Necrotizing enterocolitis (NEC)







Necrotizing enterocolitis (NEC) is the most common gastrointestinal condition in premature neonates. It is characterized by inflammation, ischemia, and permeability of the neonatal bowel wall to bacteria. It is potentially life-threatening with significant associated morbidity .
Epidemiology
NEC usually develops 2-3 days following birth, with 90% developing within the first 10 days of life . The incidence is inversely proportional to gestational age, with 90% occurring in premature infants. Its overall incidence is ~1 in 1000 births but is as high as 20% in low birth weight infants (<1500 grams) .
Clinical presentation
The presentation is often non-specific and includes:
- poor feeding
- bile stained vomitus
- abdominal distension
- blood-stained stools +/- explosive diarrhea
- respiratory distress with acidosis
- sepsis
Risk factors
- prematurity (50-80%)
- congenital heart disease
- perinatal asphyxia
- decreased umbilical flow in utero
Pathology
NEC is usually idiopathic and multi-factorial. A combination of ischemic and infective etiology with added contributive factors such as immature immunity have been proposed . Although a partially infective etiology has been hypothesized, no causative organism has been isolated. Translocation of intestinal flora through immature mucosa has been postulated .
Inflammation starts from the mucosal surface and progresses to hemorrhagic and coagulative necrosis. There is ensuing loss of mucosal integrity, transmural necrosis, and perforation.
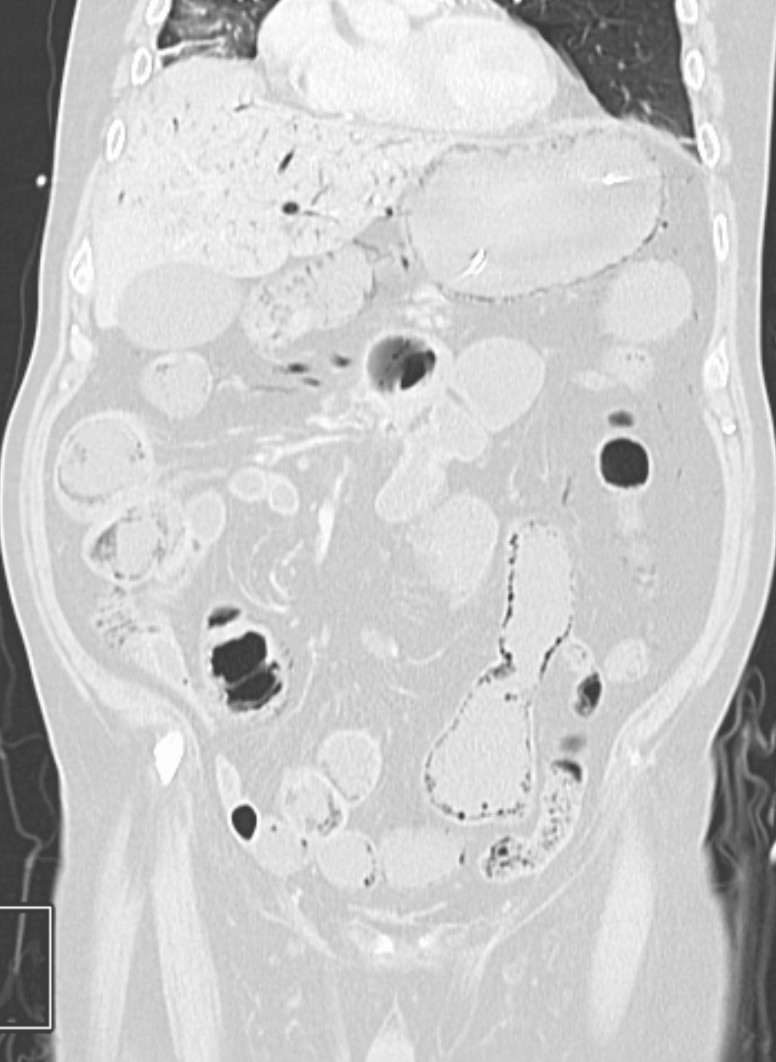
Although NEC can affect any part of the large or small bowel, the most common location is the terminal ileum. The right colon (including cecum) is occasionally involved. Involvement of the stomach is less common.
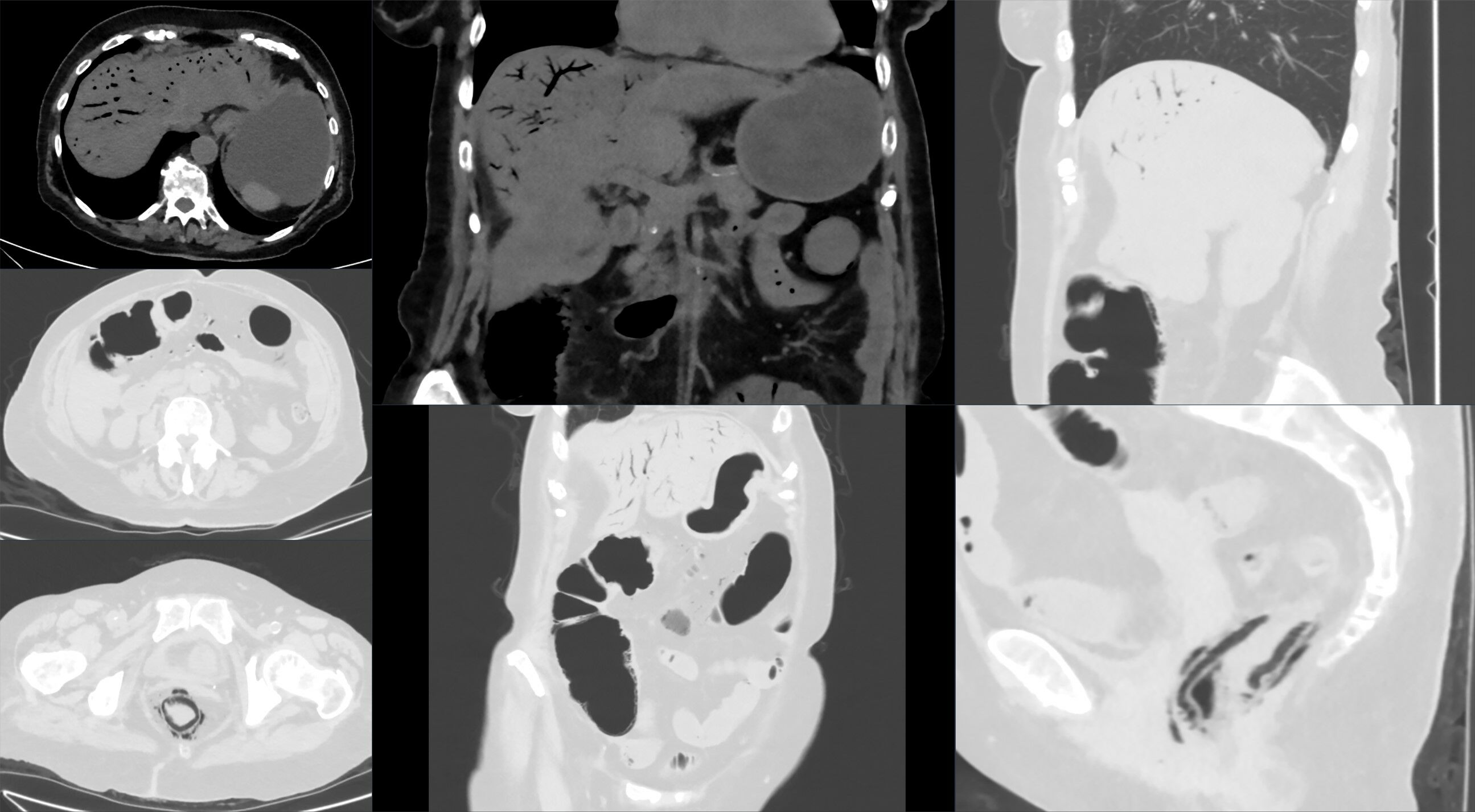
Radiographic features
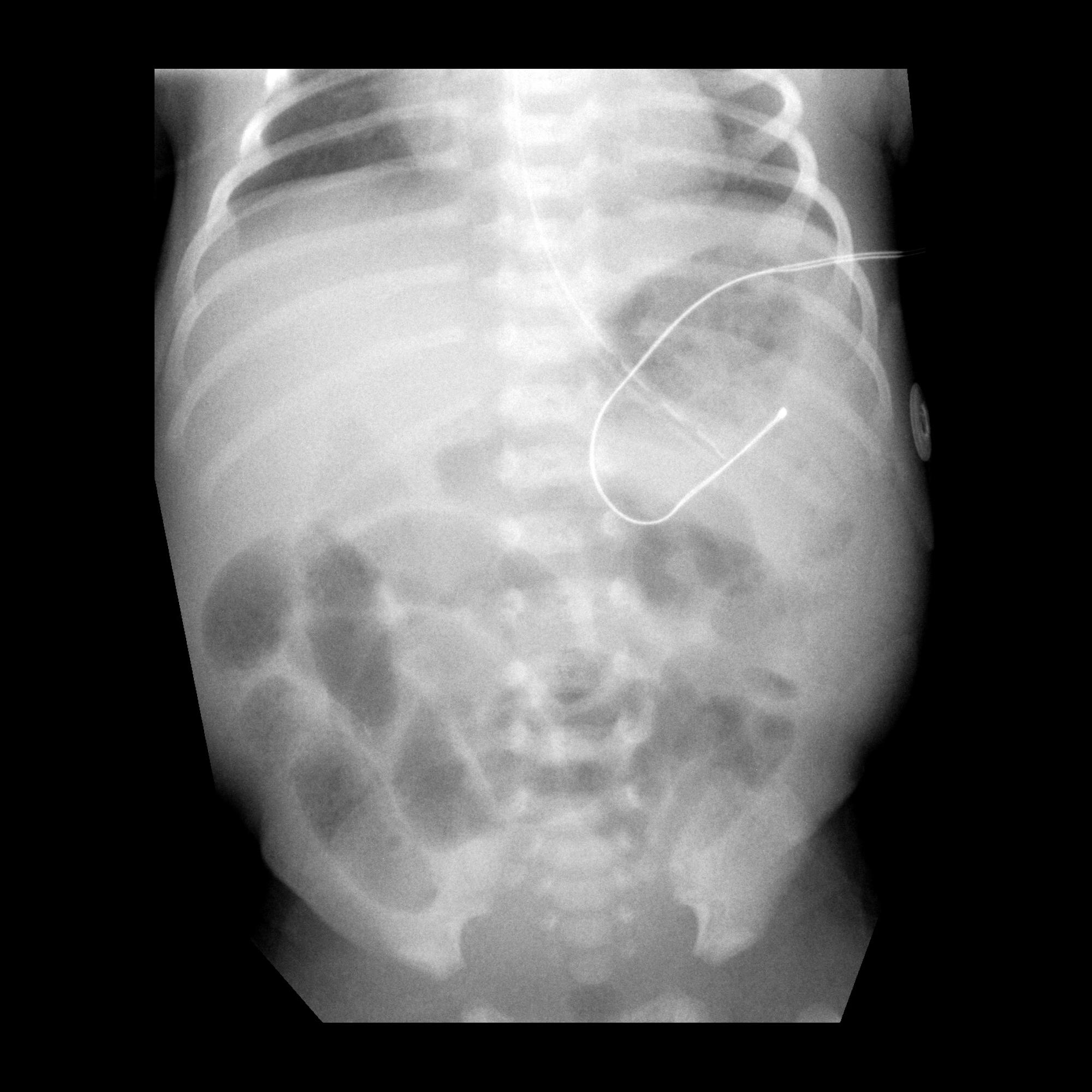
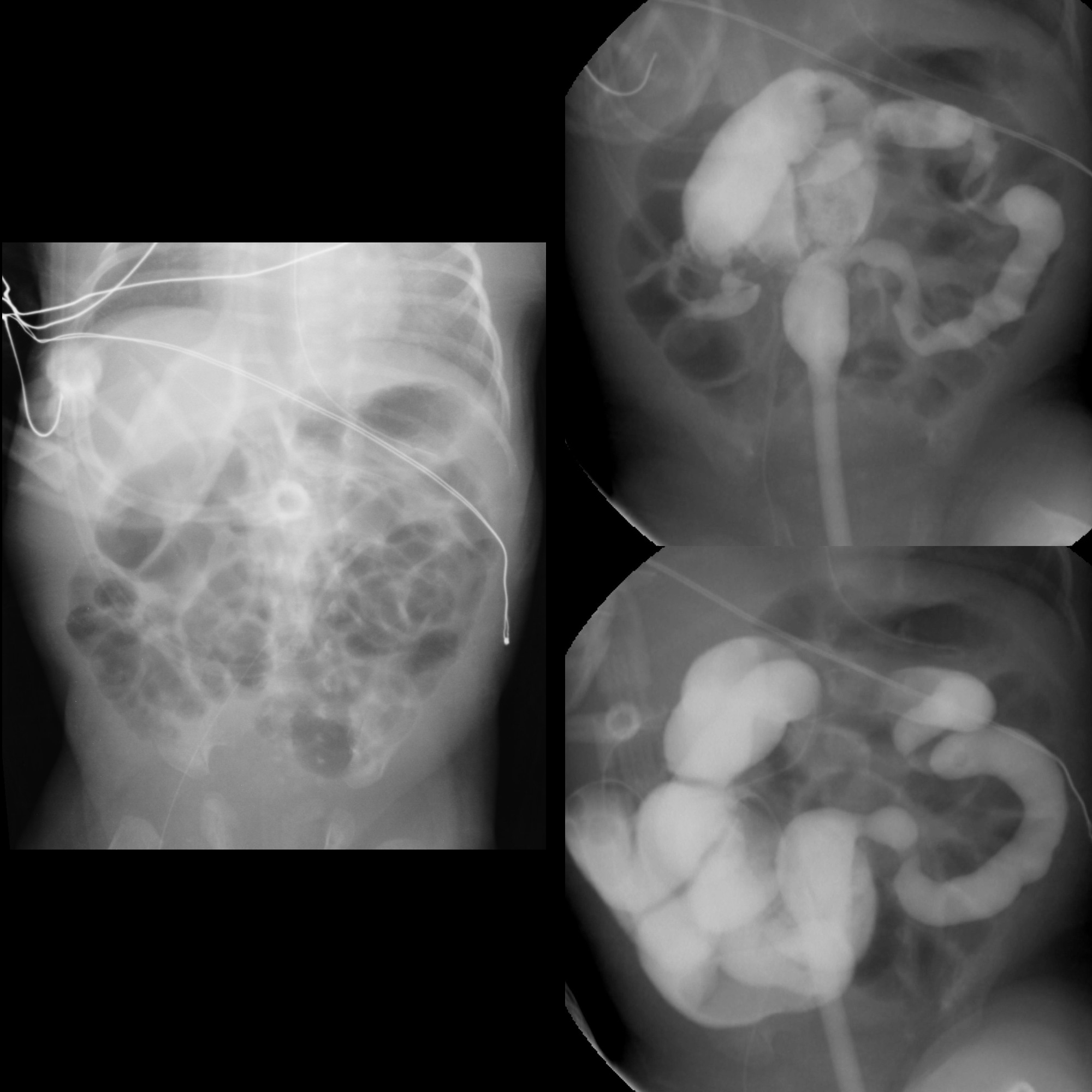
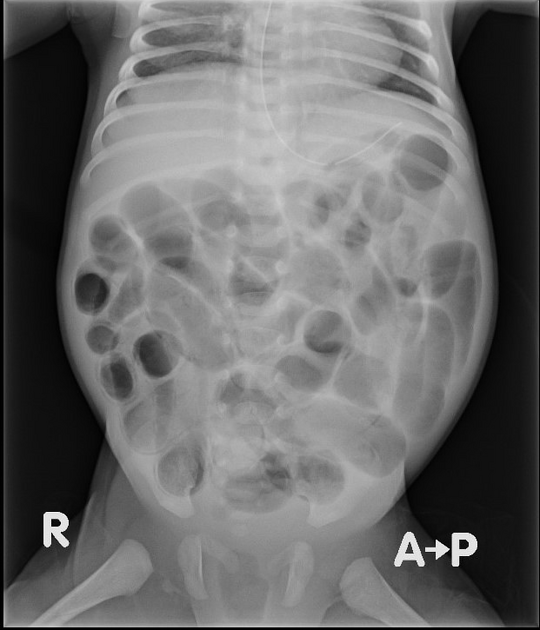
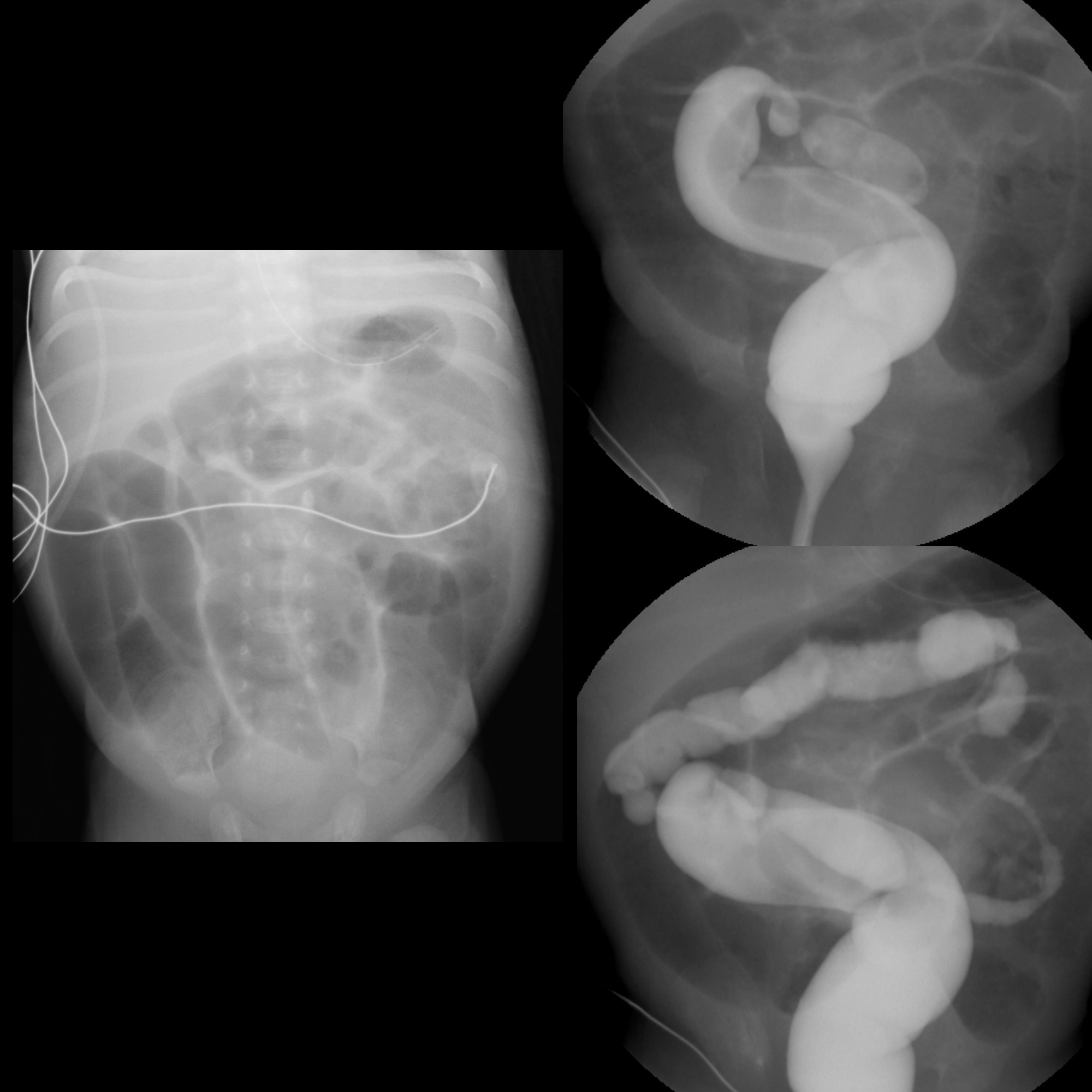
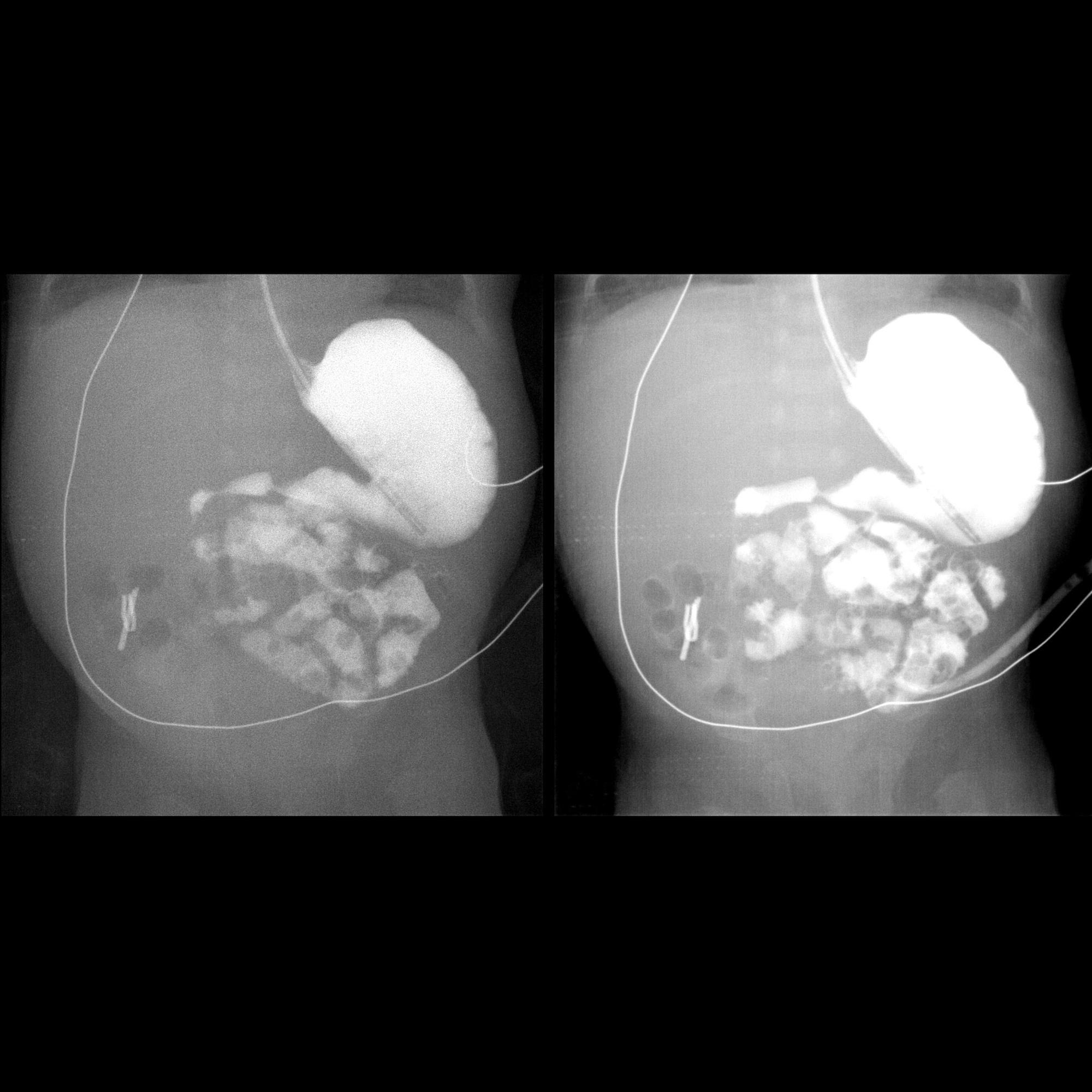
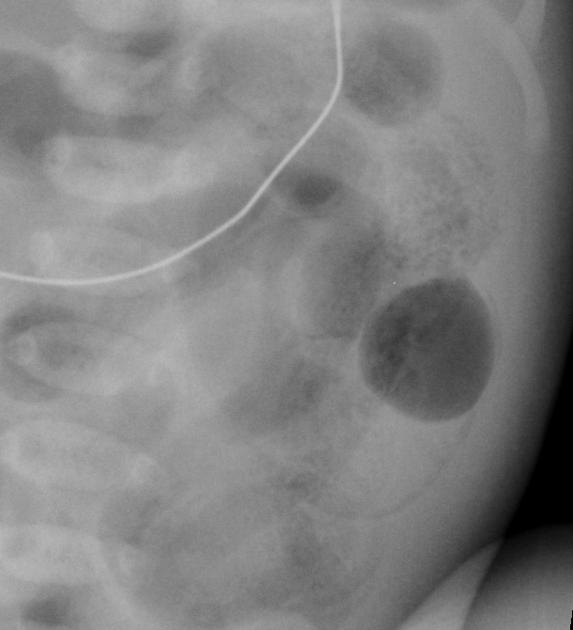
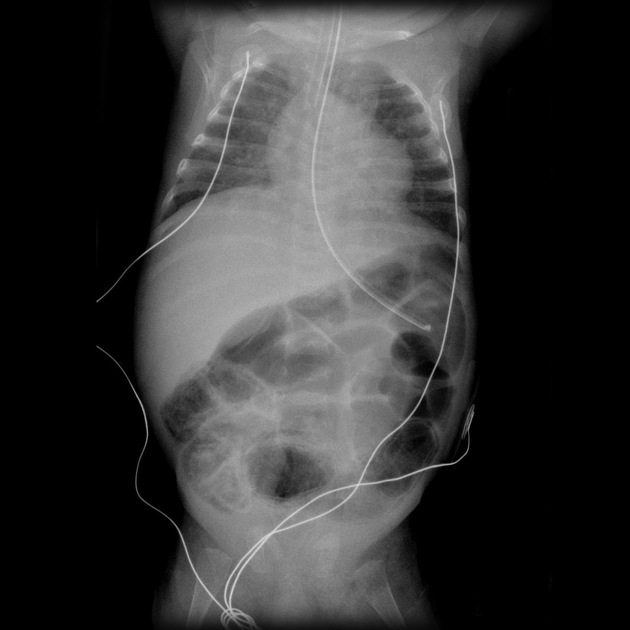
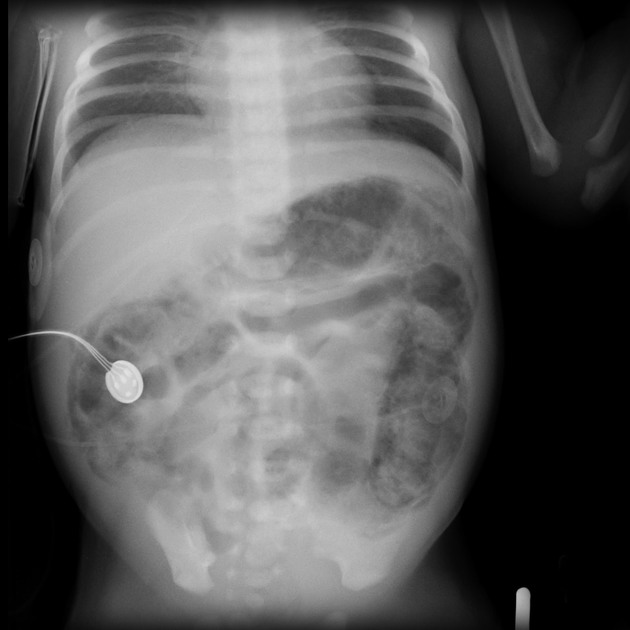
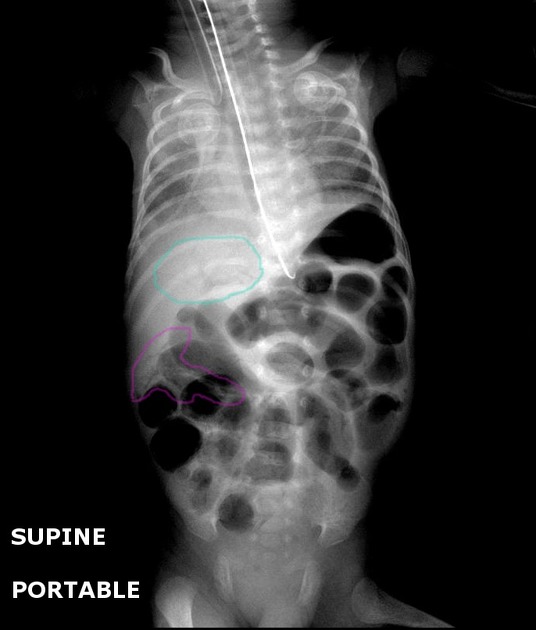
Plain radiograph
Supine abdominal x-rays are the mainstay of diagnosis. If NEC is suspected clinically, or there is a concern on supine films, an additional cross-table lateral or left-lateral decubitus view provides increased sensitivity . Findings include:
- dilated bowel loops (often asymmetrical in distribution)
- loss of the normal polygonal gas shape
- bowel wall edema with thumbprinting
- pneumatosis intestinalis
- portal venous gas
- pneumoperitoneum indicates severe disease
- only 50-75% of patients with proven perforation will have visible free gas
- air on both sides of the bowel (Rigler sign)
- air outlining the falciform ligament (football sign)
For follow-up, supine and lateral projections have been recommended for the first 48 hours as this is when most perforation occurs. After 48 hours, vertical beam supine projections may be sufficient if there no concern for perforation .
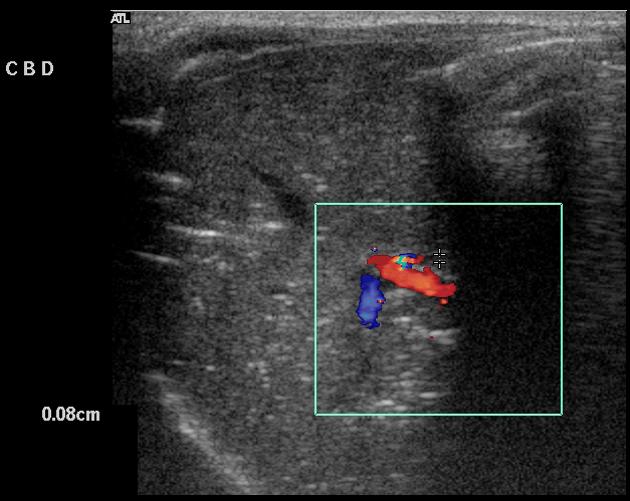
Ultrasound
- bowel wall thickening
- alteration of the vascular state
- hypervascular (viable but engorged in early stage)
- hypovascular (infarcted in a later stage)
- intramural gas manifesting as hyperechoic foci within the bowel wall
- free fluid, especially with echogenic debris, suggests perforation
Treatment and prognosis
NEC can be managed both medically and surgically and appropriate patient selection is essential in optimizing outcome. A clinical staging system has been developed (see necrotizing enterocolitis staging), with stage I and II receiving medical therapy and stage III undergoing surgery .
Medical management consists of supportive measures and cessation of oral feeding, along with broad-spectrum antibiotics and gastric aspiration .
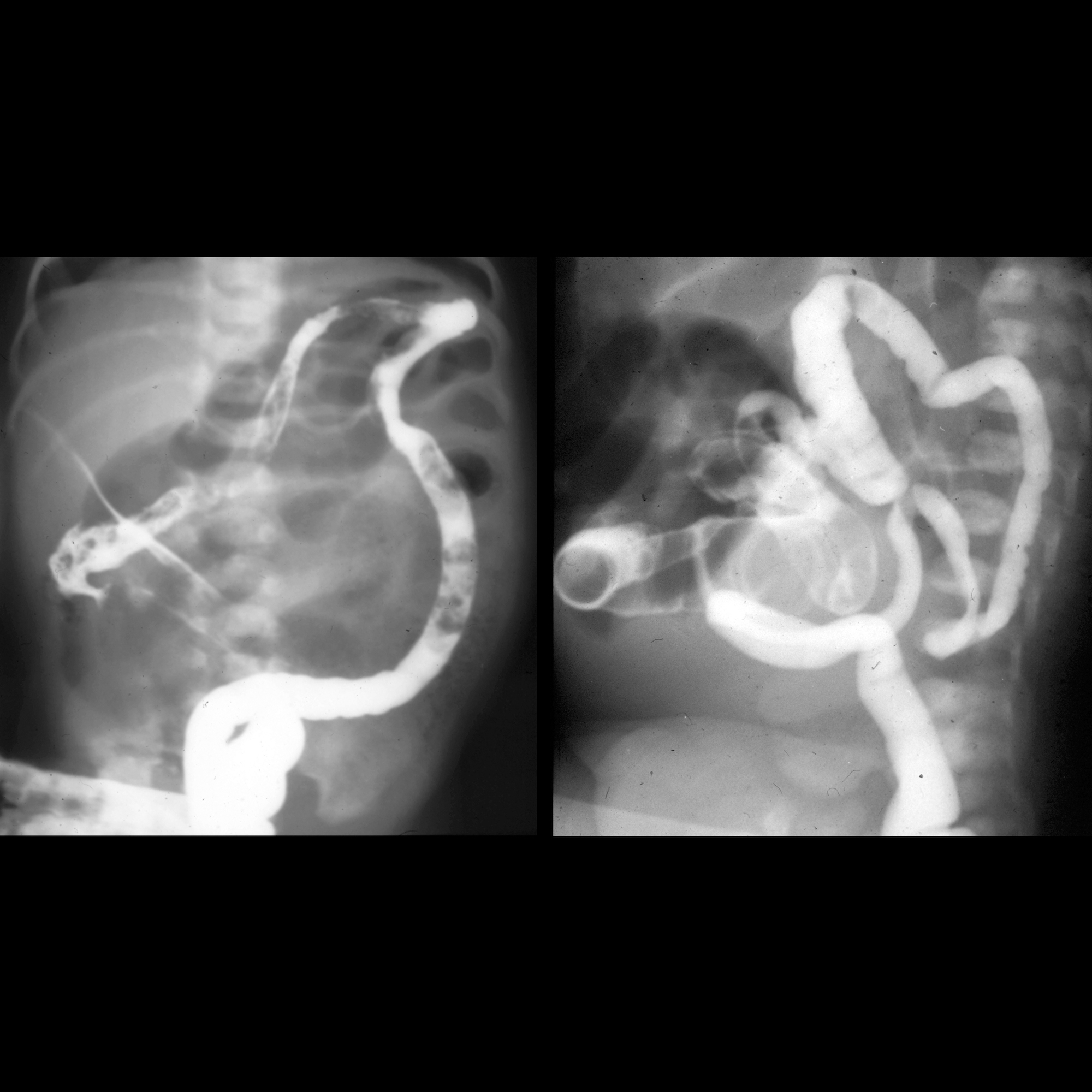
Surgery is usually reserved for patients with evidence of perforation and entails resection of clearly necrotic bowel and the creation of a proximal enterostomy . Other relative indications for surgery include portal venous gas, a fixed dilated loop on serial x-rays and abdominal wall erythema . Re-anastomosis is usually delayed until the infant has completely recovered.
Despite therapy, mortality remains significant, ranging between 9 and 28% . Furthermore ~20% of surviving patients will go on to develop stricture. These are more common in the large bowel (80%) and may result in bowel obstruction weeks to months later .
Differential diagnosis
In the correct clinical scenario, the presence of gas within bowel wall has a little differential.
Conditions worth keeping in mind include :
- pneumatosis coli
- neonatal appendicitis
- meconium ileus
- Hirschsprung disease
- infectious enterocolitis
- Fokale Intestinale Perforation (FIP)
Siehe auch:
- Fokale Intestinale Perforation (FIP)
- Pneumatosis intestinalis
- Mekoniumileus
- Pneumatosis coli
- Morbus Hirschsprung
- intramurale Gaseinschlüsse
- Pneumoperitoneum beim Neugeborenen
- neonatal appendicitis
- necrotising enterocolitis staging
und weiter:
- Pneumoperitoneum
- portalvenöses Gas
- football sign
- neonatal bilious vomiting
- Pneumatosis cystoides des Kolons
- ischämische Kolitis
- Gas im Pfortadersystem beim Neugeborenen
- Gas im Pfortadersystem bei nekrotisierender Enterokolitis
- Nekrose
- spontane intestinale Perforation
- Enterokolitis
- Enterokolitis bei Morbus Hirschsprung

 Assoziationen und Differentialdiagnosen zu Nekrotisierende Enterokolitis:
Assoziationen und Differentialdiagnosen zu Nekrotisierende Enterokolitis: