Scaphoidfraktur

































Scaphoid fractures (i.e. fractures through the scaphoid bone) are common, in some instances can be difficult to diagnose, and can result in significant functional impairment.
Epidemiology
Scaphoid fractures account for 70-80% of all carpal bone fractures . Although they occur essentially at any age, adolescents and young adults are most commonly affected . Older patients falling in a similar manner are more likely to sustain a distal radial fracture (usually a Colles fracture).
Clinical presentation
Classically there can be a pain in anatomical snuffbox which is thought to have a sensitivity of ~90% and a specificity of ~40% .
Pathology
The usual mechanism is falling on an outstretched hand with resultant hyperextension of the wrist or purely compressive force . Occasionally stress fractures are also encountered although these are less common, and only usually seen in athletes (e.g. shot putters or gymnasts) .
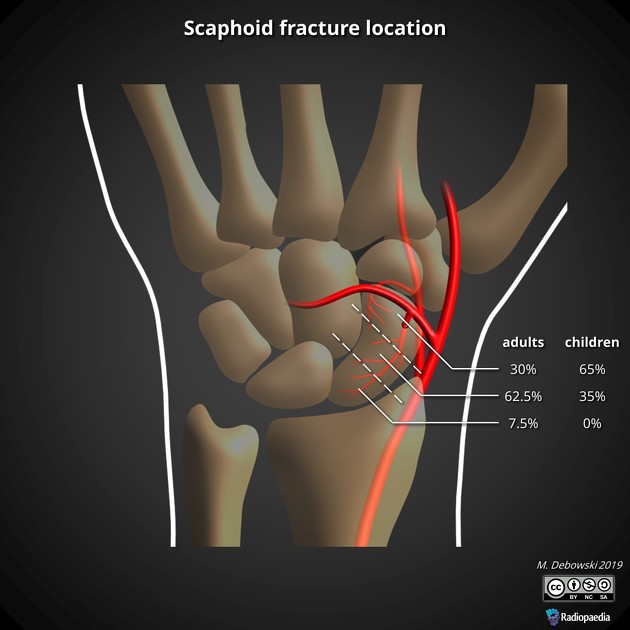
Fractures can occur essentially anywhere along the scaphoid, but distribution is not even :
- waist of the scaphoid: 70-80%
- distal pole (or so-called scaphoid tubercle): 20%
- proximal pole: 10%
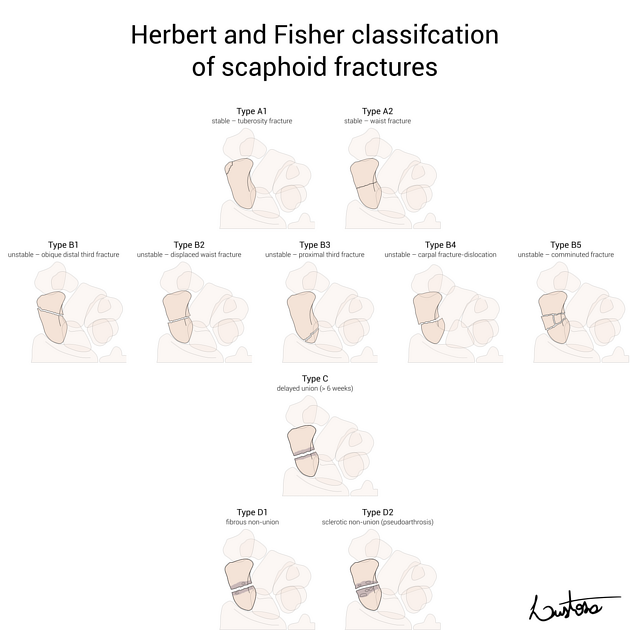
Classification
See: Mayo classification of scaphoid fractures.
Radiographic features
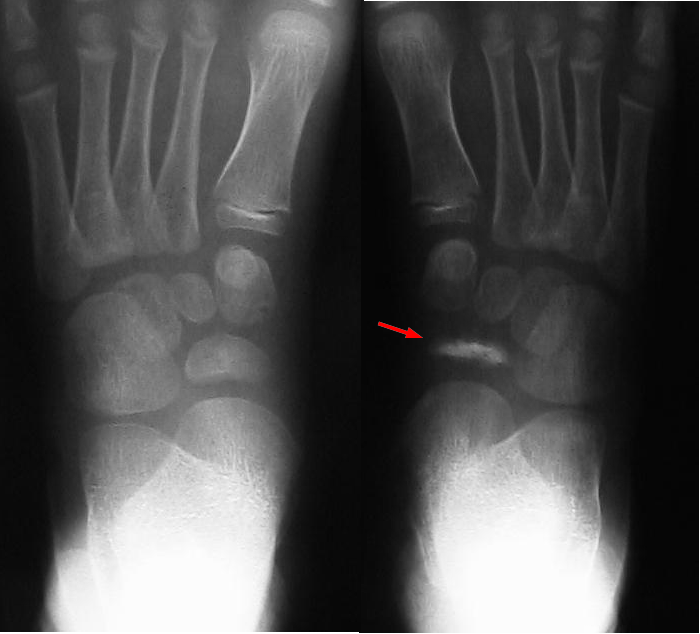
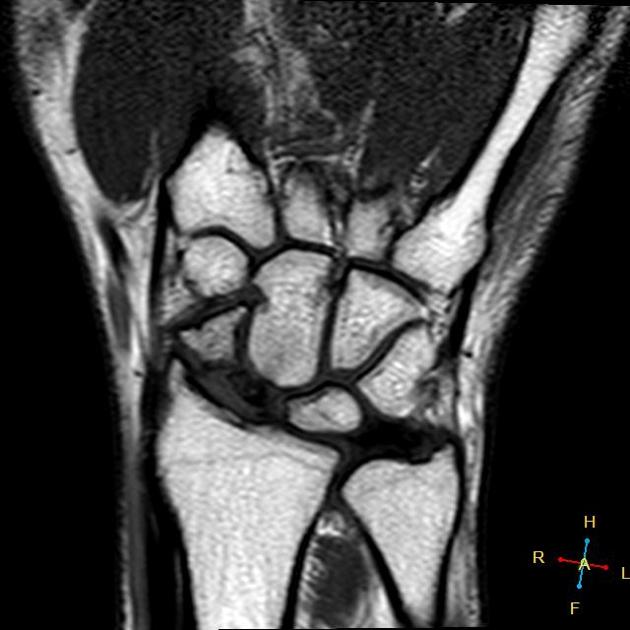
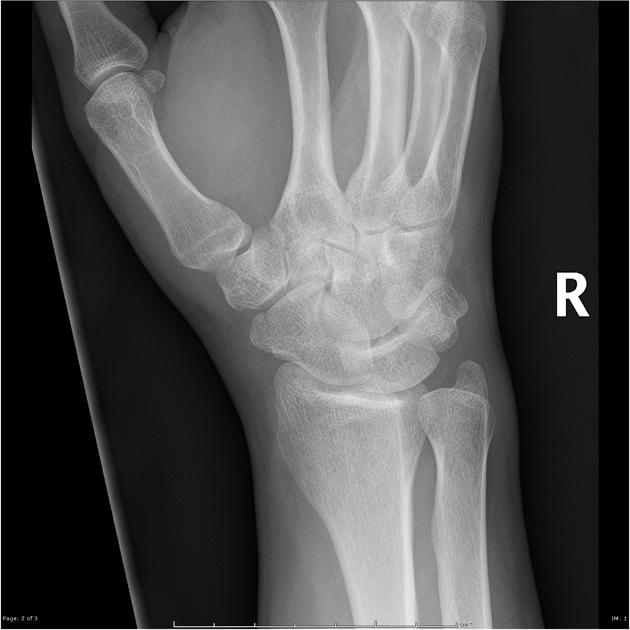
Plain radiograph
A dedicated plain radiographic series investigating the scaphoid exists, consisting of four projections of the scaphoid bone. It is positionally different from the wrist series. It should, however, be noted that the initial radiograph can miss from 5-20% of fractures in the acute setting .
Features include:
- visualization of the fracture +/- displacement
- soft tissue swelling and lateral displacement of the adjacent fat pads
- scaphoid fat pad sign: obliteration or lateral displacement of a straight/convex lucent line on the lateral aspect of the scaphoid
- associated scapholunate ligament disruption (Terry Thomas sign) which can be accentuated with a clenched fist view
If AVN develops the first sign will be slight sclerosis. This can be on account of the rest of the wrist undergoing demineralization due to immobilization, whereas the proximal portion being bereft of blood supply retains its calcium. With time the proximal part undergoes osteonecrosis, becomes increasingly sclerotic and can 'implode' and fragment with secondary osteoarthritic changes .
Report checklist
In addition to stating that a fracture is present, a number of features should be sought and commented upon:
- fracture
- location (distal pole, waist, proximal pole)
- involvement of articular surfaces
- displacement or step
- humpback deformity due to angulation between proximal and distal parts
- alignment
- scapholunate interval
- lunate dislocation (trans-scaphoid perilunate dislocation)
- associated fractures (e.g. Colles fracture or other carpal bone fractures)
- evidence of avascular necrosis if the fracture is subacute
Importantly if no fracture is seen it is essential to recommend repeat x-rays (including dedicated scaphoid views) in 7-10 days . If these repeat films are negative also, then MRI (or bone scan if MRI is unavailable) should be recommended if clinical suspicion persists .
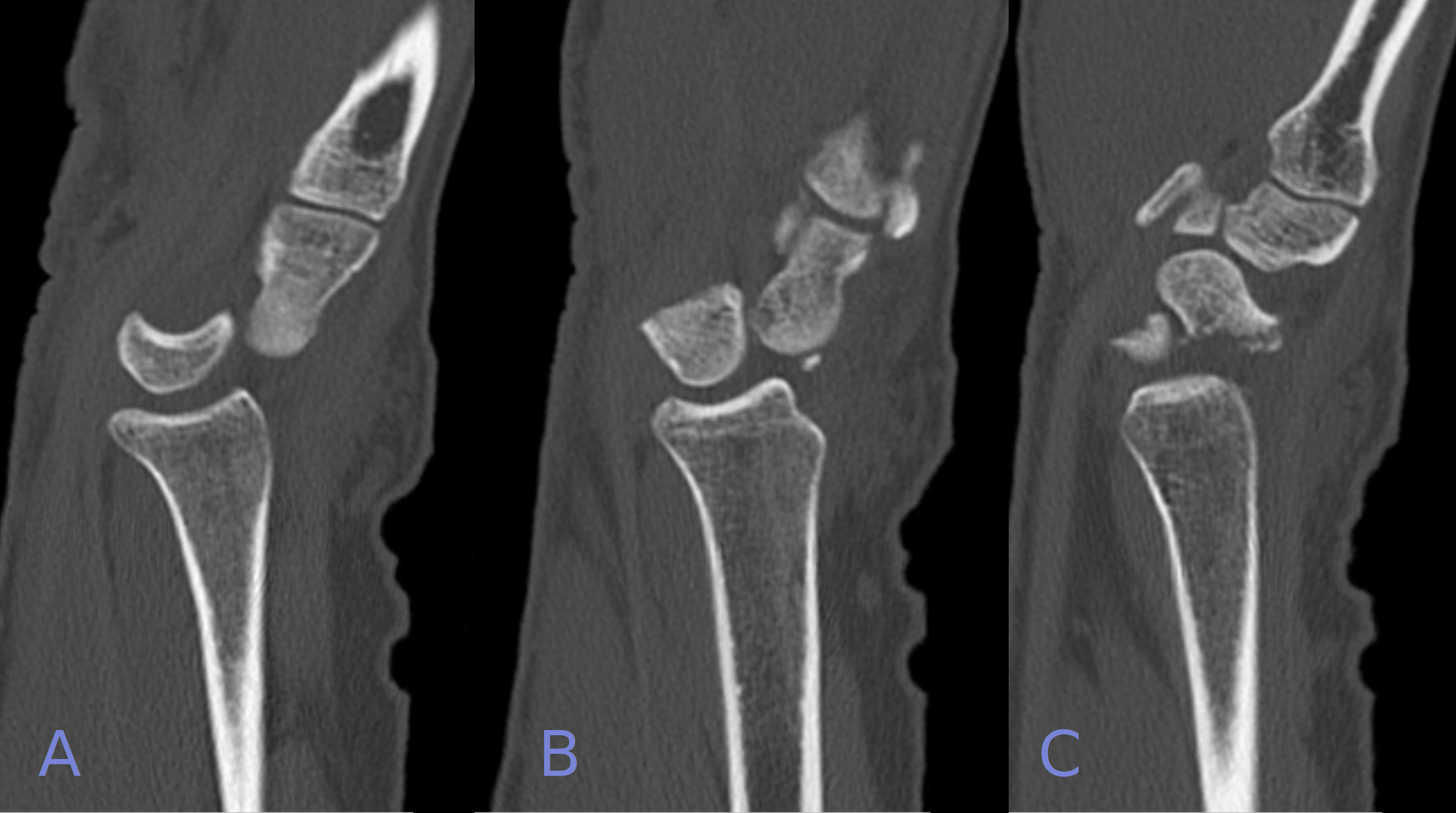
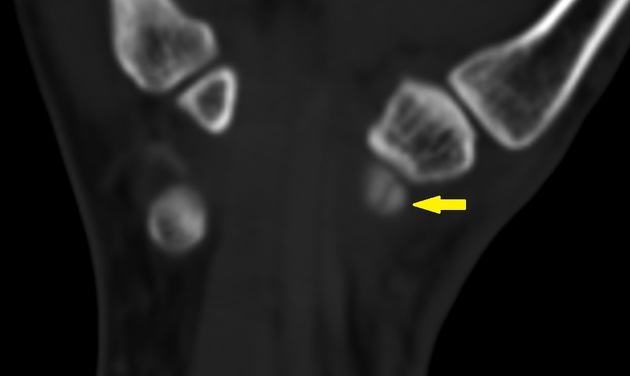
CT
CT may be used for diagnosis when plain films are normal because it is readily available and quick . Reported sensitivities, specificities and negative predictive values for CT have been reported CT to be 89-90%, 85-100%, and 97-98% respectively. CT may be insensitive to trabecular injury . CT is useful for staging scaphoid fractures if surgery is considered and when fractures of the carpus are extensive or complex. CT also is useful in assessing bone union .
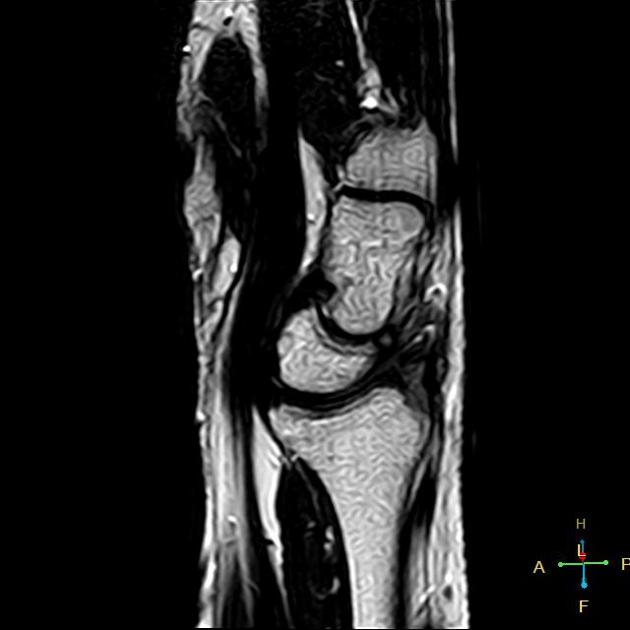
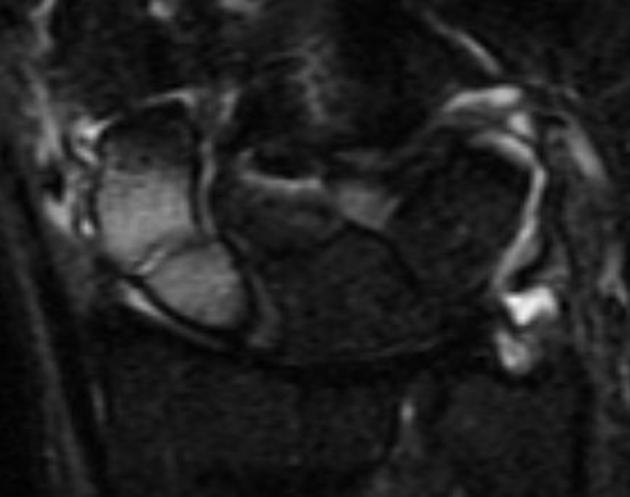
MRI
MRI is the most sensitive modality for trabecular fractures, and this can detect completely undisplaced fractures, especially in the first 24 hours following injury . It is also useful in assessing for avascular necrosis.
Nuclear medicine
Although bone scans are more sensitive than plain radiograph, they are usually reserved for patients with ongoing pain despite normal serial plain films . Bone scans will be most sensitive 3-4 days following the injury. An occult fracture will appear as a region of increased uptake, whereas avascular necrosis will demonstrate a photopenic region at the lower pole of the scaphoid.
Treatment and prognosis
Management options can broadly be divided into:
- immobilization with cast application
- internal fixation for >2 mm displaced fragments, usually with a headless self-compressing screw
- non-union can be managed with internal fixation and bone grafting
Non-union occurs in 5-15% of cases . Factors affecting prognosis:
- location
- distal pole: the excellent likelihood of union (~100%)
- waist: ~10-20% chance of non-union
- proximal pole: ~30-40% chance of non-union
- vertically oriented fracture line
- fragment displacement of >1 mm
- ligamentous instability: increased scapholunate angle (i.e. >60º or radiolunate or capitolunate angle >15º
Complications
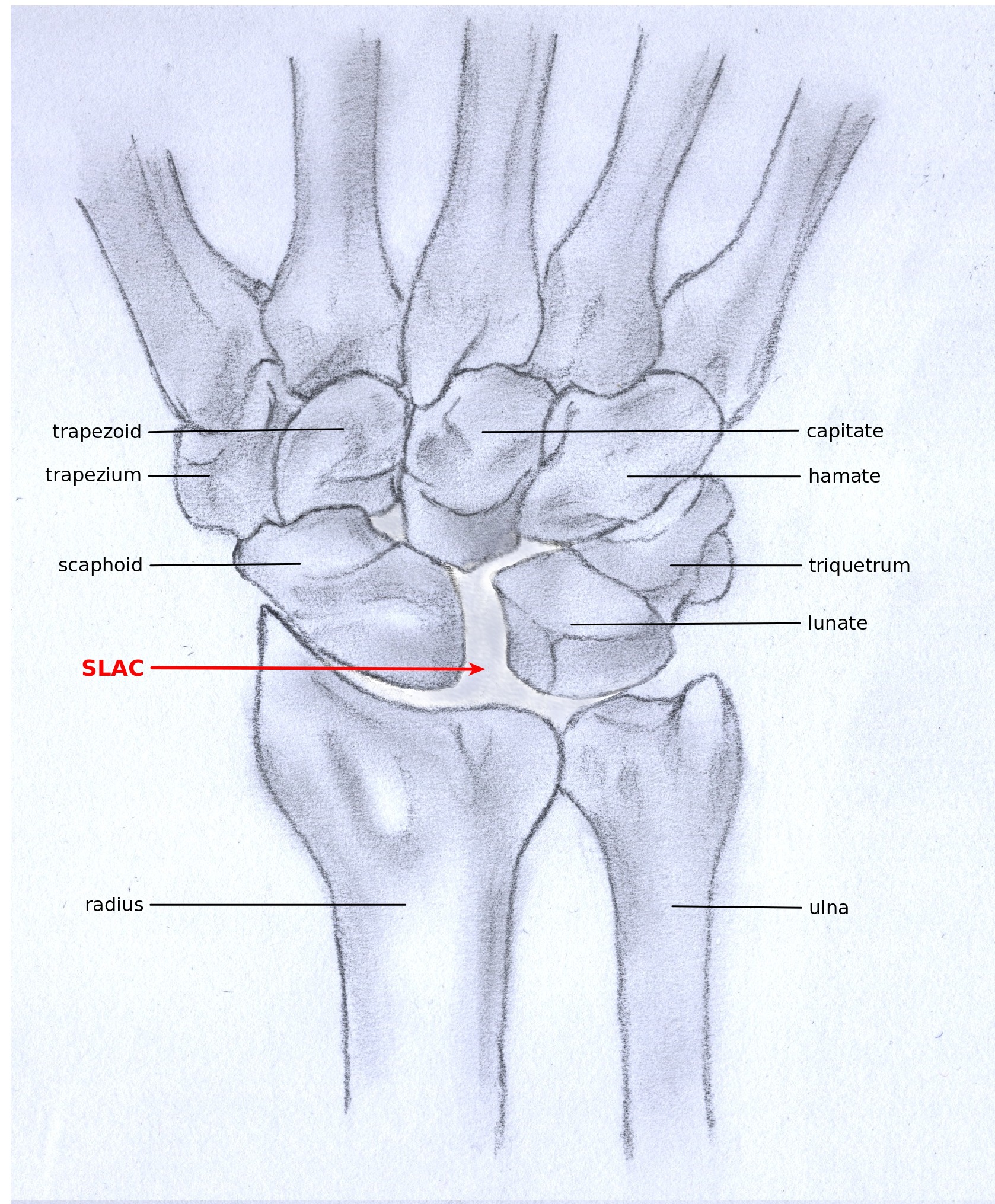
The major complication of scaphoid fractures is non-union or malunion leading to instability and secondary osteoarthritic change. Hence surgical treatment of displaced fractures or angulation.
A number of other specific complications are encountered from time to time:
- avascular necrosis in ~30% (range 13-50%)
- this most commonly involves the proximal portion as a result of arterial supply to the scaphoid entering distally
- note Preiser disease is the term used for non-traumatic avascular necrosis
- SNAC wrist: scaphoid non-union advanced collapse
- SLAC wrist: scapholunate advanced collapse
History and etymology
The term scaphoid derives from the Greek word for boat. The bone profile is thought to look like a boat or skiff.
Siehe auch:
- Aseptische Knochennekrose
- Colles-Fraktur
- Terry-Thomas sign
- perilunäre Luxation
- Morbus Köhler I
- scaphoid non-union advanced collapse
- distale Radiusfraktur
- scapholunate advanced collapse (SLAC)
- anatomical snuffbox
- Scaphoidpseudarthrose
- Mayo-Klassifikation Scaphoidfraktur
- Scaphoidfraktur Klassifizierung nach Russe
- Scaphoidfraktur Klassifikation nach Watson-Jones
- Klassifikation Scaphoidfrakturen nach Schernberg und Elzein
- humpback deformity
- Os scaphoideum
und weiter:
- DISI-Fehlstellung
- scapholunärer Winkel
- Frakturen der oberen Extremitäten
- anatomical snuff box
- fall onto an outstretched hand
- Frakturen der Handwurzelknochen
- bone infarct of the scaphoid
- radiologisches muskuloskelettales Curriculum
- occult scaphoid fracture
- Scaphoidfraktur Nekrose
- ipsilateral fractures of distal radius, scaphoid and capitate
- scaphoid fissure
- scaphoid tubercle fracture
- distal scaphoid fracture
- sclerotic proximal pole scaphoid post fracture

 Assoziationen und Differentialdiagnosen zu Scaphoidfraktur:
Assoziationen und Differentialdiagnosen zu Scaphoidfraktur: