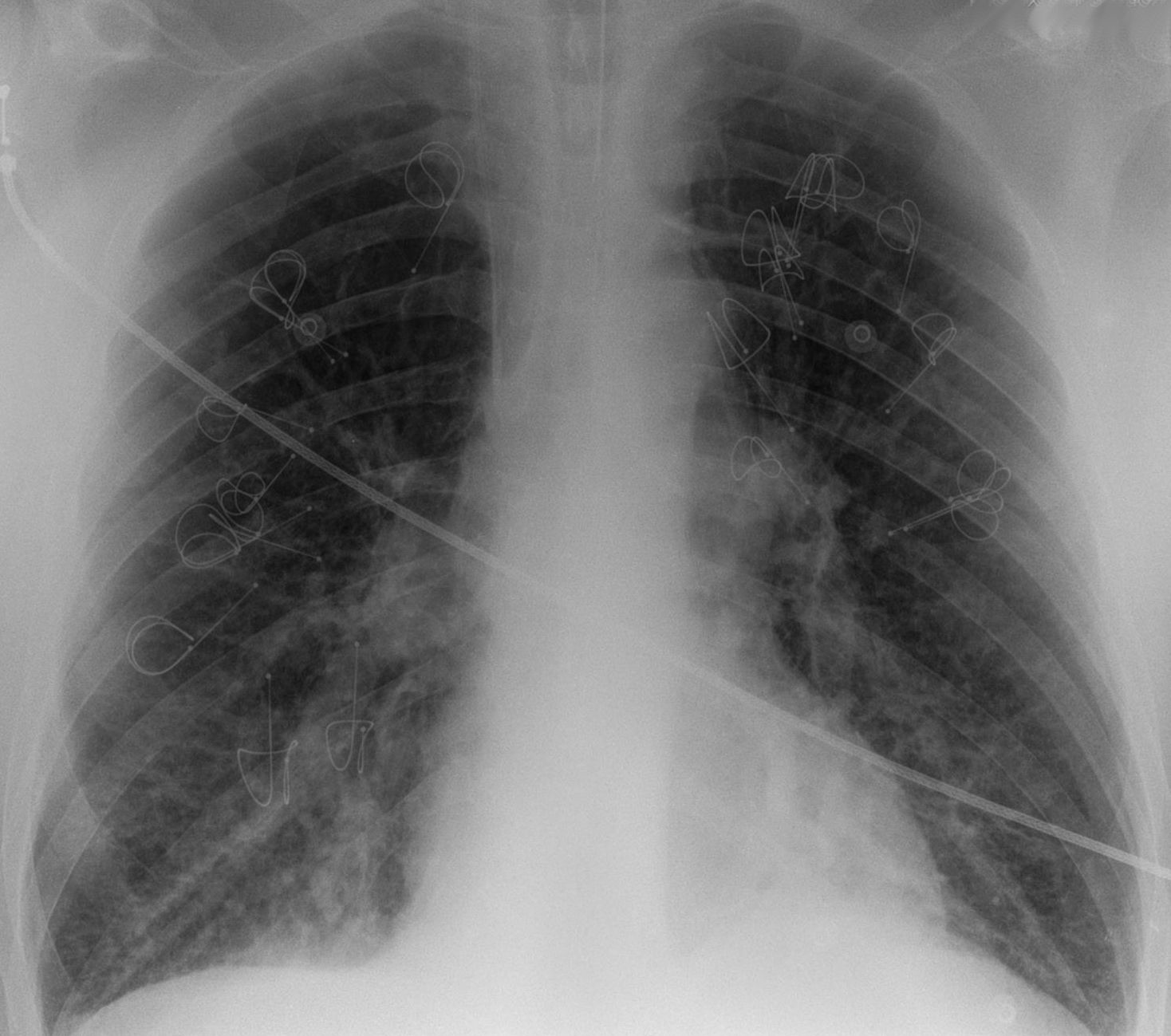
Plain radiograph
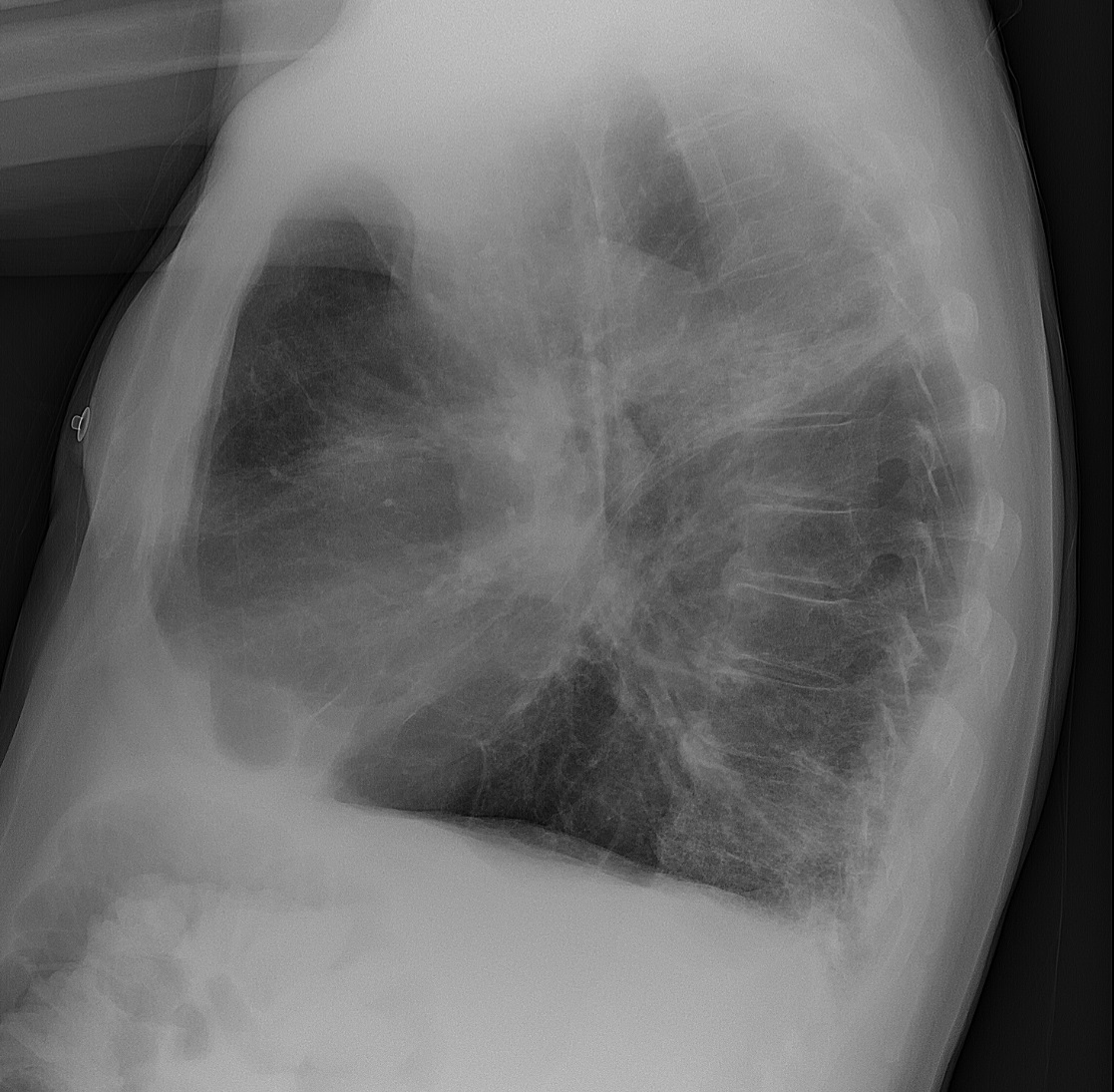
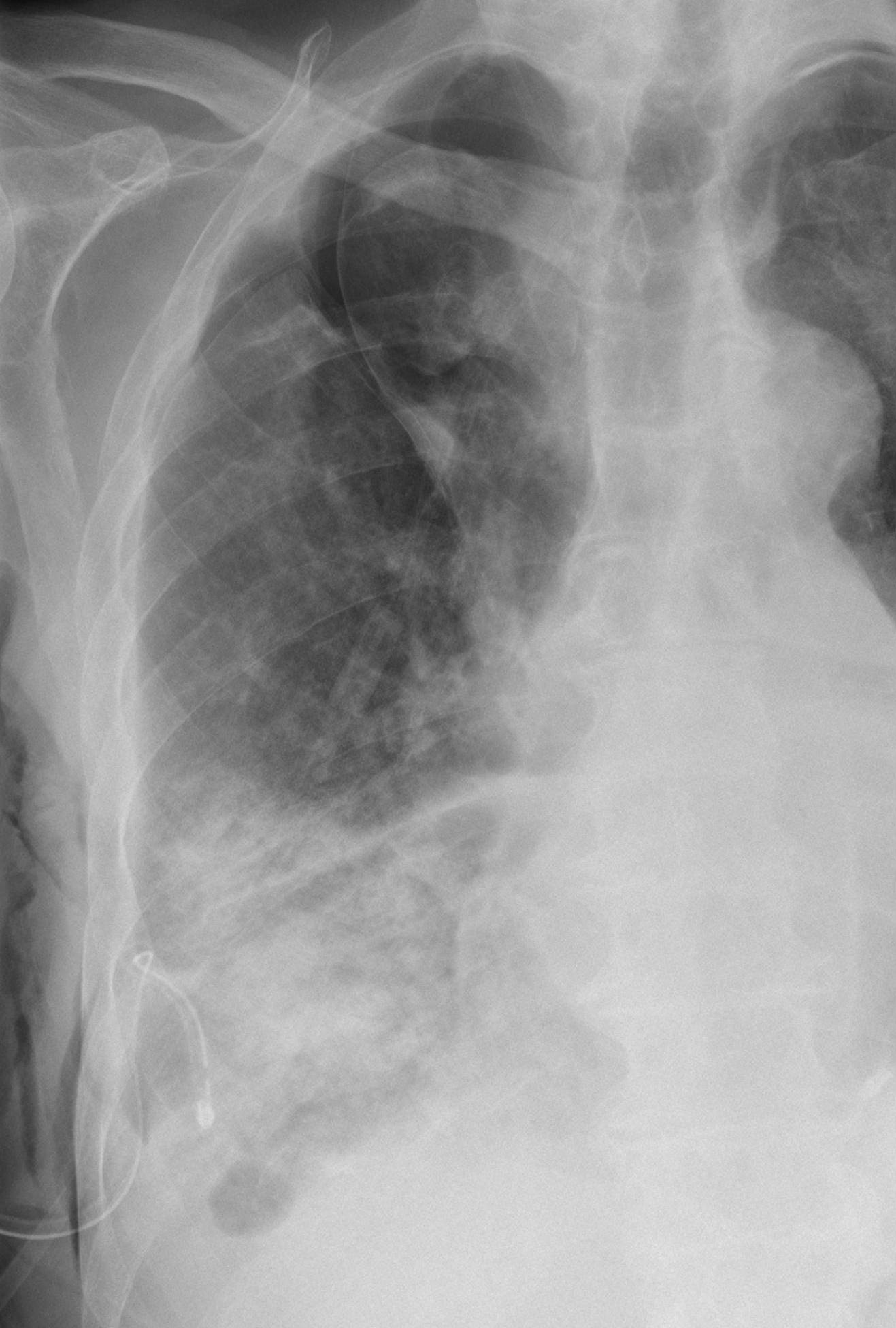
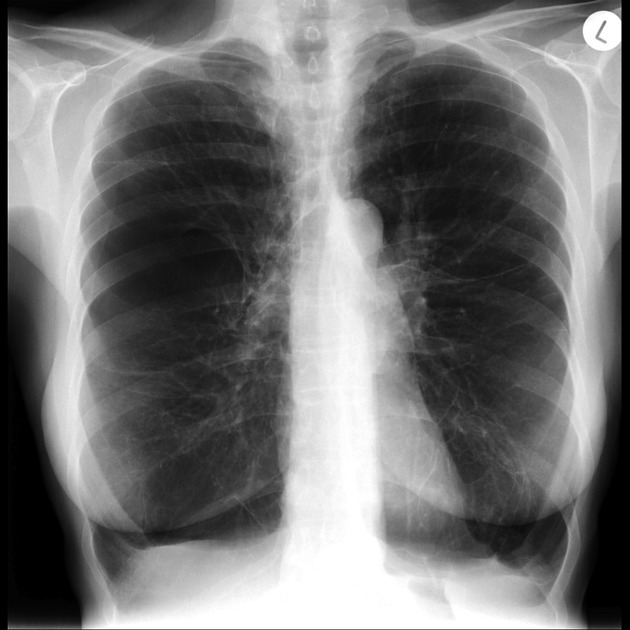
Findings of chronic bronchitis on chest radiography are non-specific and include increased bronchovascular markings and cardiomegaly. Emphysema manifests as lung hyperinflation with flattened hemidiaphragms, a small heart, and possible bullous changes. On the lateral radiograph, a "barrel chest" with widened anterior-posterior diameter may be visualized. The "saber-sheath trachea" sign refers to marked coronal narrowing of the intrathoracic trachea (frontal view) with concomitant sagittal widening (lateral view).
CT
Findings of COPD may be seen in a variety of CT chest studies, e.g. contrast-enhanced CT, CT pulmonary angiography, staging CT chest, HRCT chest, etc.
Chronic bronchitis
In chronic bronchitis, bronchial wall thickening may be seen in addition to enlarged vessels. Repeated inflammation can lead to scarring with bronchovascular irregularity and fibrosis.
Emphysema
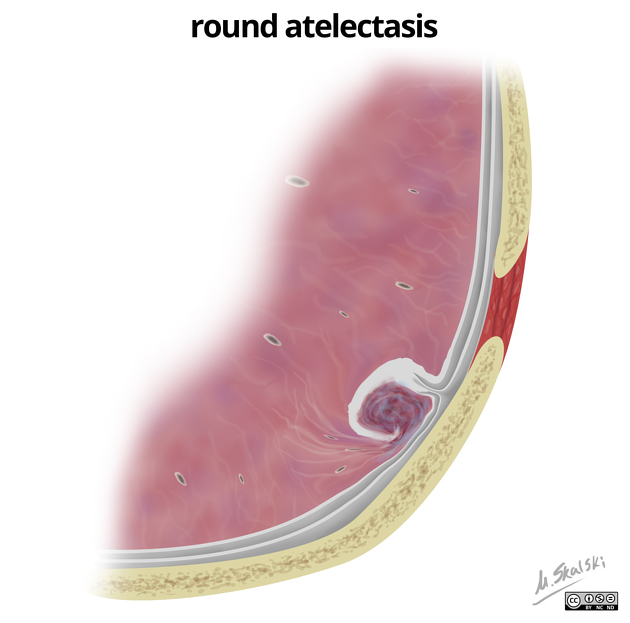
Emphysema is diagnosed by alveolar septal destruction and airspace enlargement, which may occur in a variety of distributions. Centrilobular emphysema is predominantly seen in the upper lobes with panacinar emphysema predominating in the lower lobes. Paraseptal emphysema tends to occur near lung fissures and pleura. Formation of giant bullae may lead to compression of mediastinal structures, while rupture of pleural blebs may produce spontaneous pneumothorax/pneumomediastinum.
Complications
Exacerbations
- exacerbation of COPD
- infective exacerbation of COPD
- non-infective exacerbation of COPD
Treatment and prognosis
Barring whole-lung transplantation, there is currently no cure for COPD, but it is highly preventable and treatable.
Lifestyle measures
Risk factor reduction via smoking cessation, occupational health, and air pollution reduction should be instituted. Patients should also have all available vaccinations.
Pharmacology
Pharmacological management is generally first-line. It involves the use of bronchodilators, corticosteroids, and other medications (e.g. methylxanthines, leukotriene receptor antagonists, phosphodiesterase type-4 inhibitors, omalizumab), as well as supplemental oxygen and pulmonary rehabilitation. Long-acting β2-agonist (LABA) and long-acting muscarinic antagonist (LAMA) combination therapies are currently considered the most effective strategy .
Acute exacerbations are treated with high-dose corticosteroids, short-acting bronchodilators, supplemental oxygen, and antibiotics if indicated.
Surgery
Surgical therapy is usually reserved for COPD refractory to pharmacological management. In addition to the aforementioned whole-lung lung transplant, other surgical procedures include:
- endobronchial valve or intrabronchial valve
- bullectomy
- lung volume reduction surgery
Siehe auch:
- Pneumothorax
- Pleura
- Mediastinalemphysem
- Vaskulitis
- air trapping
- saber-sheath trachea
- Kardiomegalie
- zystische Fibrose
- Alpha-1-Antitrypsin-Mangel
- Lappenspalt
- fibrosis
- spontaneous pneumothorax secondary to COPD
- mediastinal structures
- Emphysem
und weiter:
- penetrierendes Aortenulkus (PAU)
- portalvenöses Gas
- Morbus Fabry
- deep sulcus sign Begriffsklärung
- saber sheath trachea
- chest radiograph assessment using ABCDEFGHI
- Anthrakose
- pneumatosis intestinalis (mnemonic)
- Asthma bronchiale
- dirty chest
- deep sulcus sign Bettlunge
- pulmonary arterial hypertension classification - third world symposium on PAH
- pneumothorax in the exam
- diffuse Trachealverengung
- Emphysemindex

 Assoziationen und Differentialdiagnosen zu Chronisch obstruktive Lungenerkrankung:
Assoziationen und Differentialdiagnosen zu Chronisch obstruktive Lungenerkrankung: