Ovarialtorsion bei Ovarialfibrom













Ovarialtorsion bei Ovarialfibrom
Ovarialtorsion Radiopaedia • CC-by-nc-sa 3.0 • de
Ovarian torsion, also sometimes termed adnexal torsion or tubo-ovarian torsion, refers to rotation of the ovary and portion of the fallopian tube on the supplying vascular pedicle.
It can be intermittent or sustained and results in venous, arterial and lymphatic stasis. It is a gynecological emergency and requires urgent surgical intervention to prevent ovarian necrosis.
Epidemiology
Ovarian torsion has a bimodal age distribution occurring mainly in young women (15-30 years) and post-menopausal women. Approximately 20% of the cases occur during pregnancy .
Torsion occurs due to two main reasons :
- hypermobility of the ovary: <50%
- adnexal mass: ~50-80%
- most lesions are dermoid cysts or paraovarian cysts
- large cystic ovaries undergoing ovarian hyperstimulation are at particular risk
- masses between 5-10 cm are at most risk
Clinical presentation
Most patients present with severe non-specific lower abdominal and pelvic pain, either intermittent or sustained, nausea, and vomiting. There is an adnexal tenderness. A raised white cell count is common.
Pathology
The result of vascular compromise secondary to ovarian torsion is hemorrhagic infarction and necrosis, that can occur as rapidly as within hours of torsion onset.
Torsion of a normal ovary more commonly occurs in young children when developmental abnormalities predispose the ovary to torsions, such as excessively long Fallopian tubes or an absent mesosalpinx.
In adulthood, causes include both benign and malignant ovarian tumors, polycystic ovaries and adhesions. In early pregnancy, a torsion can occur secondary to a corpus luteal cyst or laxity of the adjacent tissues.
Radiographic features
The main feature of torsion is ovarian enlargement due to venous/lymphatic engorgement, edema, and hemorrhage. Secondary signs include free pelvic fluid, an underlying ovarian lesion, reduced or absent vascularity and a twisted dilated tubular structure corresponding to the vascular pedicle. Adnexal torsion is commonly unilateral, with a slight (3:2) right-sided predilection (presumably due to the protective effects of the sigmoid colon on the left) .
Ultrasound
Ultrasound is the initial imaging modality of choice. Sonographic features include
- enlarged (>4 cm) ovary
- variable echogenicity (hypo- or hyperechoic)
- a long-standing infarcted ovary may have a more complex appearance with cystic or hemorrhagic degeneration
- peripherally displaced follicles with hyperechoic central stroma
- midline ovary position
- free pelvic fluid may be seen in >80% of cases
- an underlying ovarian lesion may be seen (possible lead point for torsion)
- Doppler findings in torsion are widely variable
- little or no ovarian venous flow (common; sensitivity of 100% and specificity of 97%)
- absent arterial flow (a less common, sign of poor prognosis)
- absent or reversed diastolic flow
- normal vascularity does not rule out intermittent torsion
- normal Doppler flow can also occasionally be found due to dual supply from both the ovarian and uterine arteries
- whirlpool sign of twisted vascular pedicle
- ovary tenderness to transducer pressure
- follicular ring sign16
CT
- good at ruling out ovarian torsion if a normal ovary/adnexa is seen on ultrasound
- the twisted ovarian pedicle is pathognomonic for ovarian torsion if demonstrated
- torsion appears as a complex adnexal lesion representing
- enlarged ovary (>4.0 cm )
- distended pedicle
- possible underlying ovarian lesion
- HU >50 on non-contrast CT suggests hemorrhagic necrosis
- lack of enhancement may be seen
- surrounding fat stranding, edema, and free fluid
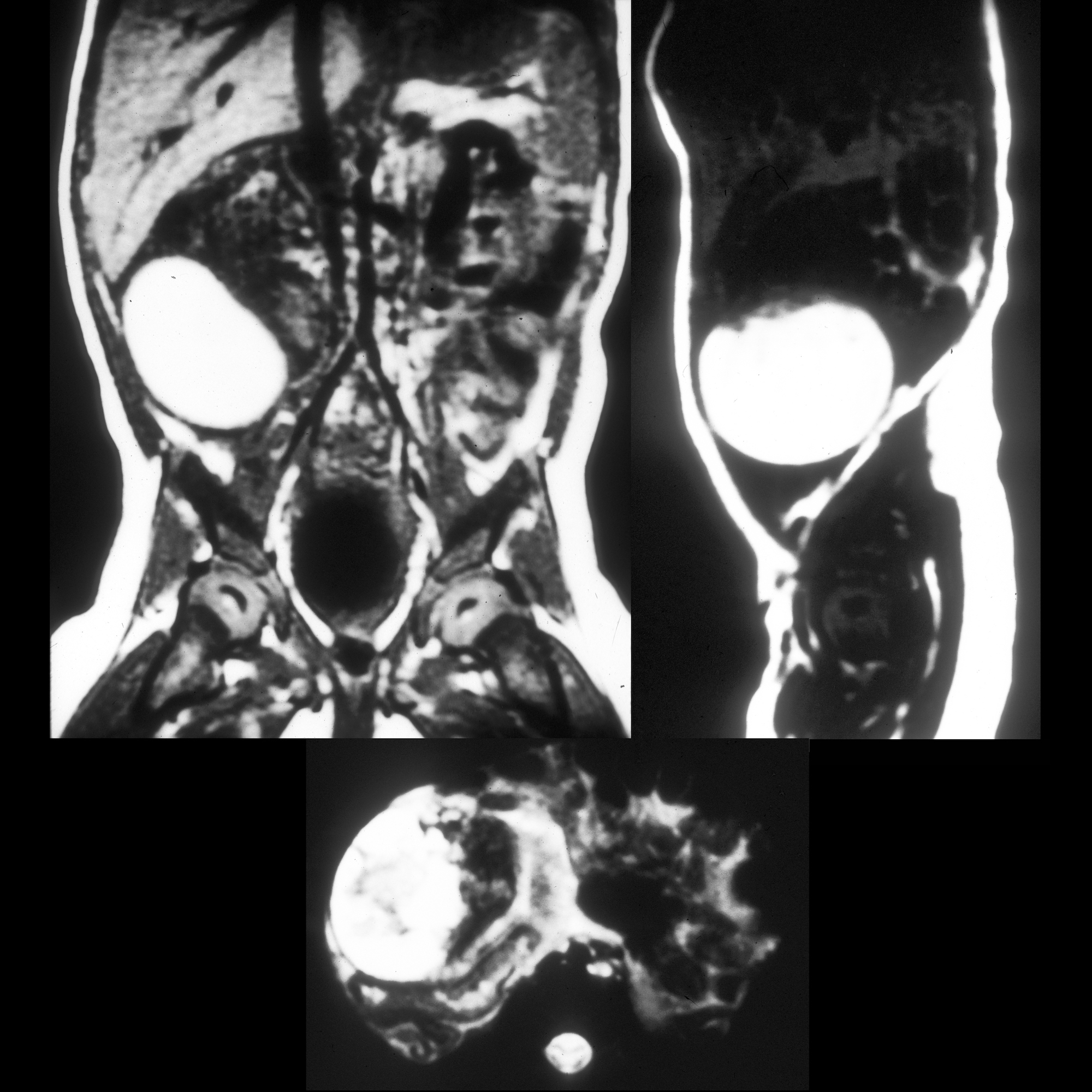
MRI
Not the imaging modality of choice if torsion is suspected, as urgent imaging is required.
If hemorrhagic infarction is present, signal changes include :
- T1
- thin rim of high signal (methemoglobin) without contrast enhancement
- endometriomas and hemorrhagic corpus luteal cysts are less likely to have a high T1 rim and do not usually involve the entire ovary
- T2: can have low signal due to interstitial hemorrhage
Treatment and prognosis
Urgent surgery is required to prevent ovarian necrosis. Most ovaries are not salvageable, in which case a salpingo-oophorectomy is required. If not removed, the necrotic ovary can become infected and cause an abscess or peritonitis. In the case of a non-infarcted adnexa, surgical untwisting can be performed. Mortality resulting from ovarian torsion is rare. Spontaneous detorsion has also been reported.
Differential diagnosis
For an enlarged edematous ovary +/- Fallopian tube, consider:
- pelvic inflammatory disease (PID): has a very different clinical presentation
- massive ovarian edema (MOO)
- oophoritis
Practical points
- the ovary should be tender to transducer pressure
- absence of ovarian Doppler flow is highly specific for torsion, but normal Doppler flow does not completely rule out torsion
- an ovarian mass causing the torsion must always be sought
Ovarialfibrom Radiopaedia • CC-by-nc-sa 3.0 • de
Ovarian fibromas are a benign ovarian tumor of sex cord / stromal origin. Although fibromas account for ~4% of all ovarian neoplasms, they are the most common sex cord ovarian tumor.
Epidemiology
Fibromas occur at all ages but are most frequently seen in middle-aged women.
Clinical presentation
Fibromas are generally asymptomatic and are often detected at palpation during a routine gynecologic examination. Tumors can reach a large size at presentation.
Pathology
The tumor belongs to the same histopathologic spectrum as an ovarian thecoma / ovarian fibrothecoma. Fibromas have no (or very few) thecal cells and no (or minimal) estrogen activity.
It is composed of spindle cells forming variable amounts of collagen. Sectioning of a fibroma typically reveals a chalky-white surface that has a whorled appearance, similar to that of a uterine fibroid. Areas of edema, occasionally with cyst formation, are also relatively common.
Associations
They are associated with ascites in 40% of cases and with pleural effusions in a small percentage of cases.
- Meigs syndrome: consists of ovarian fibroma with ascites and a pleural effusion
- fibromas are seen in 75% of patients with nevoid basal cell carcinoma syndrome
Radiographic features
Ultrasound
On ultrasound, fibromas most commonly manifest as solid, hypoechoic masses with ultrasound beam attenuation. As such, they may appear similar to a pedunculated subserosal uterine fibroid.
However, the sonographic appearance can be variable, and some tumors can rarely have cystic components.
CT
Fibromas usually manifest as diffuse, slightly hypoattenuating masses with poor, very slow contrast enhancement. Calcification and bilaterality are both uncommon.
MRI
Signal characteristics include:
- T1: fibromas usually demonstrate homogeneous low signal intensity
- T2
- fibromas appear as well-circumscribed masses with low signal intensity
- may contain scattered hyperintense areas representing edema or cystic degeneration
- a band of T2 hypointensity separating the tumor from the uterus on all imaging planes is also considered a characteristic feature
- T1 C+ (Gd): usually shows heterogeneous enhancement
Treatment and prognosis
Ovarian fibromas are almost always benign .
Complications
Differential diagnosis
General imaging differential considerations include:
- large pedunculated subserosal uterine leiomyoma
- thecoma and fibrothecoma
- tend to have brighter signal on T2 given edema and cystic degeneration
- contrast-enhancement may be observed given the vascularization of the theca cells
 Assoziationen und Differentialdiagnosen zu Ovarialtorsion bei Ovarialfibrom:
Assoziationen und Differentialdiagnosen zu Ovarialtorsion bei Ovarialfibrom: